Abstract
Purpose
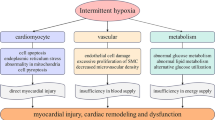
Patients with obstructive sleep apnoea (OSA) have a high incidence of vascular endothelial injury. The most important pathophysiological feature of OSA is chronic intermittent hypoxia (CIH). This study aimed to investigate the mechanisms of CIH-related vascular endothelial injury.
Methods
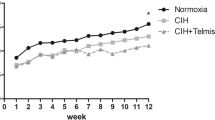
IH exposure was applied to human umbilical vein endothelial cells (HUVECs). After modeling, cell viability, the expression levels of peroxisome proliferator activated receptor γ (PPARγ), apoptosis-associated proteins and mitochondrial division fusion proteins, and the levels of reactive oxygen species (ROS) and mitochondrial membrane potential (MMP) were assessed via Cell Counting Kit-8 (CCK-8), western blotting, fluorescent microscope, and flow cytometry, respectively. Rosiglitazone (PPARγ agonist), tempo (the mitochondrial-specific antioxidant), and tempo combined with PPARγ interfering RNA were used to treat HUVECs, respectively.
Results
After IH exposure, cell viability and levels of MMP decreased, cell apoptosis and ROS levels increased, and the expression levels of PPARγ decreased. Both tempo and rosiglitazone pretreatment ameliorated cell apoptosis and improved cell viability. In addition, mitochondrial function became better after tempo pretreatment. PPARγ interference reversed the protective effects of tempo on IH-related mitochondrial function injury and cell injury.
Conclusions
PPARγ regulated the apoptosis and cell viability of IH-treated HUVECs by altering mitochondrial function. This finding clarifies the mechanism of CIH-related vascular endothelial injury.






Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Gottlieb DJ, Punjabi NM (2020) Diagnosis and management of obstructive sleep apnea: a review. JAMA 323:1389–1400
Sharma S, Stansbury R, Hackett B, Fox H (2021) Sleep apnea and pulmonary hypertension: a riddle waiting to be solved. Pharmacol Ther 227:107935
Adir Y Humbert M Chaouat A (2021) Sleep-related breathing disorders and pulmonary hypertension. Eur Respir J 57
Chang HP, Chen YF, Du JK (2020) Obstructive sleep apnea treatment in adults. Kaohsiung J Med Sci 36:7–12
Coniglio AC, Mentz RJ (2020) Sleep breathing disorders in heart failure. Heart Fail Clin 16:45–51
Zinchuk A, Yaggi HK (2020) Phenotypic subtypes of OSA: a challenge and opportunity for precision medicine. Chest 157:403–420
De Silva TM, Li Y, Kinzenbaw DA, Sigmund CD, Faraci FM (2018) Endothelial PPARγ (peroxisome proliferator-activated receptor-γ) is essential for preventing endothelial dysfunction with aging. Hypertension 72:227–234
Lian N Chen M Zhang S Chen L Huang J Lin Q (2021) Decreased expression of PPARγ is associated with aortic endothelial cell apoptosis in intermittently hypoxic rats. Sleep and Breathing
Mukohda M (2019) Role of PPARγ, a transcription factor in cardiovascular disease. Nihon Yakurigaku Zasshi 154:56–60
Hu C, Lu KT, Mukohda M, Davis DR, Faraci FM, Sigmund CD (2016) Interference with PPARγ in endothelium accelerates angiotensin II-induced endothelial dysfunction. Physiol Genomics 48:124–134
McDonnell MJ, Aliberti S, Goeminne PC, Restrepo MI, Finch S, Pesci A, Dupont LJ, Fardon TC, Wilson R, Loebinger MR, Skrbic D, Obradovic D, De Soyza A, Ward C, Laffey JG, Rutherford RM, Chalmers JD (2016) Comorbidities and the risk of mortality in patients with bronchiectasis: an international multicentre cohort study. Lancet Respir Med 4:969–979
Yeligar SM, Kang BY, Bijli KM, Kleinhenz JM, Murphy TC, Torres G, San Martin A, Sutliff RL, Hart CM (2018) PPARγ Regulates mitochondrial structure and function and human pulmonary artery smooth muscle cell proliferation. Am J Respir Cell Mol Biol 58:648–657
