Abstract
Objective
The purpose of this study is to examine the pathophysiology underlying sleep apnea (SA).
Background
We consider several critical features of SA including the roles played by the ascending reticular activating system (ARAS) that controls vegetative functions and electroencephalographic findings associated with both SA and normal sleep. We evaluate this knowledge together with our current understanding of the anatomy, histology, and physiology of the mesencephalic trigeminal nucleus (MTN) and mechanisms that contribute directly to normal and disordered sleep. MTN neurons express γ-aminobutyric acid (GABA) receptors which activate them (make chlorine come out of the cells) and that can be activated by GABA released from the hypothalamic preoptic area.
Method
We reviewed the published literature focused on sleep apnea (SA) reported in Google Scholar, Scopus, and PubMed databases.
Results
The MTN neurons respond to the hypothalamic GABA release by releasing glutamate that activates neurons in the ARAS. Based on these findings, we conclude that a dysfunctional MTN may be incapable of activating neurons in the ARAS, notably those in the parabrachial nucleus, and that this will ultimately lead to SA. Despite its name, obstructive sleep apnea (OSA) is not caused by an airway obstruction that prevents breathing.
Conclusions
While obstruction may contribute to the overall pathology, the primary factor involved in this scenario is the lack of neurotransmitters.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sleep apnea (SA) is a respiratory disorder characterized by intermittent reductions (hypopnea) or full cessation (apnea) of breathing for a few seconds or as long as a few minutes; these episodes may occur many times during sleep.Footnote 1 More than one billion individuals worldwide currently experience some form of sleep apnea [1]. The number of individuals carrying this diagnosis has been rising steadily. SA can have a negative effect on quality of life and may also increase the risk of premature death. Of note, SA is a significant risk factor associated with mortality due to all causes, particularly those associated with cardiovascular events [2].
Materials and methods
We reviewed the published literature focused on sleep apnea (SA) reported in Google Scholar, Scopus, and PubMed databases. We used these findings to inform our review that focused on the role of the mesencephalic trigeminal nucleus (MTN).
Background
While several types of this disorder have been identified, the two most prominent forms are obstructive and central SA. Obstructive sleep apnea (OSA), which is the more common of the two forms, is believed to be a result of complete or partial obstruction of the upper airway during sleep. By contrast, central sleep apnea (CSA) results from dysfunction of the respiratory control centers of the brain stem, most notably the pre-Bötzinger complex. In CSA, the respiratory control center fails to provide the signal to inhale, causing the individual to miss one or more breathing cycles while asleep.
Sleep
Sleep is a complex physiological mechanism that involves the actions of numerous components of the central nervous system (CNS). Sleep is induced and maintained by CNS-mediated inhibition of neurons in the ascending reticular activating system (ARAS) nuclei mediated by the hypothalamic neurons of the preoptic area (POA), the thalamic reticular nucleus, and the nucleus accumbens [3]. Neurons in the POA release inhibitory neurotransmitters such as ɣ-aminobutyric acid (GABA) and galaninFootnote 2 to activate neurons in ARAS, including orexinergic neurons of the lateral hypothalamus, histaminergic neurons of the tuberomammillary nucleus, glutamatergic neurons of the parabrachial nucleus (PBN) in the dorsolateral pons, serotonergic neurons of the dorsal raphe nuclei, noradrenergic neurons of the locus coeruleus, and cholinergic neurons of the basal forebrain, laterodorsal tegmentum, and pedunculopontine tegmentum. GABA released by the hypothalamus inhibits the ARAS and neurotransmitters are not released [4, 5].
MTN consists of a narrow band of cells that passes near the periaqueductal grey and is completely incorporated in the Reticular Formation [6]. Adjacent to the MTN, towards the centre and in front of the fourth ventricle, is the locus coeruleus (LC), which is the main source of noradrenergic fibers in the CNS and is the origin of the sympathetic nervous system.
The LC and MTN are closely related during embryonic development: the LC plays a role in the differentiation of MTN neurons, which in turn are necessary for proper LC functioning (Espana A, 2012).
The ascending reticular activating system (ARAS)
Neurotransmitters released by the ARAS activate the cerebral cortex. These neurotransmitters also control the activity of the lungs and heart [7]. Reduced levels of norepinephrine in the brainstem also contribute to the development of respiratory disturbances [8, 9]. Similarly, dopamine stimulates respiratory and cardiovascular function [10] and medullary serotonergic neurons modulate respiratory responses [11, 12]. Orexin, which is an important promoter of wakefulness, also stimulates respiratory and cardiovascular responses [13,14,15] as well as testosterone synthesis [16, 17]. Testosterone stimulates the activity of the respiratory and cardiovascular systems, especially in the male sex; therefore, in the male, in addition to the decreased contribution of orexin to respiratory control, it also lacks the contribution of a greater amount of testosterone. This finding may explain at least in part the prevalence of SA in men [18,19,20,21,22]. Likewise, neurons in the PBN play a particularly important role in SA development. These neurons respond to excitatory signals provided by the amino acid, L-glutamate as well as inhibitory signals mediated by GABA, and are modulated by signals from cholinergic, monoaminergic, and orexinergic/hypocretinergic neurons as well as those that express melanin-concentrating hormone (MCH) that are directly involved in the control of both respiratory and cardiovascular function. These distinct neuronal populations mediate continuous interactions between the cortex and subcortical circuits and can modulate sympathetic and cardiovagal output, respiratory patterns, and chemosensitivity [23, 24].
While neurotransmitter release from the ARAS remains ongoing to some extent, overproduction of GABA by the neurons in the POA during sleep might result in a significant reduction in the release of one or more of these neurotransmitters from the ARAS.
The mesencephalic trigeminal nucleus (MTN)
The mesencephalic trigeminal nucleus (MTN) is a brainstem structure that activates the release of neurotransmitters from the ARAS during sleep. Neurons in the MTN are activated by GABA released from the POA. Activated MTN cells respond by releasing glutamate that then activates the ARAS and promotes the release of neurotransmitters that modulate the activity of the cerebral cortex as well as the respiratory and cardiovascular systems [25]. Glutamate from MTN cells can also modulate the activity of neurons in the motor trigeminal nucleus (Mo5), thereby activating the muscles of mastication; this results in the clenching of the teeth (i.e., rhythmic masticatory muscle activity (RMMA), also known as sleep bruxism (SB)) and increasing glutamate release and activation of the ARAS [25].
Electroencephalographic findings during sleep
Neurons in the POA release GABA for the entire duration of sleep. Thus, the MTN must remain activated during the entire duration of sleep (most evidently, on the EEG, during NREM sleep) to maintain activation of the ARAS to support glutamate release. Of note, on an electroencephalogram (EEG), only electrocortical signals associated with responses to GABA and glutamate will be detected.
