Abstract
Purpose
The impact of obstructive sleep apnea syndrome (OSAS) in terms of mortality, morbidity, and quality of life has been well established. Phenotyping OSAS is essential in order to make the best therapeutic choice. A particular subset of patients with OSAS shows nocturnal respiratory failure, defined by a nighttime oxygen saturation <90% in more than 30% of the total sleep time (TST90). The aim of this study was to identify possible predictive factors for nighttime respiratory failure (NRF) in patients with OSAS.
Methods
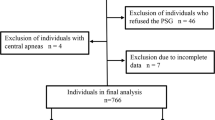
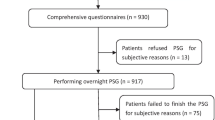
In this retrospective study, patients with suspected OSAS who underwent a sleep study were enrolled. Of 116 patients with moderate/severe OSAS who met the inclusion criteria, 67 also had nocturnal respiratory failure. We compared clinical, anthropometric, and laboratory data in patients with OSAS vs. OSAS and nocturnal respiratory failure.
Results
Patients with OSAS and nocturnal respiratory failure were more frequently female, had a higher BMI, lower daytime oxygen partial pressure (PaO2) in arterial blood, higher Apnea Hypopnea Index (AHI), and a lower number of sleep hours per night. Chronic obstructive pulmonary disease (COPD) was more diagnosed in the group of patients with nocturnal respiratory failure. A lower number of total sleep hours, lower daytime PaO2, lower AHI, increased oxygen desaturation index (ODI), and the presence of a diagnosed COPD were all found to increase the risk of having nocturnal respiratory failure.
Conclusion
COPD, AHI, ODI, daytime PaO2, and total sleep hours are the main predictors for NRF in patients with moderate and severe OSAS.





Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AUC:
-
Area under the curve
- AHI:
-
Apnea Hypopnea Index
- COPD:
-
Chronic obstructive pulmonary disease
- GERD:
-
Gastroesophageal reflux disease
- IQR:
-
Median and interquartile ranges
- NRF:
-
Nocturnal respiratory failure
- OHS:
-
Obesity hypoventilation syndrome
- OSAS:
-
Obstructive sleep apnea syndrome
- ODI:
-
Oxygen desaturation index
- ROC:
-
Receiver operating characteristic
- SD:
-
Standard deviation
References
Peppard PE, Young T, Barnet JH et al (2013) Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. https://doi.org/10.1093/aje/kws342
Xie C, Zhu R, Tian Y, Wang K (2017) Association of obstructive sleep apnoea with the risk of vascular outcomes and all-cause mortality: a meta-analysis. BMJ Open. https://doi.org/10.1136/bmjopen-2016-013983
Baratta F, Pastori D, Fabiani M et al (2018) Severity of OSAS, CPAP and cardiovascular events: a follow-up study. Eur J Clin Investig. https://doi.org/10.1111/eci.12908
Tarasiuk A, Reuveni H (2013) The economic impact of obstructive sleep apnea. Curr Opin Pulm Med. https://doi.org/10.1097/MCP.0b013e3283659e1e
Sullivan CE, Berthon-Jones M, Issa FG, Eves L (1981) Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. Lancet. https://doi.org/10.1016/S0140-6736(81)92140-1
Rotenberg BW, Murariu D, Pang KP (2016) Trends in CPAP adherence over twenty years of data collection: a flattened curve. J Otolaryngol Head Neck Surg. https://doi.org/10.1186/s40463-016-0156-0
Sutherland K, Kairaitis K, Yee BJ et al (2018) From CPAP to tailored therapy for obstructive sleep Apnoea. Multidiscip Respir Med. https://doi.org/10.1186/s40248-018-0157-0
Zinchuk A, Yaggi HK (2020) Phenotypic subtypes of OSA: a challenge and opportunity for precision medicine. Chest 157:403–420
Levi-Valensi P, Weitzenblum E, Rida Z et al (1992) Sleep-related oxygen desaturation and daytime pulmonary haemodynamics in COPD patients. Eur Respir J
Weitzenblum E, Chaouat A, Charpentier C et al (1997) Sleep-related hypoxaemia in chronic obstructive pulmonary disease: causes, consequences and treatment. Respiration 64:187–193. https://doi.org/10.1159/000196669
