Abstract
Objectives
To observe the efficacy and side effects of liraglutide in the treatment of type 2 diabetes mellitus (T2DM) patients with severe obstructive sleep apnea (OSA).
Methods
The study conducted in an outpatient setting was a two-center, prospective randomized controlled study. T2DM patients with severe OSA were randomized to the control group (continuous positive airway pressure [CPAP] and drug treatment without liraglutide) or the liraglutide group (CPAP and drug treatment including liraglutide). Demographic and clinical characteristics, sleep-disordered breathing indices, cardiac function indices, and side effects were evaluated and compared between the two groups before and after 3 months.
Results
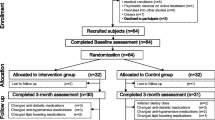
Of 90 patients, 45 were randomized to the intervention arm (with liraglutide) and 45 to the control arm (without liraglutide). One patient in the liraglutide group dropped out of the study on day 8 after enrollment due to obvious gastrointestinal symptoms. No significant differences were found between the two groups in baseline demographics, clinical characteristics, cardiac function indicators, or sleep disorder respiratory indices (P > 0.05). After 3 months, the body mass index (BMI), apnea hypopnea index (AHI), and mean systolic blood pressure in the liraglutide treatment group were significantly lower than those in the control group (P < 0.05). The minimum oxygen saturation was significantly higher in the liraglutide group compared with that in the control group after 3 months of follow-up (P < 0.05). No difference was found between the two groups in the summary of side effects (P > 0.05).
Conclusions
Liraglutide combined with CPAP can effectively reduce BMI, lower mean systolic blood pressure, and improve AHI scores and hypoxia in T2DM patients with severe OSA. Liraglutide did not increase side effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Severe obstructive sleep apnea (OSA) is often associated with insulin resistance, which increases the risk of type 2 diabetes mellitus (T2DM) in patients with OSA. Untreated OSA can affect glycemic control, increase the incidence of cardiovascular and cerebrovascular diseases in patients with OSA patients and T2DM, and affect the prognosis of OSA with T2DM [1]. The latest research suggests that diabetics who are treated with insulin are at higher risk for OSA. The prevalence of OSA in patients with T2DM with obesity has been reported to be 26 to 83% [2,3,4]. There is a bidirectional relationship between OSA and T2DM [5]. Intensive lifestyle interventions, diet control, weight loss, and continuous positive airway pressure (CPAP) are all current treatment options for patients with severe OSA [6]. Currently considered effective treatment outcomes include diet, exercise, and/or CPAP [7]. However, patients have difficulty adhering to these treatment routes long-term, especially weight loss interventions [8]. CPAP may also lead to weight gain, further exacerbating metabolic complications [9, 10]. Therefore, the optimal treatment for the patients with T2DM and severe OSA is to provide glucose control and weight loss interventions in addition to CPAP. Obesity and insulin resistance are often seen in patients with T2DM and severe OSA, which is the theoretical basis for providing liraglutide treatment for these patients. We investigated the effects and safety of liraglutide regarding sleep apnea indicators, weight control, cardiac function, and glycolipid metabolism in patients with T2DM and severe OSA.
Methods
This study was registered in Science and Technology Bureau of Shenzhen Yantian District (No. 20180329). The Ethics Committee of Shenzhen Yantian People’s Hospital approved the study in accordance with the principles of the Declaration of Helsinki. It was a randomized, controlled, nonblinded clinical trial in patients with T2DM and severe OSA. The clinical trial was conducted in Shenzhen Yantian District People’s Hospital and Longyan First Hospital Affiliated to Fujian Medical University from July 2019 to September 2021. All patients visited the clinic once a month for a follow-up period of up to 3 months.
Patient enrollment
From July 2019 to September 2021, patients with T2DM and severe OSA (AHI > 15) were recruited from clinics at Shenzhen Yantian People’s Hospital and Longyan First Hospital Affiliated to Fujian Medical University. All patients who participated in this study provided informed consent.
Inclusion criteria were:
-
1.
Age 18–75 years;
-
2.
Clinical diagnosis of T2DM;
-
3.
Severe OSA with apnea-hypopnea index (AHI) > 15 by polysomnography;
-
4.
No current use of DPP-IV inhibitors or GLP-1RA treatment;
-
5.
Current use of CPAP treatment.
Exclusion criteria were:
-
1.
Pregnant, breastfeeding, or planning to become pregnant soon;
-
2.