Electroencephalographic sleep structure
Sleep includes two distinct phases. The first, in which the eyes move rapidly, is known as rapid eye movement (REM) sleep. The EEG associated with this phase is rapid and unsynchronized. By contrast, the EEG pattern detected during NREM phases is slow and synchronized. An example of an NREM trace is shown in Figs. 1, 2 and 3.
In this image, we can detect both baseline traces and cycles in which these patterns have been altered. In addition to these macrostructural sleep stages, microstructural features of NREM detected on EEG include alternating fluctuations characterized as sleep “superficialization” [26]. This type of EEG trace, which is known as a “cycle alternating pattern” (CAP) can be detected for either brief or long periods and can be interrupted by periods of normal EEG activity characteristic of NREM sleep (Fig. 4).
Each CAP cycle is defined by alternating sequences of two EEG patterns known as the A and B-phases. These variations are closely related to fluctuations in the levels of arousal that characterize the two different functional states and that are mediated by the arousal control mechanism [27]. Arousal is mediated by ARAS activation [28, 29]. The A-phase represents an activation response and includes both slow high-voltage (synchronized) and fast low-voltage (unsynchronized) waves. These phases are associated with temporary increases in the level of consciousness, muscle tone, and vegetative functions associated with ARAS neuronal activation during sleep. GABA released from hypothalamic POA neurons activates the MTN which in turn activates the ARAS nuclei. Neurons in the MTN express GABA-depolarizing ionotropic receptors that produce slow but large and sustained chloride currents when activated [30, 31]. Thus, MTN neurons respond with prolonged activation that can be maintained throughout the duration of sleep. Detection of CAP and non-CAP (NCAP) phases on EEG is linked to the specific kinetics of these GABA-depolarizing receptors.
Sleep apnea
Apneic episodes appear often, but not always, immediately after phase A during the B-(inhibitory) phase of the CAP [24, 32, 33] (Fig. 5).
Modulation of EEG responses based on respiratory events. Respiratory events are as indicated within the boxes, including (from left to right) hypopnea, apnea, hypopnea, apnea, and hypopnea. The apneic episodes appeared exclusively during the inhibitory B-phase of NREM sleep and concluded at the beginning of the A-phase of the CAP. Resumption of breathing is always signaled by conversion to an A-phase pattern [24, 32, 33]
Results (pathophysiology of sleep apnea)
Apnea occurs when brainstem structures responsible for activating the respiratory system (i.e., the ARAS nuclei and brainstem structures associated with the pre-Bötzinger complex) are inactivated (CSA) or when individuals are unable to overcome resistance (obstruction) in the airways (OSA). We hypothesize that these findings are largely the result of an excess of GABAergic-mediated inhibition of the POA and/or insufficient MTN-mediated activation of the ARAS nuclei and their collective impact on the respiratory system during sleep. In the text to follow, we analyze the various parameters revealed by EEGs performed on individuals during sleep (i.e., polysomnography (PSG)).
The only forms of cyclic activation recorded by EEG during NREM sleep were A-phases of CAPs [34, 35]. We note that only the MTN can undergo physiologic cyclic activation for the entire duration of the NREM sleep, leading to activation of the ARAS and generation of increased cortical activity recorded by the EEG; thus, we hypothesize that the CAP A-phases are regulated by signals from the MTN. We distinguish 3 types of A-Phases, A1, A2, and A3 with increasing of arousal threshold (the arousal threshold is the propensity to wake up from sleep), each A-phase marks a single cycle of neurotransmitter release from the ARAS; all A-phase subtypes were shown to be capable of reinstatement of breathing [36], with the strongest effect nonetheless noted during A3 [36, 37]. In milder obstructive sleep apnea (apnea–hypopnea index < 20), sleep continuity may be reinforced by cyclic alternating pattern subtype A1, whereas in more severe obstructive sleep apnea, decompensation of these sleep-stabilizing mechanisms may occur and more intrusive cyclic alternating pattern fluctuations disrupt sleep circuitry [37] the action of the MTN causes the release of many neurotransmitters. By contrast, the NCAP and CAP B-phases result from the actions of GABA on ARAS neurons; the MTN remains active at these times.
Airway obstruction cannot be the sole cause of obstructive sleep apnea (OSA)
Findings from the EEG tracings reveal that apneic episodes occur exclusively during inhibitory B-phases; the resumption of breathing correlates with an activating A-phase pattern [24, 32, 33]. Apneic episodes are never detected during CAP A-phases. During this phase, neurotransmitters are released from the ARAS and apnea ceases. Of note, CAPs and apneic periods are recorded with different instruments; thus, a coincidence of events most likely represents a relationship between these two mechanisms. Of note, obstructive mechanisms modulate the responses of the respiratory system alone while central mechanisms (i.e., ARAS neurotransmitter deficiency) will have an impact on both the CNS and the respiratory system. Thus, if obstruction was the sole cause of OSA, CAP phase-B periods on EEG would be unlikely to correlate specifically with apneic events. Thus, we hypothesize that OSA may also be the result of ARAS neurotransmitter deficiency. Of note, apneic episodes are always detected in association with CAP B-phases and never during corresponding NCAP phases. Thus, SA is unlikely to be a result of GABA-mediated inhibition of the ARAS. If this was the case, SA would also be detected during NCAP phases, which are the most abundant in terms of time. By contrast, the actions of the MTN are more likely to result in apneic responses. A more careful analysis of EEG/ polysomnography (PSG) results corresponding to RMMA/SB episodes reveals that:
-
RMMA episodes result from a sequence of events associated with sleep micro-arousal. During the seconds to minutes that immediately precede the onset of RMMA, the heart and brain become activated [38]; the respiration rate also increases typically before the onset of muscle activity [39]. These results imply that the MTN is active and activates the nuclei of the ARAS during the NCAP phases of sleep, thereby preventing the onset of SA. Thus, apnea can only develop once the MTN has released all its glutamate stores and fully activated the nuclei of the ARAS, leaving it functionally inactive.
-
MTN remains activated throughout the duration of sleep, including during the CAP B-phases and NCAP. However, after an A-phase, which is accompanied by prominent glutamate release, the MTN may be functionally depleted, and apnea can occur. While the impact of GABA prevails during the NCAP phase, the MTN remains capable of glutamate release and apnea does not occur. Therefore, OSA is not the direct result of the airway obstruction; while this feature remains an essential co-factor in the mechanism underlying OSA, the primary contributing factor to this phenomenon is the temporary absence of ARAS-derived neurotransmitters.
