Abstract
Purpose
This study aimed to examine the relationship between plasma metabolites (biochemical parameters) and comorbid illnesses with sleep quality in individuals with coronary heart disease (CHD).
Methods
This descriptive cross-sectional study was conducted between 2020 and 2021 at a university hospital. Hospitalized patients with a diagnosis of CHD were analyzed. The Personal Information Form' and Pittsburgh Sleep Quality Index (PSQI) were used to collect data. Laboratory findings including plasma metabolites were examined.
Results
Of 60 hospitalized patients with CHD, 50 (83%) had poor sleep quality. A positive and statistically significant correlation was found between the plasma metabolite blood urea nitrogen and poor sleep quality (r = 0.399; p = 0.002). The presence of CHD and additional chronic diseases (especially diabetes mellitus, hypertension, and chronic kidney disease) are important parameters associated with the risk of poor sleep quality (p = 0.040 < 0.05).
Conclusion
Increases in blood urea nitrogen level in individuals with CHD are associated with worse sleep quality. Additional chronic diseases coexisting with CHD correlate with increased risk of poor sleep quality.
Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available (The patients participating in the study were informed that the data would not be shared) but are available from the corresponding author on reasonable request.
References
Matthews KA, Strollo PJ Jr, Hall M et al (2011) Associations of Framingham risk score profile and coronary artery calcification with sleep characteristics in middle-aged men and women: Pittsburgh SleepSCORE study. Sleep 34(6):711–716. https://doi.org/10.5665/SLEEP.1032
Tenekeci EG, Kara B (2016) The relationship between sleep quality and fatigue in individuals with myocardial infarction. Gulhane Med. J 58(4):366. https://doi.org/10.5455/gulhane.210780
World Health Organization. Cardiovascular diseases (CVDs) fact sheet. https://www.who.int/en/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds). Accessed 30 Jun 2022
Kara B (2012) Sleep Problems Before and after acute myocardial infarction: a comparative study. TAF Prev Med Bull 11(6):687–694. https://doi.org/10.5455/pmb.1326922971
Johansson I, Karlson BW, Grankvist G et al (2010) Disturbed sleep, fatigue, anxiety and depression in myocardial infarction patients. Eur J Cardiovasc Nurs 9(3):175–180. https://doi.org/10.1016/j.ejcnurse.2009.12.003
Covassin N, Singh P (2016) Sleep duration and cardiovascular disease risk: epidemiologic and experimental evidence. Sleep Med Clin 11(1):81–89. https://doi.org/10.1016/j.jsmc.2015.10.007
Whitesell PL, Obi J, Tamanna NS et al (2018) A review of the literature regarding sleep and cardiometabolic disease in african descent populations. Front Endocrinol (Lausanne) 11(9):140. https://doi.org/10.3389/fendo.2018.00140
St-Onge MP, Grandner MA, Brown D et al (2016) Sleep duration and quality: impact on lifestyle behaviors and cardiometabolic health: a scientific statement from the American Heart Association. Circulation 134(18):e386. https://doi.org/10.1161/CIR.0000000000000444
Hoevenaar-Blom MP, Spijkerman AM, Kromhout D et al (2014) Sufficient sleep duration contributes to lower cardiovascular disease risk in addition to four traditional lifestyle factors: the MORGEN study. Eur J Prev Cardiol 21(11):1367–1375. https://doi.org/10.1177/2047487313493057
Berger S, Aronson D, Lavie P et al (2013) Endothelial progenitor cells in acute myocardial infarction and sleep disordered breathing. Am J Respir Crit Care Med 187:90–98
Javaheri S, Redline S (2017) Insomnia and risk of cardiovascular disease. Chest 152(2):435–444. https://doi.org/10.1016/j.chest.2017.01.026
Demir CEK (2015) The role of stem cells in obstructive sleep apnea syndrome. J Turk Sleep Med 2:25–28. https://doi.org/10.4274/jtsm.02.007
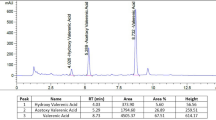
Huang T, Zeleznik O, Poole E et al (2017) Habitual sleep quality, plasma metabolites, and risk of coronary heart disease in postmenopausal women. Circulation 136(suppl_1):A13603-A. https://doi.org/10.1093/ije/dyy234
Gökçe S, Mert H (2015) Investigation of sleep quality and related factors in patients with heart failure. J of Educ and Res in Nurs 12(2):113–120. https://doi.org/10.5222/HEAD.2015.113
Lao XQ, Liu X, Deng HB et al (2018) Sleep quality, sleep duration, and the risk of coronary heart disease: a prospective cohort study with 60,586 adults. J Clin Sleep Med 14(1):109–117. https://doi.org/10.5664/jcsm.6894
Wang S, Li Z, Wang X et al (2022) Associations between sleep duration and cardiovascular diseases: a meta-review and meta-analysis of observational and Mendelian randomization studies. Front Cardiovasc Med 9:930000. https://doi.org/10.3389/fcvm.2022.930000
Yin J, Jin X, Shan Z et al (2017) Relationship of sleep duration with all-cause mortality and cardiovascular events: a systematic review and dose-response meta-analysis of prospective cohort studies. J Am Heart Assoc 6:9. https://doi.org/10.1161/JAHA.117.005947
Habibović M, Mudde L, Pedersen S et al (2018) Sleep disturbance in patients with an implantable cardioverter defibrillator: prevalence, predictors and impact on health status. European J of Cardiovasc Nurs 17(5):390–398. https://doi.org/10.1177/1474515117748931
Nagai M, Hoshide S, Kario K (2010) Sleep duration as a risk factor for cardiovascular disease-a review of the recent literature. Curr Cardio Rev 6(1):54–61. https://doi.org/10.2174/157340310790231635