Contraindication for DPP-IV inhibitors or GLP1-RAs;
-
3.
Heart failure class III–IV;
-
4.
Chronic kidney disease stage 4 and stage 5;
-
5.
History of pancreatitis;
-
6.
Infections, trauma, hyperthyroidism, hypothyroidism, or malignant tumors;
-
7.
Reluctance to follow up or participation in other clinical trials simultaneously.
The patients were followed up in the outpatient clinic once per month and prescribed medication. One patient in the liraglutide group refused to continue the study because of nausea and vomiting on day 8. All follow-up and data collection were completed in the remaining 89 patients.
Study protocol and measures (Fig. 1)
Control group (no intervention)
The control group was not given a placebo. If conventional hypoglycemic drugs (excluding liraglutide) were given for poor blood glucose control, the type or dosage of the drugs could be adjusted these adjustments were recorded. All patients were treated with CPAP for OSA.
Liraglutide group
Liraglutide was injected subcutaneously once daily into the abdomen, thigh, or upper arm. It was commenced at a starting dose of 0.6 mg once per day. The dose was increased to 1.2 mg/day after 1 week and 1.8 mg/day after the second week. Those who did not tolerate the increased dose continued to maintain the original dose of 0.6 mg/day or 1.2 mg/day. If the drug was tolerated, the patient was required to maintain the maximum tolerated dose. All adjustments occurred under the guidance of the research team. Patients continued CPAP treatment during this period.
Clinical characteristics
Measurements recorded at baseline and follow-up included body mass index (BMI), blood pressure, uric acid levels, blood lipid levels, HbA1c levels, and medication use (hypertension, diabetes, and hyperlipidemia medications).
Detection of cardiac function indicators
The left ventricular ejection fraction (LVEF) and left ventricular end-diastolic diameter (LVEDd) were measured by echocardiography at baseline and after 3 months of follow-up. M-type echocardiography was used to measure LVEF.
Sleep-disordered breathing indices
At baseline and after 3 months of follow-up, polyrespiratory sleep monitoring was performed, and AHI and minimum nocturnal oxygen saturation were recorded.
Summary of the indicators of side effects
Side effects including gastrointestinal complaints, hypoglycemia, pancreatitis, and dermatitis during treatment with liraglutide were recorded at each follow-up.
Follow-up
Follow-up was completed in the outpatient clinic once per month and continued for 3 months.
Statistical analysis
SPSS 19.0 software (SPSS, Chicago, IL) was used for statistical analysis. Continuous variables with a normal distribution are expressed as the mean ± standard deviation (SD), while continuous variables with a non-normal distribution are expressed as the median and quartile difference. Categorical variables are expressed in absolute values and percentages. For comparison between the two groups, Student’s t test was used for normally distributed values, and the Mann‒Whitney U test was used for non-normally distributed values. Categorical variables were compared using the chi-square test or Fisher’s exact test. Intragroup (before and after 3 months of treatment) comparisons, including comparisons of the liraglutide group and control group, were performed by paired sample t tests (when continuous variables followed a normal distribution) and Wilcoxon tests (when continuous variables followed a non-normal distribution). P < 0.05 (2-tailed) was considered statistically significant.
Results
Baseline clinical data
Demographic and clinical data are summarized in Table 1. There were no significant differences in demographic and clinical characteristics at baseline between the control group and the liraglutide group (P > 0.05) (Table 1). Of the 90 patients in this study, one patient in the liraglutide group dropped out because of significant gastrointestinal discomfort giving a lost to follow-up rate of 1.1%.
Cardiac functions
The LVEF and LVEDd values at baseline and 3 months after randomization were measured to estimate cardiac function. The LVEF and LVEDd values were not significantly different between the control group and the liraglutide group at baseline and 3 months after randomization (P > 0.05) (Table 2).
Sleep-disordered breathing indices
At baseline, there was no significant difference in AHI and minimum oxygen saturation between the two groups, but after 3 months of randomization, the liraglutide group had significantly better AHI and minimum oxygen saturation than the control group (P < 0.05). The AHI and minimum oxygen saturation values were also significantly better in the liraglutide group after 3 months of treatment than at baseline (P < 0.05) (Table 3).