CAP rates, the PBN, and the MTN and their contributions to SA
The number of CAP events detected on an EEG during 1 h of NREM sleep is known as the “CAP-rate” (CAP rate is the percentage ratio of total CAP time to NREM sleep time [33]. This value provides us with information on MTN activity,the remainder of the EEG tracing (i.e., the NCAP) reflects GABAergic activity. Therefore, a relatively low CAP rate suggests minimal MTN activity and the predominance of GABA and its associated neurotransmitters, and vice versa [40]. Measurements of the CAP rate might provide substantial insight into the differential diagnosis of neurological pathologies and may provide a means to evaluate the effectiveness of specific pharmacological treatments.
Results from previous studies revealed that individuals manifesting symptoms of depression exhibit higher CAP rates on EEG [41]. This finding implies that their ARAS nuclei are comparatively inactive and release lower levels of neurotransmitters in the CNS (i.e., less GABA leads to a higher CAP rate). This information might ultimately be developed and used to confirm the diagnosis of depression and to determine whether the prescribed therapies are having an impact at least at the physiological/neurologic level.
Similarly, patients diagnosed with migraine were found to have lower than normal CAP rates [42]. This information, which reflects an overabundance of neurotransmitters, might also contribute to the differential diagnosis of this neurological condition.
Given that mechanisms underlying SA include excess GABA release by the POA, the CAP rate detected on EEG should be at normal or lower than normal levels [43]. However, higher than normal CAP rates were detected in patients diagnosed with severe SA [33]. In general, patients with severe SA (i.e., those with apnea/hypopnea index (AHIs) ≥ 20 events/h) exhibit higher CAP rates on EEG; by contrast, those with mild to moderate disease (AHI < 20 events/h) have normal or reduced CAP rates [43]. Among the explanations for these observations, Kaur et al. [44] described several subcortical arousal circuitries and hypothesized that overly intense physiological stimulation (i.e., AHI ≥ 20events/h) may overwhelm the brain’s sleep-gating mechanisms. Among their findings, Kaur et al. [44] demonstrated the existence of ascending and descending projections from subregions of PBN that play a central role in inducing cortical arousal and regulating respiratory responses. Their results also revealed two functionally distinct arousal states that potentially arise from the ascending projections of the PBN with links to the basal forebrain and other hypothalamic, insular, and thalamo-cortical targets. In this model, baseline arousal is supported, at least in part, by excitatory inputs from the medial PBN. This state is altered in response to sleep-active GABAergic neurons in the medullary parafacial zone; this leads to profound increases in the synchronization of slow-wave sleep [45]. By contrast, visceral sensory distress (e.g., pain or respiratory insufficiency) stimulates the lateral subregions of the PBN and evokes more potent basal forebrain arousal [44]. The electrocortical signature of this activity includes higher alpha/beta frequency bursts that are consistent with the A-phase of the CAP response. Furthermore, in experiments performed in rodents, hypercapnic stimulation of the lateral PBN in rodents led to a powerful concomitant resumption of breathing via its descending medullary projections [44, 46]. This property of the PBN is somewhat reminiscent of the dual activation capacity of the MTN and its role in promoting motor (Mo5) activation that leads to RMMA and SB [25, 38, 39, 47,48,49,50,51]. Activation of the MTN in this setting leads to the release of larger quantities of glutamate and thus increased activation of ARAS neurons, particularly those of the PBN that lead to increases in heart, respiratory, and CAP rates. Of note, excess GABA released by the POA is the source of “visceral distress” that leads to the activation of the MTN. The fact that ARAS neurons (the PBN in particular) and MTN exhibit two functionally distinct arousal states is unlikely to be a coincidence [52].
Sleep apnea (SA) and REM sleep
As noted above, CAPs are detected only during periods of NREM sleep. Nonetheless, SA can also occur during REM sleep. This is because ARAS neurotransmitters may be released in reduced quantities or not released at all. This will prevent the switch from NREM to REM sleep cycles. Osorio-Forero et al. [53] reported that norepinephrine levels declined steeply during REM sleep. Released neurotransmitter from locus coeruleus REM-OFF neurons acts on the pedunculopontine tegmentum REM-ON neurons to prevent REM sleep; thus, norepinephrine levels tend to be very low during this sleep cycle, and SA can develop. Likewise, the orexinergic tone is completely absent during REM sleep [54]. Both dorsal raphe nucleus serotonergic and TMN histaminergic neurons appear to be electrically silent during REM sleep [55, 56]. Therefore, ARAS neurotransmitter deficiencies associated with SA also persist during REM sleep.
Causes of sleep apnea (SA)
The absence of one or more neurotransmitters during sleep may be due to the excessive actions of the POA (i.e., GABA release), but may also be due to an ineffective MTN. Among the mechanisms associated with an ineffective MTN, we consider the following:
-
Sudden infant death syndrome (SIDS) can occur in newborns, mainly between the second and sixth months of life. During the first month of life, a newborn does not experience true NREM but instead exhibits a unique type of REM sleep. On or about the sixth month of life, deciduous teeth emerge and the MTN becomes more effective [57]. Results from multiple studies document that pacifier use can reduce the risk of SIDS [58], and can also activate the MTN.
-
The MTN may also be rendered ineffective in elderly, edentulous individuals who need to sleep with their mouths open in order to breathe because of airway obstruction [59,60,61,62].
Diagnosis
A diagnosis of SA can be established by the results of a PSG examination or (more easily but less precisely) via the use of an oximeter. Many patients are diagnosed based on reports from spouses that he or she stops breathing for a substantial period of time while asleep. Even if the diagnosis is clear, it is important to understand why and how this patient developed SA. This will require a careful medical history and clinical examination to detect problems that may include substance abuse, drugs, obstructions, and lack of or complete absence of teeth. It is not possible to treat SA without identifying and (if possible) eliminating the underlying cause.
Agents that can cause sleep apnea
Substances and drugs that over-stimulate GABA release from the POA can cause or exacerbate SA. Among the risk factors in this category, attention should be paid to alcohol [63] and tobacco use [64], use of opioids and/or cannabis [65, 66], and obesity [67]. Several of these agents may also result in SB [68,69,70,71]. Furthermore, some anticonvulsants that amplify signaling via GABA-A receptors can elicit or exacerbate SA [72]. Similarly, some antidepressants increase the levels of neurotransmitters detected in the CNS [73]. The use of some anticonvulsant [70] and antidepressant medications [74] can also result in SB. Of note, none of these drugs promote airway obstruction.
