Abstract
Purpose
To compare loop gain (LG) before and during pharmacological increases in cerebral blood flow (CBF) at high altitude (HA). Loop gain (LG) describes stability of a negative-feedback control system; defining the magnitude of response to a disturbance, such as hyperpnea to an apnea in periodic breathing (PB). “Controller-gain” sensitivity from afferent peripheral (PCR) and central-chemoreceptors (CCR) plays a key role in perpetuating PB. Changes in CBF may have a critical role via effects on central chemo-sensitivity during sleep.
Methods
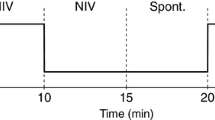
Polysomnography (PSG) was performed on volunteers after administration of I.V. Acetazolamide (ACZ-10mg/kg) + Dobutamine (DOB-2–5 μg/kg/min) to increase CBF (via Duplex-ultrasound). Central sleep apnea (CSA) was measured from NREM sleep. The duty ratio (DR) was calculated as ventilatory duration (s) divided by cycle duration (s) (hyperpnea/hyperpnea + apnea), LG = 2π/(2πDR-sin2πDR).
Results
A total of 11 volunteers were studied. Compared to placebo-control, ACZ/DOB showed a significant increase in the DR (0.79 ± 0.21 vs 0.52 ± 0.03, P = 0.002) and reduction in LG (1.90 ± 0.23 vs 1.29 ± 0.35, P = 0.0004). ACZ/DOB increased cardiac output (CO) (8.19 ± 2.06 vs 6.58 ± 1.56L/min, P = 0.02) and CBF (718 ± 120 vs 526 ± 110ml/min, P < 0.001). There was no significant change in arterial blood gases, minute ventilation (VE), or hypoxic ventilatory response (HVR). However, there was a reduction of hypercapnic ventilatory response (HCVR) by 29% (5.9 ± 2.7 vs 4.2 ± 2.8 L/min, P = 0.1).
Conclusion
Pharmacological elevation in CBF significantly reduced LG and severity of CSA. We speculate the effect was on HCVR “controller gain,” rather than “plant gain,” because PaCO2 and VE were unchanged. An effect via reduced circulation time is unlikely, as the respiratory-cycle length did not change.




Similar content being viewed by others
Data availability
All data that support the findings of this study are available within the paper.
Abbreviations
- ABG:
-
Arterial blood gas
- ACZ:
-
Acetazolamide
- AHI:
-
Apnea-hypopnea index
- AMS:
-
Acute mountain sickness
- BC:
-
British Columbia
- BMI:
-
Body mass index
- CA:
-
Carbonic anhydrase
- CBF:
-
Cerebral blood flow
- CBFv:
-
Cerebral blood flow velocity
- CCR:
-
Central chemoreceptors
- CO2:
-
Carbon dioxide
- CO:
-
Cardiac output
- CSA:
-
Central sleep apnea
- CSF:
-
Cerebrospinal fluid
- DOB:
-
Dobutamine
- DR:
-
Duty ratio
- EEG:
-
Electroencephalogram
- EMG:
-
Electromyography
- EOG:
-
Electrooculography
- HA:
-
High altitude
- HVR:
-
Hypoxic ventilatory response
- HCVR:
-
Hypercapnic ventilatory response
- HR:
-
Heart rate
- I.V.:
-
Intravenous
- LG:
-
Loop gain
- PB:
-
Periodic breathing
- PCR:
-
Peripheral chemoreceptors
- PSG:
-
Polysomnography
- VA:
-
Vertebral artery
- VE:
-
Minute ventilation
References
Eckert DJ et al (2007) Central sleep apnea: pathophysiology and treatment. Chest 131(2):595–607
Ainslie PN, Burgess KR (2017) Chapter 18 - respiratory physiology: sleep at high altitudes, In Principles and Practice of Sleep Medicine (Sixth Edition), Kryger M, Roth T, Dement WC (eds.), Elsevier. p. 182–192.e4
San T et al (2013) Effects of high altitude on sleep and respiratory system and their adaptations. ScientificWorldJournal 2013:241569
Dempsey JA (2005) Crossing the apnoeic threshold: causes and consequences. Exp Physiol 90(1):13–24
Burgess KR et al (2014) Influence of cerebral blood flow on central sleep apnea at high altitude. Sleep 37(10):1679–1687
Khoo MC et al (1982) Factors inducing periodic breathing in humans: a general model. J Appl Physiol Respir Environ Exerc Physiol 53(3):644–659
Nemati S et al (2011) Model-based characterization of ventilatory stability using spontaneous breathing. J Appl Physiol 111(1):55–67
Edwards BA et al (2009) Maturation of respiratory control and the propensity for breathing instability in a sheep model. J Appl Physiol 107(5):1463–1471
Topor Z, Vasilakos K, Remmers J (2004) Interaction of two chemoreflex loops in determining ventilatory stability. Nonlinear Studies 11(8):527–541
Cherniack NS, Longobardo GS (2006) Mathematical models of periodic breathing and their usefulness in understanding cardiovascular and respiratory disorders. Exp Physiol 91(2):295–305
Nattie E, Li A (2012) Central chemoreceptors: locations and functions. Compr Physiol 2(1):221–254