Indicators of cardiovascular risk
BMI, blood lipids, uric acid, HbA1c, and 24-h ambulatory blood pressure were measured after 3 months of follow-up. The BMI and 24-h mean systolic blood pressure (SBP) values were lower in the liraglutide group than in the control group after the 3-month follow-up (P < 0.05). The BMI, CHOL, LDL, HbA1c and 24-h ambulatory blood pressure values were significantly improved in the liraglutide group after 3 months compared with baseline, and the BMI and HbA1c values in the control group were also improved after 3 months compared with baseline (Table 4).
Summary of the indicators of side effects
No pancreatitis occurred during treatment with liraglutide at any follow-up timepoint. No significant differences in the occurrence of gastrointestinal complaints, hypoglycemia, or dermatitis were found between the two groups (P > 0.05) (Table 5).
Discussion
Liraglutide is a hypoglycemic agent used to treat T2DM. It is a glucagon-like peptide-1 receptor agonist (GLP-1RA) and can also be used in weight loss therapy [11]. A dose of 1.8 mg/day is commonly used to treat diabetes, while a dose of 3.0 mg/day or higher is used for weight control. The highest dose used in this study was 1.8 mg/day. OSA is often associated with T2DM. As a routine treatment for OSA, CPAP has the risk of affecting metabolism, and patients have poor compliance with CPAP treatment. Therapies that benefit both OSA and T2DM patients are important. Weight loss is beneficial for controlling blood sugar levels and improving OSA. Our study suggested that liraglutide, a GLP-RA, is a hypoglycemic agent associated with significant weight loss that improves the severity of OSA in T2DM patients.
Several large studies in patients with diabetes have found that liraglutide improves blood sugar control and leads to significant weight loss [12]. The SCALE diabetes trial involving obese patients (BMI greater than 27) showed that liraglutide given subcutaneously at 3.0 and 1.8 mg resulted in 6% and 5% weight loss, respectively, compared to placebo. In our study, the maximum intervention dose of liraglutide was 1.8 mg once daily. The results showed a 2.0 decrease in BMI in the liraglutide group. These results suggested that liraglutide 1.8 mg once a day has a good effect on weight loss in the Chinese population. The weight loss effect of liraglutide is primarily achieved through appetite suppression mediated by peripheral and central nervous system (CNS) pathways. It can directly stimulate POMC neurons while inhibiting arcuate nucleus neuropeptide y (NPY) and AgRP neurons, reducing hunger and increasing satiety [13]. This feeling of fullness can also have an effect on other areas of the brain, such as the mesolimbic system. These effects lead to a loss of appetite and feelings of nausea. Therefore, liraglutide injections reduce stomach motility and slow the emptying of stomach contents, affecting food intake and leading to weight loss [14, 15]. The latest study showed that 5% weight loss did not affect the risk of cardiovascular events, but 10% weight loss was enough to reduce cardiovascular events [16]. Although BMI decreased significantly, lipid levels, uric acid levels, glycosylated hemoglobin levels, and cardiac function indicators did not improve significantly in our study, which was the result of 3-month follow-up. Longer follow-up studies are needed to confirm whether liraglutide treatment can improve blood lipid, uric acid, glycated hemoglobin levels, and other indicators. However, our study also showed that the 24-h mean SBP in the liraglutide group was significantly lower than that in the control group. This may be due to improvements in AHI and minimum oxygen saturation values at night.
The SCALE sleep apnea study showed weight loss and improved AHI scores in the liraglutide group, which was consistent with the conclusions of this study [17]. In addition, liraglutide improved the minimum blood oxygen saturation in patients with severe OSA and T2DM [18]. There is a strong association between obesity and OSA. Risk factors for OSA include tonsil and adenoid hypertrophy and obesity, which may lead to upper airway stenosis or obstruction [19]. Corrado Pelaia found in their study that BMI was closely related to neck circumference, waist circumference [20], peripheral oxygen saturation, and AHI scores [21]. Additional studies have shown that regular physical activity may reduce the occurrence of severe OSA in an evidence-based way through weight loss [22]. Our study showed significant weight loss in the liraglutide group, which may reduce adipose tissue compression of the upper airway or prevent airway collapse. This improves OSA severity, reduces AHI scores, and increases nighttime minimum oxygen saturation. More studies are needed to determine if liraglutide improves the sleep disorder respiratory index in other ways.