Therapies for sleep apneas
Some alternative antidepressants that might be considered include the selective norepinephrine reuptake inhibitor, reboxetine together with the antimuscarinic hyoscine butylbromide [75], and the serotonin modulator, trazodone [76]; mirtazapine is another potential choice [77]. Patients often receive supplemental oxygen administered via C-PAP and BiPAP, among other devices. While these therapies provide excellent support for increased oxygen intake of oxygen, they may not be a very effective means to treat cardiac complications associated with central apneas. Many of these same antidepressants can also be used to treat SB (Grinshpoon A, 2014; Khosravi M, 2020).
The use of the anti-hypertensive agent, clonidine, has been associated with diminished susceptibility to central apnea [78] and can also be used to treat SB [79, 80]. Interestingly, clonidine is a selective centrally-acting alpha-2-adrenergic agonist that alters the NREM/REM cycle via dose-dependent reductions in REM sleep [81]. Clonidine can be used to treat SA and SB and also reduces the incidence of RMMA while increasing the CAP rate [82]. While this appears to be a paradoxical effect of this drug, it is important to recognize that although Mo5 contains many adrenergic receptors [83, 84], clonidine activates only those of the α2 class. Hence, clonidine inhibits Mo5 while stimulating GABA release in the hypothalamus and thus activating MTN neurons [85,86,87]. Thus, clonidine appears to be an excellent drug that might be used for the management of SA. Further understanding of the impact of clonidine on Mo5 and MTN will require additional research.
As a final note, we ask our readers to understand that this chapter was not designed to be an exhaustive survey of drugs that might cause or be used to treat SA. Instead, we have chosen to highlight some of the agents that can cause SA and discuss some of the drugs that might be used for its treatment.
Sleep apnea and sudden unexplained death during sleep (SUDS)
SA and its associated causes are quite hazardous to one’s health, most notably in patients with pre-existing cardiac and bronchopulmonary pathology. Three hundred to four hundred thousand of these patients die during sleep each year in the USA alone [2, 88,89,90,91]. We have already discussed SIDS and its impact on infants. While the pathogenesis of SUDS has not yet been elucidated, families with a significant history of this disorder are more likely to present with significant nocturnal hypoxia [92,93,94] and a lack of ARAS neurotransmitters [95].
Discussion
MTN is the only structure in the brainstem (and perhaps in the entire CNS) that remains activated during sleep. The MTN can activate nuclei of the ARAS followed by the cerebral cortex as well as the cardiovascular and respiratory systems. These findings were confirmed in PSG studies in which different instruments (e.g., EEG, ECG, EMG, pulse oximeter, and nasal cannulas) simultaneously record the results of MTN activation that correspond to episodes of SA and RMMA. EEGs performed during sleep permit us to distinguish between different phases of CAP and NCAP; these tracing also distinguish between phases of greater (CAP phase-A) and reduced cerebral activation (CAP phase-B). Notably, SA occurs only during intervals corresponding to CAP phase-B. Because CAP phase-A corresponds to activation of the MTN and NCAP phases feature increases in heart and respiratory rate, these results suggest SA occurs only when the MTN has become nearly inactive. These features are also observed in OSA; thus, the key element of this response appears to be MTN inactivity. This is especially the case in “fragile” patients, including those with respiratory problems.
One key finding of our study was that the main cause of OSA cannot be obstruction per se. If this was the case, then episodes of SA should also be prominent during the NCAP phases. While the pathogenetic mechanisms we have described are clearly valid for CSA (i.e., decreased release of ARAS neurotransmitters prevents the appropriate functioning of the respiratory system both directly and via mechanisms promoting dysfunction of the parabrachial nucleus and pre-Bötzinger complex), they also explain many of the signs and symptoms of more commonly diagnosed OSA. As a case in point, we considered what might happen in response to an MTN that has not been fully activated (e.g., in the absence of teeth in both newborns and the elderly). In both cases, our findings revealed an increase in the number of unexplained deaths during sleep, suggesting that the pathogenic mechanisms underlying both SIDS and SUDS may relate directly to the absence of ARAS-derived neurotransmitters and SA.
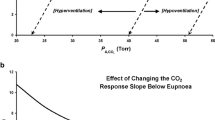
We would like to point out that the apneas we talked about in this paper, sleep apneas, occur almost exclusively in healthy individuals or with small comorbidities (obstructions, obesity) and that, in these patients, apneas never occur during wakefulness, therefore sleep, with its mechanisms, is a “conditio sine qua non” for apneas. There are other apneas such as those occurring in Cheyne–Stokes breathing, in which the apnea can also occur while awake, but we are talking about patients with major problems: damage to respiratory centers, or by heart failure, newborns with immature respiratory systems, kidney failure, narcotic poisoning, and raised intracranial pressure. The pathophysiology of Cheyne–Stokes breathing can be summarized as apnea leading to increased CO2 which causes excessive compensatory hyperventilation, in turn causing decreased CO2 which causes apnea, restarting the cycle, it is not related to sleep, but can also occur during sleep.
Precisely the fact that apneas have a strong correlation with the B-phase of the CAPs (when the action of the MTN has finished) and not in the A-phase or in the NCAP phases, when the MTN is active, perhaps less active than POA GABA, but nonetheless active, provides evidence that apneas are due to one or more ARAS neurotransmitters deficiency.
Conclusions and suggestions
CAPs identified on EEGs are generated in response to the activation of the MTN.
SA is the result of a deficiency of one or more neurotransmitters released by the ARAS. This deficiency has been reported in association with both REM and NREM sleep. Therefore, SA can occur during both phases.
While deficiencies in one or more of the ARAS neurotransmitters during sleep may be due to the excessive activation of the POA (i.e., the release of GABA), this state may also be due to MTN in an ineffective state.
Despite its name, OSA is not caused by an airway obstruction that prevents breathing. While obstruction may contribute to the overall pathology, the primary factor involved in this scenario is the lack of neurotransmitters.
SA and the associated deficiency of ARAS-derived neurotransmitters have been linked to unexplained death during sleep. We recognize that these neurotransmitters also act on the cardiovascular system. Thus, the overall lack of neurotransmitters may also lead to cardiovascular problems, including cardiac arrest and death.
SB results in an increase in the level of ARAS neurotransmitter release and by doing so prevents the development of SA and associated heart problems. Patients presenting with signs and symptoms of SB might be responding by activating a defense mechanism against GABA excess.
Substances and drugs that over stimulate the release of GABA from the POA can cause or exacerbate pre-existing SA.
In conclusion, the pathophysiologic factors associated with the development of SA are directly related to central mechanisms modulating normal sleep. Patients presenting with suspected SA might be managed with an oximeter and heart rate monitor equipped with a powerful alarm. Thus, if the oxygen saturation and/or heart rate drop too low, an alarm will be activated. This very simple strategy may ultimately save his or her life. Devices of this type are already available for purchase; they are inexpensive and may save many lives if properly calibrated and used on a routine basis.