Meng L, Ding Y, Li J et al (2022) Impact of inflammatory markers on the relationship between sleep quality and diabetic kidney disease. Sleep Breath 26(1):157–165. https://doi.org/10.1007/s11325-021-02380-6
Newman AB, Spiekerman CF, Lefkowitz D et al (2000) Daytime sleepiness predicts mortality and cardiovascular disease in older adults. J Am Geriatr Soc 48(2):115–123. https://doi.org/10.1111/j.1532-5415.2000.tb03901.x
Zhuang Z, Gao M, Yang R et al (2020) Association of physical activity, sedentary behaviours and sleep duration with cardiovascular diseases and lipid profiles: a Mendelian randomization analysis. Lipids Health Dis 19(1):86. https://doi.org/10.1186/s12944-020-01257-z
Atef H, Abdeen H (2021) Effect of exercise on sleep and cardiopulmonary parameters in patients with pulmonary artery hypertension. Sleep Breath 25(4):1953–1960. https://doi.org/10.1007/s11325-020-02286-9
Calero K, Anderson WM (2019) Can poor sleep cause kidney disease? Another step closer to the answer. J Clin Sleep Med 15:371–372. https://doi.org/10.5664/jcsm.7652
Park S, Lee S, Kim Y et al (2020) Short or long sleep duration and CKD: a mendelian randomization study. J Am Soc Nephrol 31:2937–2947. https://doi.org/10.1681/ASN.2020050666
Ahmad S, Gupta M, Gupta R et al (2013) Prevalence and correlates of insomnia and obstructive sleep apnea in chronic kidney disease. N Am J Med Sci 5(11):641–646. https://doi.org/10.4103/1947-2714.122306
Lee HJ, Kwak N, Kim YC et al (2021) Impact of sleep duration on mortality and quality of life in chronic kidney disease: results from the 2007-2015 KNHANES. Am J Nephrol 52:1–8. https://doi.org/10.1159/000516096
Hao Q, Xie M, Zhu L et al (2020) Association of sleep duration with chronic kidney disease and proteinuria in adults: a systematic review and dose-response meta-analysis. Int Urol Nephrol 52:1305–1320. https://doi.org/10.1007/s11255-020-02488-w
Tan NYQ, Chan J, Cheng CY et al (2018) Sleep duration and diabetic kidney disease. Front Endocrinol 9:808. https://doi.org/10.3389/fendo.2018.00808
Bo Y, Yeoh EK, Guo C et al (2019) Sleep and the risk of chronic kidney disease: a cohort study. J Clin Sleep Med 15:393–400. https://doi.org/10.5664/jcsm.7660
Hildreth CM (2011) Prognostic indicators of cardiovascular risk in renal disease. Front Physiol 2:121
Neumann J, Ligtenberg G, Klein II et al (2004) Sympathetic hyperactivity in chronic kidney disease: pathogenesis, clinical relevance, and treatment. Kidney Int 65(5):1568–1576
Ricardo AC, Knutson K, Chen J et al (2017) The association of sleep duration and quality with CKD progression. Journal of the American Society of Nephrology 28(12):3708–3715. https://doi.org/10.1681/ASN.2016121288
Kurt R, Şahin A, Güneş H et al (2020) Association between natriuretic peptide levels and sleep quality in patients with heart failure. MN Kardiyoloji 27(4):189–196
Liu Y, Wheaton AG, Croft JB et al (2018) Relationship between sleep duration and self-reported health-related quality of life among US adults with or without major chronic diseases, 2014. Sleep Health 4(3):265–272. https://doi.org/10.1016/j.sleh.2018.02.002
Cho E-H, Lee H, Ryu OH et al (2014) Sleep disturbances and glucoregulation in patients with type 2 diabetes. J of Korean Medical Sci 29(2):243–247. https://doi.org/10.3346/jkms.2014.29.2.243
Calhoun DA, Harding SM (2010) Sleep and hypertension. Chest 138(2):434–443. https://doi.org/10.1378/chest.09-2954
Redline S, Foody J (2011) Sleep disturbances: time to join the top 10 potentially modifiable cardiovascular risk factors? Am Heart Assoc 124:2049–2051. https://doi.org/10.1161/CIRCULATIONAHA.111.062190
Turek NF, Ricardo AC, Lash JP (2012) Sleep disturbances as nontraditional risk factors for development and progression of CKD: review of the evidence. Am J of Kidney Dis 60(5):823–833. https://doi.org/10.1053/j.ajkd.2012.04.027
Acknowledgements
We would like to thank all patients who participated in this study and all hospital staff who helped.
Funding
The funding source was covered by the researchers.
Author information
Authors and Affiliations
Contributions
Esma Gökçe designed the study, analyzed the data, and drafted the manuscript. Arzu İşler collected the data. Sevban Arslan critically revised the manuscript and supervised this project. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Ethics committee approval dated 08.03.2019 and numbered 86 was obtained from the non-interventional clinical research ethics committee for the study. The permission of the official institution, numbered 61229848-622.01/, was obtained from the Medical Faculty Hospital Health Application and Research Center. The study was carried out in accordance with the principles of the Declaration of Helsinki, which was revised in 2008. The study is based on the STROBE sectioning guidelines.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This study is limited only to the findings of patients hospitalized in the cardiology department of a university hospital.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gökçe, E., Arslan, S. & İşler, A. Correlation of plasma metabolites and comorbid illnesses with poor sleep quality in patients with coronary heart disease. Sleep Breath 27, 2249–2255 (2023). https://doi.org/10.1007/s11325-023-02835-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-023-02835-y