Ainslie PN, Duffin J (2009) Integration of cerebrovascular CO2 reactivity and chemoreflex control of breathing: mechanisms of regulation, measurement, and interpretation. Am J Physiol Regul Integr Comp Physiol 296(5):R1473–R1495
Burgess KR et al (2018) Increasing cerebral blood flow reduces the severity of central sleep apnea at high altitude. J Appl Physiol 124(5):1341–1348
Sands SA et al (2016) Control theory prediction of resolved Cheyne−Stokes respiration in heart failure. Eur Respir J 48(5):1351–1359
Fan JL et al (2012) Effects of acetazolamide on cerebrovascular function and breathing stability at 5050 m. J Physiol 590(5):1213–1225
Ritschel WA et al (1998) Pharmacokinetics of acetazolamide in healthy volunteers after short- and long-term exposure to high altitude. J Clin Pharmacol 38(6):533–539
Swenson ER, Hughes JM (1993) Effects of acute and chronic acetazolamide on resting ventilation and ventilatory responses in men. J Appl Physiol (1985) 74(1):230–7
Klem GH et al (1999) The ten-twenty electrode system of the International Federation. The International Federation of Clinical Neurophysiology. Electroencephalogr Clin Neurophysiol Suppl 52:3–6
Berry RB et al (2017) AASM Scoring Manual Updates for 2017 (Version 24). J Clin Sleep Med 13(05):665–666
Rechtschaffen A (1968) K.A editors, A manual of standardized terminology, techniques and scoring system of sleep stages in human subjects. Brain Information Service/Brain Research Institute, University of California
Vorstrup S, Henriksen L, Paulson OB (1984) Effect of acetazolamide on cerebral blood flow and cerebral metabolic rate for oxygen. J Clin Invest 74(5):1634–1639
Hauge A, Nicolaysen G, Thoresen M (1983) Acute effects of acetazolamide on cerbral blood flow in man. Acta Physiol Scand 117(2):233–239
Wesseling KH et al (1993) Computation of aortic flow from pressure in humans using a nonlinear, three-element model. J Appl Physiol (1985) 74(5):2566–73
Bärtsch P, Gibbs JSR (2007) Effect of altitude on the heart and the lungs. Circulation 116(19):2191–2202
Naughton M et al (1993) Role of hyperventilation in the pathogenesis of central sleep apneas in patients with congestive heart failure. Am Rev Respir Dis 148(2):330–338
Iturriaga R, Mokashi A, Lahiri S (1993) Dynamics of carotid body responses in vitro in the presence of CO2-HCO3-: role of carbonic anhydrase. J Appl Physiol 75(4):1587–1594
Teppema LJ, Dahan A (1999) Acetazolamide and breathing. Does a clinical dose alter peripheral and central CO(2) sensitivity? Am J Respir Crit Care Med 160(5 Pt 1):1592–7
Xie A et al (2009) Influence of cerebral blood flow on breathing stability. J Appl Physiol (1985) 106(3):850–6
Naughton MT (1998) Pathophysiology and treatment of Cheyne-Stokes respiration. Thorax 53(6):514–518
Acknowledgements
This study was carried out within the framework of the Ev-K2-CNR Project in collaboration with the Nepal Academy of Science and Technology as foreseen by the Memorandum of Understanding between Nepal and Italy. Thanks to contributions from the Italian National Research Council and the Italian Ministry of Foreign Affairs. We extend thanks to ADInstruments and Compumedics Ltd. for the use of their laboratory equipment.
Funding
The Peninsula Health Care p/l provided non-financial support on the form of equipment loan. NSERC provided financial support of in the form of a grant. CRC provided financial support in the form of funding for travel and consumables. Lottery Health NZ and the University of Otago provided financial support in the form of travel funding and salary (SJEL). The sponsors had no role in the design or conduct of the research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee (University of British Columbia Ethics Committee and the Nepal Health Medical Research Council) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in this study.
Disclosure of the presence or absence of financial support and off-label or investigational use
Intravenous acetazolamide use was off-label.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Summary at a glance
Intravenous administration of Acetazolamide and Dobutamine significantly reduced loop gain and the severity of central sleep apnea. The effect was most likely on the “controller gain.”.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Burgess, A., Andrews, G., Colby, K.M.E. et al. Loop gain response to increased cerebral blood flow at high altitude. Sleep Breath (2023). https://doi.org/10.1007/s11325-023-02956-4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11325-023-02956-4