Data availability
I confirm I have included a data availability statement in my main manuscript file.
Notes
For simplicity, this review will focus primarily on SA, but will also refer to sleep hypopnea as relevant.
In the text to follow, we refer to GABA only.
Abbreviations
- AHI:
-
Apnea hypopnea index
- ARAS:
-
Ascending reticular activating system
- BiPAP:
-
Bilevel positive Airway pressure
- CAP:
-
Cycle alternating pattern
- CNS:
-
Central nervous system
- SA:
-
Sleep apnea
- CPAP:
-
Continuous Positive Airway Pressure
- CSA:
-
Central sleep apnea
- GABA:
-
ɣ-Aminobutyric acid
- ECG:
-
Electrocardiogram
- EEG:
-
Electroencephalogram
- EMG:
-
Electromyogram
- LC:
-
Locus coeruleus
- MCH:
-
Melanin-concentrating hormone
- Mo5:
-
Motor trigeminal nucleus
- MTN:
-
Mesencephalic trigeminal nucleus
- NCAP:
-
Non cycle alternating pattern
- NREM:
-
Non rapid eye movement
- OSA:
-
Obstructive sleep apnea
- PBN:
-
Parabrachial nucleus
- POA:
-
Preoptic area
- PSG:
-
Polysomnography
- REM:
-
Rapid eye movement
- RMMA:
-
Rhythmic masticatory muscle activity
- SB:
-
Sleep bruxism
- SIDS:
-
Sudden infant death syndrome
- SUDS:
-
Sudden unexplained death syndrome
- TMN:
-
Tubero-mammilary nucleus
References
Lyons MM, Bhatt NY, Pack AI, Magalang UJ (2020) Global burden of sleep-disordered breathing and its implications. Respirology 25(7):690–702. https://doi.org/10.1111/resp.13838
Heilbrunn ES, Ssentongo P, Chinchill VMI, Oh J, Ssentongo AE (2021) Sudden death in individuals with obstructive sleep apnoea: a systematic review and meta-analysis. BMJ Open Respir Res 8(1):e000656. https://doi.org/10.1136/bmjresp-2020-000656
Luppi PH, Fort P (2018) Neuroanatomical and Neurochemical Bases of Vigilance States. Handb Exp Pharmacol. https://doi.org/10.1007/164_2017_84
Szymusiak R, Steininger T, Alam N, McGinty D (2001) Preoptic area sleep-regulating mechanisms. Arch Ital Biol 139(1–2):77–92
Szymusiak R, McGinty D (2008) Hypothalamic regulation of sleep and arousal. Ann N Y Acad Sci 1129:275–86. https://doi.org/10.1196/annals.1417.027
Rokx JT, Jüch PJ, van Willigen JD (1986) Arrangement and connections of mesencephalic trigeminal neurons in the rat. Acta Anat (Basel) 127(1):7–15
Doi A, Ramirez J-M (2010) State-dependent interactions between excitatory neuromodulators in the neuronal control of breathing. J Neurosci 30(24):8251–62. https://doi.org/10.1523/JNEUROSCI.5361-09.2010
Viemari JC, Ramirez JM (2006) Norepinephrine differentially modulates different types of respiratory pacemaker and non pacemaker neurons. J Neurophysiol 95:2070–2082
Zanella S, Roux JC, Viemari JC, Hilaire G (2006) Possible modulation of the mouse respiratory rhythm generator by A1/C1 neurones. Respir Physiol Neurobiol 153:126–138. https://doi.org/10.1016/j.resp.2005.09.009,pmid:16309976
Song ZY, Yi HL (2017) Progress of dopamine in obstructive sleep apnea hypopnea syndrome Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 52(7):549–551. https://doi.org/10.3760/cma.j.issn.1673-0860.2017.07.018
Benarroch EE (2014) Neurology medullary serotonergic system: organization, effects, and clinical correlations. Neurology 83(12):1104–1111. https://doi.org/10.1212/WNL.0000000000000806
Hilaire G, Voituron N, Menuet C, Ichiyama RM, Subramanian HH, Dutschmann M (2010) The role of serotonin in respiratory function and dysfunction. Respir Physiol Neurobiol 174(1–2):76–88. https://doi.org/10.1016/j.resp.2010.08.017
Barnett S, Li A (2020) Orexin in respiratory and autonomic regulation, health and diseases. Compr Physiol 10(2):345–363. https://doi.org/10.1002/cphy.c190013
Kuwaki T (2021) Orexin (hypocretin) participates in central autonomic regulation during fight-or-flight response. Peptides 139:170530. https://doi.org/10.1016/j.peptides.2021.170530
Williams RH, Burdakov D (2008) Hypothalamic orexins/hypocretins as regulators of breathing. Expert Rev Mol Med 10:e28. https://doi.org/10.1017/S1462399408000823
Joshi D, Singh SK (2018) The neuropeptide orexin A - search for its possible role in regulation of steroidogenesis in adult mice testes. Andrology 6(3):465–477. https://doi.org/10.1111/andr.12475
Assisi L, Pelagalli A, Squillacioti C, Liguori G et al (2019) Orexin A-mediated modulation of reproductive activities in testis of normal and cryptorchid dogs: possible model for studying relationships between energy metabolism and reproductive control. Front Endocrinol (Lausanne) 22(10):816. https://doi.org/10.3389/fendo.2019.00816
Gencer B, Bonomi M, Adorni MP, Sirtori CR, Mach F, Ruscica M (2021) Cardiovascular risk and testosterone - from subclinical atherosclerosis to lipoprotein function to heart failure.Rev Endocr Metab Disord. https://doi.org/10.1007/s11154-021-09628-2
Jones TH, Kelly DM (2018) Randomized controlled trials - mechanistic studies of testosterone and the cardiovascular system. Asian J Androl Mar-Apr 20(2):120–130. https://doi.org/10.4103/aja.aja_6_18
Carbajal-García A, Reyes-García J (2020) Montaño LM Androgen effects on the adrenergic system of the vascular, airway, and cardiac myocytes and their relevance in pathological processes. Int J Endocrinol 12(2020):8849641. https://doi.org/10.1155/2020/8849641
Yeap BB, Dwivedi G, Chih HJ, Reid C et al (2000)Androgens and cardiovascular disease in men. Endotext
Yoshihisa A, Suzuki S, Sato Y, Kanno Y et al (2018) relation of testosterone levels to mortality in men with heart failure. Am J Cardiol 121(11):1321–1327. https://doi.org/10.1016/j.amjcard.2018.01.052