OSA is a risk factor for hypertension, coronary heart disease, arrhythmia, heart failure, stroke, and other cardiovascular and cerebrovascular diseases [23, 24]. The underlying mechanism of the association between OSA and cardiovascular disease is not yet fully understood. The current first-line treatment for OSA is CPAP. However, there are some problems. First, the results from randomized controlled trials suggest that CPAP therapy does not reduce the incidence of cardiovascular disease [25]. Second, there is the concern of long-term adherence to CPAP therapy. This study suggests that liraglutide, as a GLP-RA and a hypoglycemic agent associated with weight loss for the treatment of type 2 diabetes, may improve OSA severity. This study suggests that liraglutide, as a GLP-RA and a hypoglycemic agent associated with weight loss, may improve OSA severity in patients with T2DM. However, whether or not liraglutide improves cardiovascular risk factors in T2DM patients with severe OSA remains unclear. Some studies have shown that liraglutide improves various cardiometabolic parameters in obese and prediabetic patients, reducing the risk of diabetes [26]. Our study showed that after 3 months of liraglutide intervention, the mean SBP in patients with OSA and T2DM was controlled. However, no significant difference was found in the average SBP, blood lipid level, glycosylated hemoglobin level, and uric acid level in the liraglutide group, which may be related to the insufficient liraglutide intervention time and the small sample size of this study.
GLP-1 agonists and analogs have been reported to be well tolerated. Nausea is the most common symptom of discomfort during early liraglutide treatment [27]. Although this side effect is not a serious health concern, it may cause patients to stop liraglutide treatment [28]. Liraglutide is associated with hypoglycemic risk, but severe hypoglycemic episodes were rarely reported in the LEAD study. In our study, there was no difference in the incidence of gastrointestinal discomfort, hypoglycemia, or dermatitis between the two groups.
Although these results are novel, there are limitations to our study that need to be considered. First, despite being a two-center study, the sample size was not large, which limits the ability to generalize the findings. Second, follow-up time was limited and the effects on lipids, blood sugar, and other indicators need to be confirmed by longer term follow-up studies. Third, our findings cannot be generalized to patients with mild OSA because only patients with severe OSA were enrolled.
Conclusion
Liraglutide is a glucose-lowering drug used in patients with T2DM and for weight loss in obese patients. In our study, liraglutide combined with CPAP improved the severity of OSA, lowered BMI and mean SPB values in patients with T2DM and severe OSA, and did not increase hypoglycemic side effects.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Devaraj NK (2020) Knowledge, attitude, and practice regarding obstructive sleep apnea among primary care physicians. Sleep and Breathing 24(4):1581–1590
Coughlin SR, Mawdsley L, Mugarza JA et al (2004) Obstructive sleep apnoea is independently associated with an increased prevalence of metabolic syndrome. Eur Heart J 25:735–741
Foster GD, Sanders MH, Millman R et al (2009) Obstructive sleep apnea among obese patients with type 2 diabetes. Diabetes Care 32:1017–1019
West SD, Nicoll DJ, Stradling JR (2006) Prevalence of obstructive sleep apnoea in men with type 2 diabetes. Thorax 61:945–950
Huang T, Lin BM, Stampfer MJ et al (2018) A population-based study of the bidirectional association between obstructive sleep apnea and type 2 diabetes in three prospective US cohorts. Diabetes Care 41:2111–9
Giles TL, Lasserson TJ, Smith BH et al (2006) Continuous positive airways pressure for obstructive sleep apnoea in adults. Cochrane Database Syst Rev CD001106
Foster GD, Borradaile KE, Sanders MH et al (2009) A randomized study on the effect of weight loss on obstructive sleep apnea among obese patients with type 2 diabetes: the sleep ahead study. Arch Intern Med 169:1619–1626
Ashrafian H, le Roux CW, Rowland SP et al (2012) Metabolic surgery and obstructive sleep apnoea: the protective effects of bariatric procedures. Thorax 67:442–449
Craig SE, Kohler M, Nicoll D et al (2012) Continuous positive airway pressure improves sleepiness but not calculated vascular risk in patients with minimally symptomatic obstructive sleep apnoea: the mosaic randomised controlled trial. Thorax 67:1090–1096