Toffoli S, Roegiers A, Feron O, Van Steenbrugge M, Ninane N, Raes M, Michiels C (2009) Intermittent hypoxia is an angiogenic inducer for endothelial cells: role of HIF-1. Angiogenesis 12:47–67
Osman AM, Carter SG, Carberry JC, Eckert DJ (2018) Obstructive sleep apnea: current perspectives. Nat Sci Sleep 10:21–34
Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip MSM, Morrell MJ, Nunez CM, Patel SR, Penzel T, Pépin JL, Peppard PE, Sinha S, Tufik S, Valentine K, Malhotra A (2019) Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med 7:687–698
Chen YC Hsu PY Hsiao CC Lin MC (2019) Epigenetics: a potential mechanism involved in the pathogenesis of various adverse consequences of obstructive sleep apnea. Int J Mol Sci 20
Javaheri S, Barbe F, Campos-Rodriguez F, Dempsey JA, Khayat R, Malhotra A, Martinez-Garcia MA, Mehra R, Pack AI, Polotsky VY, Redline S, Somers VK (2017) Sleep apnea: types, mechanisms, and clinical cardiovascular consequences. J Am Coll Cardiol 69:841–858
Ketsawatsomkron P, Sigmund CD (2015) Molecular mechanisms regulating vascular tone by peroxisome proliferator activated receptor gamma. Curr Opin Nephrol Hypertens 24:123–130
Di BB, Li HW, Li WP, Shen XH, Sun ZJ, Wu X (2015) Pioglitazone inhibits high glucose-induced expression of receptor for advanced glycation end products in coronary artery smooth muscle cells. Mol Med Rep 11:2601–2607
Legchenko E Chouvarine P Borchert P Fernandez-Gonzalez A Snay E Meier M Maegel L Mitsialis SA Rog-Zielinska EA Kourembanas S Jonigk D Hansmann G (2018) PPARgamma agonist pioglitazone reverses pulmonary hypertension and prevents right heart failure via fatty acid oxidation. Sci Transl Med 10
Zhong CB, Chen X, Zhou XY, Wang XB (2018) The role of peroxisome proliferator-activated receptor γ in mediating cardioprotection against ischemia/reperfusion injury. J Cardiovasc Pharmacol Ther 23:46–56
Rakhshandehroo M Knoch B Müller M Kersten S (2010) Peroxisome proliferator-activated receptor alpha target genes. PPAR Res 2010
Pezzuto A, Carico E (2018) Role of HIF-1 in cancer progression: novel insights. A review Curr Mol Med 18:343–351
De Nuccio C Bernardo A Troiano C Brignone MS Falchi M Greco A Rosini M Basagni F Lanni C Serafini MM Minghetti L Visentin S (2020) NRF2 and PPAR-γ pathways in oligodendrocyte progenitors: focus on ROS protection mitochondrial biogenesis and promotion of cell differentiation. Int J Mol Sci 21
Giampietro L, Gallorini M, De Filippis B, Amoroso R, Cataldi A, di Giacomo V (2019) PPAR-γ agonist GL516 reduces oxidative stress and apoptosis occurrence in a rat astrocyte cell line. Neurochem Int 126:239–245
Vallée A, Lecarpentier Y (2018) Crosstalk between peroxisome proliferator-activated receptor gamma and the canonical WNT/β-catenin pathway in chronic inflammation and oxidative stress during carcinogenesis. Front Immunol 9:745
Funding
This study was funded by Fujian Province Finance Project of China (No. BPB-LNF2021) and Joint Funds for the innovation of science and Technology, Fujian Province [Grant number. 2019Y9116].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This paper was presented as a poster at the 3rd Congress of Asian Society of Sleep Medicine.
Lian NF, Chen MX, Chen LD, Huang JF, Lin QC (Corresponding author). PPARγ regulates mitochondrial function and cell injury in intermittent hypoxia treated human umbilical vein endothelial cells. ASSM 2021 Meet.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ning-fang, L., Yong-xu, J., Jia, C. et al. The role of PPARγ in intermittent hypoxia-related human umbilical vein endothelial cell injury. Sleep Breath 27, 1155–1164 (2023). https://doi.org/10.1007/s11325-022-02696-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-022-02696-x