Benarroch EE (2019) Control of the cardiovascular and respiratory systems during sleep. Auton Neurosci 218:54–63. https://doi.org/10.1016/j.autneu.2019.01.007
Terzano MG, Parrino L, Boselli M, Spaggiari MC, Di Giovanni G (1996) Polysomnographic analysis of arousal responses in obstructive sleep apnea syndrome by means of the cyclic alternating pattern. J Clin Neurophysiol 13(2):145–55. https://doi.org/10.1097/00004691-199603000-00005
Giovanni A, Giorgia A (2021) The neurophysiological basis of bruxism. Heliyon 7(7):e07477. https://doi.org/10.1016/j.heliyon.2021.e07477
Terzano MG, Parrino L, Smerieri A (2001) Neurophysiological basis of insomnia: role of cyclic alternating patterns. Rev Neurol (Paris) 157(11 Pt 2):S62–S66
Terzano MG, Mancia D, Salati MR, Costani G et al (1985) The cyclic alternating pattern as a physiologic component of normal NREM sleep. Sleep 8(2):137–45. https://doi.org/10.1093/sleep/8.2.137
Hutt A, Lefebvre J (2021) Arousal fluctuations govern oscillatory transitions between dominant [Formula: see text] and [Formula: see text] occipital activity during eyes open/closed conditions. Brain Topogr. https://doi.org/10.1007/s10548-021-00855-z
Moruzzi G, Magoun HW (1949) Brain stem reticular formation and activation of the EEG. Electroencephalogr Clin Neurophysiol 1(4):455–473
Woodward RM, Polenzani L, Miledi R (1993) Characterization of bicuculline/baclofen-insensitive (π-like) γ- aminobutyric acid receptors expressed in Xenopus oocytes. II Pharmacology of γ-aminobutyric acid(A) and γ-aminobutyric acid(B) receptor agonists and antagonists. Mol Pharmacol 43:609–625
Jin Z, Jin Y, Birnir B (2011) GABA-activated single-channel and tonic currents in rat brain slices. J Vis Exp 53:2858. https://doi.org/10.3791/2858
Parrino L, Rausa F, Azzi N, Pollara I, Mutti C (2021) Cyclic alternating patterns and arousals: what is relevant in obstructive sleep apnea? In Memoriam Mario Giovanni Terzano. Curr Opin Pulm Med 27(6):496–504. https://doi.org/10.1097/MCP.0000000000000825
Terzano MG, Parrino L, Spaggiari MC (1990) Modifications of cyclic alternating pattern in sleep apnea syndrome. Eur Neurol 30(4):235–240. https://doi.org/10.1159/000117353
Ferini-Strambi L, Bianchi A, Zucconi M, Oldani A, Castronovo V, Smirne S (2000) The impact of cyclic alternating pattern on heart rate variability during sleep in healthy young adults. Clin Neurophysiol 111(1):99–101
Halász P, Terzano M, Parrino L, Bódizs R (2004) The nature of arousal in sleep. J Sleep Res 13(1):1–23
Parrino L, Ferri R, Bruni O, Terzano MG (2012) Cyclic alternating pattern (CAP): the marker of sleep instability. Sleep Med Rev 16(1):27–45. https://doi.org/10.1016/j.smrv.2011.02.003
Gnoni V, Drakatos P, Higgins S, Duncan I, Wasserman D, Kabiljo R, Mutti C, Halasz P, Goadsby PJ, Leschziner GD, Rosenzweig I (2021) Cyclic alternating pattern in obstructive sleep apnea: a preliminary study. J Sleep Res 30(6):e13350. https://doi.org/10.1111/jsr.13350
Lavigne GJ, Huynh N, Kato T, Okura K, Adachi K, Yao D, Sessle B (2007) Genesis of sleep bruxism: motor and autonomic-cardiac interactions. Arch Oral Biol 52(4):381–4. https://doi.org/10.1016/j.archoralbio.2006.11.017
Huynh N, Kato T, Rompré PH, Okura K, Saber M, Lanfranchi PA, Montplaisir JY, Lavigne GJ (2006) Sleep bruxism is associated to micro-arousals and an increase in cardiac sympathetic activity. J Sleep Res 15(3):339–346. https://doi.org/10.1111/j.1365-2869.2006.00536.x
Karimzadeh F, Nami M, Boostani R (2017) Sleep microstructure dynamics and neurocognitive performance in obstructive sleep apnea syndrome patients. J Integr Neurosci 16(2):127–142. https://doi.org/10.3233/JIN-170004
Farina B, Della Marca G, Grochocinski VJ, Mazza M, Buysse DJ, Di Giannantonio M, Francesco Mennuni G, De Risio S, Kupfer DJ (2003) Frank E Microstructure of sleep in depressed patients according to the cyclic alternating pattern. J Affect Disord 77(3):227–235
Della Marca G, Vollono C, Rubino M, Di Trapani G, Mariotti P, Tonali PA (2006) Dysfunction of arousal systems in sleep-related migraine without aura. Cephalalgia 26(7):857–864
Kheirandish-Gozal L, Miano S, Bruni O, Ferri R, Pagani J, Villa MP, Gozal D (2007) Reduced NREM sleep instability in children with sleep disordered breathing. Sleep 30(4):450–7
Kaur S, Saper CB (2019) Neural circuitry underlying waking up to hypercapnia. Front Neurosci 13:401. https://doi.org/10.3389/fnins.2019.00401
Anaclet C, Ferrari L, Arrigoni E, Bass CE, Saper CB, Lu J, Fuller PM (2014) The GABAergic parafacial zone is a medullary slow wave sleep-promoting center. Nat Neurosci 17:1217–1224. https://doi.org/10.1038/nn.3789
Yokota S, Kaur S, Vanderhorst VG, Saper CB, Chamberlin NL (2015) Respiratory-related outputs of glutamatergic, hypercapnia-responsive parabrachial neurons in mice. The J Comparative Neurol 523:907–920. https://doi.org/10.1002/cne.23720
Kato T, Rompré P, Montplaisir JY, Sessle BJ, Lavigne GJ (2001) Sleep bruxism: an oromotor activity secondary to micro-arousal. J Dent Res 80(10):1940–4. https://doi.org/10.1177/00220345010800101501
Khoury S, Rouleau GA, Rompré PH, Mayer P, Montplaisir JY, Lavigne GJ (2008) A significant increase in breathing amplitude precedes sleep bruxism. Chest 134(2):332–337. https://doi.org/10.1378/chest.08-0115
Lavigne GJ, Kato T, Kolta A, Sessle BJ (2003) Neurobiological mechanisms involved in sleep bruxism. Crit Rev Oral Biol Med 14(1):30–46. https://doi.org/10.1177/154411130301400104
Lavigne GJ, Rompré PH, Poirier G, Huard H, Kato T, Montplaisir JY (2001) Rhythmic masticatory muscle activity during sleep in humans. J Dent Res 80(2):443–8. https://doi.org/10.1177/00220345010800020801