Drager LF, Brunoni AR, Jenner R et al (2015) Effects of CPAP on body weight in patients with obstructive sleep apnoea: a meta-analysis of randomised trials. Thorax 70:258–264
Food and Drug Administration. Prescribing information for Saxenda, 2018 [Internet]. Maryland: Food and Drug Administration; 2018 [cited 2020 May 29]
Buse JB, Nauck M, Forst T et al (2013) Exenatide once weekly versus liraglutide once daily in patients with type 2 diabetes (DURATION-6): a randomised, open-label study. Lancet 381(9861):117–124
Secher A, Jelsing J, Baquero AF et al (2014) The arcuate nucleus mediates GLP-1 receptor agonist liraglutide-dependent weight loss. J Clin Invest 124(10):4473–4488
Dailey MJ, Moran TH (2013) Glucagon-like peptide 1 and appetite. Trends Endocrinol Metab 24(2):85–91
Williams DL, Baskin DG, Schwartz MW (2009) Evidence that intestinal glucagon-like peptide-1 plays a physiological role in satiety. Endocrinology 150(4):1680–1687
Wing RR, Lang W, Wadden TA et al (2011) Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care 34(7):1481–1486
Collier A, Blackman A, Foster G et al (2014) S28 liraglutide 3.0 mg reduces severity of obstructive sleep apnoea and body weight in obese individuals with moderate or severe disease: Scale Sleep Apnoea Trial. BMJ Publishing Group Ltd
Patinkin ZW, Feinn R, Santos M (2017) Metabolic consequences of obstructive sleep apnea in adolescents with obesity: a systematic literature review and meta-analysis. Child Obes 13(2):102–110
Khan MA, Mathur K, Barraza G et al (2020) The relationship of hypertension with obesity and obstructive sleep apnea in adolescents. Pediatr Pulmonol 55(4):1020–1027
Pelaia C, Armentaro G, Miceli S et al (2021) Association between sleep apnea and valvular heart diseases. Front Med (Lausanne) 9(8):667522
Rezaie L, Maazinezhad S, Fogelberg DJ, Khazaie H, Sadeghi-Bahmani D, Brand S (2021) Compared to individuals with mild to moderate obstructive sleep apnea (OSA), individuals with severe OSA had higher BMI and respiratory-disturbance scores. Life (Basel) 11(5):368
Hall KA, Singh M, Mukherjee S, Palmer LJ (2020) Physical activity is associated with reduced prevalence of self-reported obstructive sleep apnea in a large, general population cohort study. J Clin Sleep Med 16:1179–2118
Urbanik D, Martynowicz H, Mazur G et al (2020) Environmental factors as modulators of the relationship between obstructive sleep apnea and lesions in the circulatory system. J Clin Med 9:836
Tietjens JR, Claman D, Kezirian EJ, Yeghiazarians Y et al (2019) Obstructive sleep apnea in cardiovascular disease: a review of the literature and proposed multidisciplinary clinical management strategy. J Am Heart Assoc 8:e010440
Labarca G, Dreyse J, Drake L, Jorquera J, Barbe F (2020) Efficacy of continuous positive airway pressure (CPAP) in the prevention of cardiovascular events in patients with obstructive sleep apnea: systematic review and meta-analysis. Sleep Med Rev 52:101312
Rezaie L, Phillips D, Khazaie H (2018) Barriers to acceptance and adherence to continuous positive airway pressure therapy in patients with obstructive sleep apnea: a report from Kermanshah province, western Iran. Patient Prefer Adherence 12:1299–1304
Pi-Sunyer X, Astrup A, Fujioka K et al (2015) A randomized, controlled trial of 3.0 mg of liraglutide in weight management. N Engl J Med 373(1):11–22
Buse JB, Rosenstock J, Sesti G et al (2009) Liraglutide once a day versus exenatide twice a day for type 2 diabetes: a 26-week randomised, parallel-group, multinational, open-label trial (LEAD-6). Lancet 374(9683):39–47
Acknowledgements
This work was supported by the Department of Cardiovascular, Shenzhen Yantian People’s Hospital, Shenzhen, China, and the Department of Cardiovascular, Longyan First Hospital Affiliated to Fujian Medical University, Fujian, China.
Funding
This study was supported by Shenzhen Yantian District Science and Technology Bureau (20180239).
Author information
Authors and Affiliations
Contributions
Design of the study: WL J. Data searches: WL J, WG L, and J C. Analysis of data: WL J and FZ C. Writing — original draft preparation: WL J. Writing — review and editing: WL J and FZ C. Writing — final version: FZ C. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Shenzhen Yantian People’s Hospital and was conducted according to the principles of the Declaration of Helsinki.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jiang, W., Li, W., Cheng, J. et al. Efficacy and safety of liraglutide in patients with type 2 diabetes mellitus and severe obstructive sleep apnea. Sleep Breath 27, 1687–1694 (2023). https://doi.org/10.1007/s11325-022-02768-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-022-02768-y