Lobbezoo F, Naeije M (2001) Bruxism is mainly regulated centrally, not peripherally. J Oral Rehabil 28(12):1085–1091. https://doi.org/10.1046/j.1365-2842.2001.00839.x
Bosi M, Milioli G, Riccardi S, Melpignano A, Vaudano AE, Cortelli P, Poletti V, Parrino L (2018) Arousal responses to respiratory events during sleep the role of pulse wave amplitude. J Sleep Res 27(2):259–267. https://doi.org/10.1111/jsr.12593
Osorio-Forero A, Cardis R, Vantomme G, Guillaume-Gentil A, Katsioudi G, Devenoges C, Fernandez LMJ, Lüthi A (2021) Noradrenergic circuit control of non-REM sleep substates. Curr Biol 31(22):5009-5023 e7. https://doi.org/10.1016/j.cub.2021.09.041
Jones BE, Hassani OK (2013) The role of Hcrt/Orx and MCH neurons in sleep-wake state regulation. Sleep
Portas CM, Bjorvatn B, Ursin R (2000) Serotonin and the sleep/wake cycle: special emphasis on microdialysis studies. Prog Neurobiol 60(1):13–35.https://doi.org/10.1016/s0301-0082(98)00097-5
John J, Wu MF, Boehmer LN, Siegel JM (2004) Cataplexy-active neurons in the hypothalamus: implications for the role of histamine in sleep and waking behavior. Neuron 42(4):619–634
Andrisani G, Andrisani G (2015) The mesencephalic nucleus of the trigeminal nerve and the SIDS. Med Hypotheses 84(1):8–10. https://doi.org/10.1016/j.mehy.2014.11.005
Moon RY, Tanabe KO, Yang DC, Young HA, Hauck FR (2012) Pacifier use and SIDS: evidence for a consistently reduced risk. Matern Child Health J 16(3):609–614. https://doi.org/10.1007/s10995-011-0793-x
Bucca C, Cicolin A, Brussino L, Arienti A et al (2006) Tooth loss and obstructive sleep apnoea. Respir Res 7(1):8. https://doi.org/10.1186/1465-9921-7-8
Cillo JE Jr, Schorr R, Dattilo DJ (2020) Edentulism is associated with more severe obstructive sleep apnea syndrome. J Oral Maxillofac Surg 78(6):1013–1016. https://doi.org/10.1016/j.joms.2020.02.012
Endeshaw YW, Katz S, Ouslander JG, Bliwise DL (2004) Association of denture use with sleep-disordered breathing among older adults. J Public Health Dent Summer 64(3):181–183. https://doi.org/10.1111/j.1752-7325.2004.tb02749.x
Sanders AE, Akinkugbe AA, Slade GD, Essick GK (2016) Tooth loss and obstructive sleep apnea signs and symptoms in the US population. Sleep Breath 20(3):1095–102. https://doi.org/10.1007/s11325-015-1310-z
Burgos-Sanchez C, Jones NN, Avillion M, Gibson SJ, Patel JA, Neighbors J, Zaghi S, Camacho M (2020) Impact of alcohol consumption on snoring and sleep apnea: a systematic review and meta-analysis. Otolaryngol Head Neck Surg 163(6):1078–1086. https://doi.org/10.1177/0194599820931087
Esen AD, Akpinar M (2021) Relevance of obstructive sleep apnea and smoking: Obstructivs sleep apnea and smoking. Fam Pract 38(2):181–186. https://doi.org/10.1093/fampra/cmaa112
Chakravorty S, Vandrey RG, He S, Stein MD (2018) Sleep management among patients with substance use disorders. Med Clin North Am 102(4):733–743. https://doi.org/10.1016/j.mcna.2018.02.012
Correa D, Farney RJ, Chung F, Prasad A, Lam D, Wong J (2015) Chronic opioid use and central sleep apnea: a review of the prevalence, mechanisms, and perioperative considerations. Anesth Analg 120(6):1273–85. https://doi.org/10.1213/ANE.0000000000000672
Bonsignore MR (2021) Obesity and obstructive sleep apnea. Handb Exp Pharmacol. https://doi.org/10.1007/164_2021_558
Badel T, Savić Pavičin I, Kocijan Lovko S, Zadravec D, Milošević SA, Andreja CA (2021) Alcohol abuse in the dental patient and temporomandibular disorder caused by trauma. Psychiatr Danub Spring-Summer 33(Suppl 4):649–655
Hojo A, Haketa T, Baba K, Igarashi Y (2007) Association between the amount of alcohol intake and masseter muscle activity levels recorded during sleep in healthy young women. Int J Prosthodont 20:251–255
Oleson EB, Hamilton LR, Gomez DM (2021) Cannabinoid modulation of dopamine release during motivation, periodic reinforcement, exploratory behavior, habit formation, and attention. Front Synaptic Neurosci 13:660218
Rintakoski K, Ahlberg J, Hublin C, Broms U, Madden PAF, Könönen M, Koskenvuo M, Lobbezoo F, Kaprio J (2010) Bruxism is associated with nicotine dependence: A nationwide Finnish Twin Cohort Study. Nicotine Tob Res 12:1254–1260
Guichard K, Micoulaud-Franchi J-A, McGonigal A, Coulon P, Sureau C, Ghorayeb I, Salvo F, Philip P (2019) Association of valproic acid with central sleep apnea syndrome: two case reports. J Clin Psychopharmacol
Robillard R, Saad M, Ray LB, BuJáki B, Douglass A, Lee EK, Soucy L, Spitale N (2021) De Koninck, Kendzerska T Selective serotonin reuptake inhibitor use is associated with worse sleep-related breathing disturbances in individuals with depressive disorders and sleep complaints: a retrospective study. J Clin Sleep Med 17(3):505–513. https://doi.org/10.5664/jcsm.8942
Melo G, Dutra KL, Rodrigues Filho R, Ortega AOL, Porporatti AL, Dick B, Flores-Mir C, De Luca Canto G (2018) Association between psychotropic medications and presence of sleep bruxism: A systematic review. J Oral Rehabil 45(7):545–554
Lim R, Messineo L, Grunstein RR, Carberry JC, Eckert DJ (2021) The noradrenergic agent reboxetine plus the antimuscarinic hyoscine butylbromide reduces sleep apnoea severity: a double-blind, placebo-controlled, randomised crossover trial. J Physiol 599(17):4183–4195. https://doi.org/10.1113/JP281912
Chen CY, Chen CL, Yu CC (2021) Trazodone improves obstructive sleep apnea after ischemic stroke: a randomized, double-blind, placebo-controlled, crossover pilot study. J Neurol 268(8):2951–2960. https://doi.org/10.1007/s00415-021-10480-2
Prowting J, Maresh S, Vaughan S, Kruppe E, Alsabri B, Badr MS, Sankari A (1985) 2021 Mirtazapine reduces susceptibility to hypocapnic central sleep apnea in males with sleep-disordered breathing: a pilot study. J Appl Physiol 131(1):414–423. https://doi.org/10.1152/japplphysiol.00838.2020
Sankri-Tarbichi AG, Grullon K, Badr MS (2013) Effects of clonidine on breathing during sleep and susceptibility to central apnoea. Respir Physiol Neurobiol 185(2):356–361. https://doi.org/10.1016/j.resp.2012.09.005
Philbin KE, Bateman RJ, Mendelowitz D (2010) Clonidine, an alpha2-receptor agonist, diminishes GABAergic neurotransmission to cardiac vagal neurons in the nucleus ambiguus. Brain Res 1347:65–70
Stevens DR, Kuramasu A, Eriksson KS, Selbach O, Haas HL (2004) Alpha 2-adrenergic receptor-mediated presynaptic inhibition of GABAergic IPSPs in rat histaminergic neurons. Neuropharmacology. 46(7):1018–22
Miyazaki S, Uchida S, Mukai J, Nishihara K (2004) Clonidine effects on all night human sleep: opposite action of low- and medium-dose clonidine on human NREM-REM sleep proportion. Psychiatry Clin Neurosci 58:138–44
Carra MC, Macaluso GM, Rompré PH, Huynh N, Parrino L, Terzano MG, Lavigne GJ (2010) Clonidine has a paradoxical effect on cyclic arousal and sleep bruxism during NREM sleep. Sleep 33(12):1711–1716. https://doi.org/10.1093/sleep/33.12.1711
Grzanna R, Chee WK, Akeyson EW (1987) Noradrenergic projections to brainstem nuclei: evidence for differential projections from noradrenergic subgroups. J Comp Neurol 263(1):76–91. https://doi.org/10.1002/cne.902630107
Shao YP, Sutin J (1991) Noradrenergic facilitation of motor neurons: localization of adrenergic receptors in neurons and non neuronal cells in the trigeminal motor nucleus. Exp Neurol 114(2):216–27. https://doi.org/10.1016/0014-4886(91)90038-e
Goźlińska B, Czyzewska-Szafran H (1999) Clonidine action in spontaneously hypertensive rats (SHR) depends on the GABAergic system function. Amino Acids 17(2):131–138. https://doi.org/10.1007/BF01361876
Jastrzebski Z, Czyzewska-Szafran H, Goźlińska B, Remiszewska M, Mazurek AP (1995) Clonidine hypotension in spontaneously hypertensive rats (SHR) depends on the functional state of GABAergic and glutamatergic systems. Neurosci Lett 184(2):94–96. https://doi.org/10.1016/0304-3940(94)11177-k
Jastrzebski Z, Goźlińska B, Czyzewska-Szafran H (1993) Pharmacodynamic interaction of clonidine and muscimol in hypertension. Res Commun Chem Pathol Pharmacol 81(1):113–116
Cao W, Luo J, Huang R, Xiao Y (2022) The association between sleep breathing impairment index and cardiovascular risk in male patients with obstructive sleep apnea. Nat Sci Sleep 14:53–60. https://doi.org/10.2147/NSS.S343661. eCollection 2022
Hartmann S, Ferri R, Bruni O, Baumert M (2021) Causality of cortical and cardiovascular activity during cyclic alternating pattern in non-rapid eye movement sleep. Philos Trans A Math Phys Eng Sci 379(2212):20200248. https://doi.org/10.1098/rsta.2020.0248
Kondo H, Ozone M, Ohki N, Sagawa Y, Yamamichi K et al (2014) Association between heart rate variability, blood pressure and autonomic activity in cyclic alternating pattern during sleep. Sleep 37(1):187–94. https://doi.org/10.5665/sleep.3334
Kuriachan VP, Sumner GL, Mitchell LB (2015) Sudden cardiac death. Curr Probl Cardiol 40(4):133–200. https://doi.org/10.1016/j.cpcardiol.2015.01.002
Brooks JG (1982) Apnea of infancy and sudden infant death syndrome. Am J Dis Child
Charoenpan P, Muntarbhorn K, Boongird P, Puavilai G, Ratanaprakarn R, Indraprasit S, Tanphaichitr V, Likittanasombat K, Varavithya W, Tatsanavivat P (1994) Nocturnal physiological and biochemical changes in sudden unexplained death syndrome: a preliminary report of a case control study. Southeast Asian J Trop Med Public Health. 25(2):335–40
Ottaviani G, Buja LM (2020) Pathology of unexpected sudden cardiac death: obstructive sleep apnea is part of the challenge. Cardiovasc Pathol. 47:107221. https://doi.org/10.1016/j.carpath.2020.107221
Galland BC (2014) Elder DE Sudden unexpected death in infancy: biological mechanisms. Paediatr Respir Rev 15(4):287–292. https://doi.org/10.1016/j.prrv.2014.09.003
De-Carolis C, Boyd GA, Mancinelli L, Pagano S, Eramo S (2015) Methamphetamine abuse and “meth mouth” in Europe. Med Oral Patol Oral Cir Bucal 20:e205–e210
Goldstein G, DeSantis L, Goodacre C (2021) Bruxism: best evidence consensus statement. J Prosthodont 30(S1):91–101
Teoh L, Moses G, McCullough MJ (2019) Oral manifestations of illicit drug use. Aust Dent J 64:213–222
Acknowledgements
We thank Prof. Parrino Liborio for granting us the use of the figures in our paper.
Author information
Authors and Affiliations
Contributions
I. Andrisani Giovanni: research, pathology study, theory development, and writing.
ii. Andrisani Giorgia: research pathology study, theory development, and writing.
Corresponding author
Ethics declarations
Ethics approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent for publication
All authors give their unconditional consent to the publication of this article.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The article has not been presented at conferences and has no clinical trial registration number (it is a review article).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Andrisani, G., Andrisani, G. Sleep apnea pathophysiology. Sleep Breath 27, 2111–2122 (2023). https://doi.org/10.1007/s11325-023-02783-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-023-02783-7