Labarca G, Gower J, Lamperti L et al (2020) Chronic intermittent hypoxia in obstructive sleep apnea: a narrative review from pathophysiological pathways to a precision clinical approach. Sleep Breath
Kapur VK, Auckley DH, Chowdhuri S et al (2017) Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American academy of sleep medicine clinical practice guideline. J Clin Sleep Med 13:479–504
Mokhlesi B, Masa JF, Afshar M et al (2019) Evaluation and management of obesity hypoventilation syndrome. An official American Thoracic Society clinical practice guideline. Am J Respir Crit Care Med 200:E6–E24. https://doi.org/10.1164/RCCM.201905-1071ST
McKeon JL, Murree-Allen K, Saunders NA (1988) Prediction of oxygenation during sleep in patients with chronic obstructive lung disease. Thorax 43:312–317. https://doi.org/10.1136/thx.43.4.312
Kapsimalis F, Kryger MH (2002) Gender and obstructive sleep apnea syndrome, part 1: clinical features. Sleep 25:409–416. https://doi.org/10.1093/SLEEP/25.4.409
O'Connor CHRIS, Thornley KS, Hanly PJ (2000) Gender differences in the polysomnographic features of obstructive sleep apnea. Am J Respir Crit Care Med 161:1465–1472. https://doi.org/10.1164/AJRCCM.161.5.9904121
Ware JC, McBrayer RH, Scott JA (2000) Influence of sex and age on duration and frequency of sleep apnea events. Sleep 23:1–6. https://doi.org/10.1093/SLEEP/23.2.1C
Leech JA, Onal E, Dulberg C, Lopata MA (1988) A comparison of men and women with occlusive sleep apnea syndrome. Chest 94:983–988. https://doi.org/10.1378/CHEST.94.5.983
Basoglu OK, Tasbakan MS (2018) Gender differences in clinical and polysomnographic features of obstructive sleep apnea: a clinical study of 2827 patients. Sleep Breath 22:241–249. https://doi.org/10.1007/S11325-017-1482-9
Fletcher EC, Miller J, Divine GW et al (1987) Nocturnal oxyhemoglobin desaturation in COPD patients with arterial oxygen tensions above 60 mm Hg. Chest 92:604–608. https://doi.org/10.1378/chest.92.4.604
Matsumoto T, Murase K, Tabara Y et al (2020) Sleep disordered breathing and metabolic comorbidities across sex and menopausal status in East Asians: the Nagahama study. Eur Respir J 56:1902251. https://doi.org/10.1183/13993003.02251-2019
Lévy P, Pépin JL, Arnaud C, et al (2008) Intermittent hypoxia and sleep-disordered breathing: current concepts and perspectives. Eur Respir J Eur Respir J, 32:1082–1095
Phillips BG, Kato M, Narkiewicz K et al (2000) Increases in leptin levels, sympathetic drive, and weight gain in obstructive sleep apnea. Am J Physiol Heart Circ Physiol 279:279. https://doi.org/10.1152/ajpheart.2000.279.1.h234
Phipps PR, Starritt E, Caterson I, Grunstein RR (2002) Association of serum leptin with hypoventilation in human obesity. Thorax 57:75–76. https://doi.org/10.1136/thorax.57.1.75
Saad MF, Damani S, Gingerich RL et al (1997) Sexual dimorphism in plasma leptin concentration 1. J Clin Endocrinol Metab 82:579–584. https://doi.org/10.1210/jcem.82.2.3739
Thomas T, Burguera B, Melton LJ et al (2000) Relationship of serum leptin levels with body composition and sex steroid and insulin levels in men and women. Metabolism 49:1278–1284. https://doi.org/10.1053/meta.2000.9519
Lusic Kalcina L, Valic M, Pecotic R et al (2017) Good and poor sleepers among OSA patients: sleep quality and overnight polysomnography findings. Neurol Sci 38:1299–1306. https://doi.org/10.1007/s10072-017-2978-6
Mallon L, Broman JE, Hetta J (2005) High incidence of diabetes in men with sleep complaints or short sleep duration: a 12-year follow-up study of a middle-aged population. Diabetes Care 28:2762–2767. https://doi.org/10.2337/diacare.28.11.2762
Taheri S, Lin L, Austin D et al (2004) Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med 1:210–217. https://doi.org/10.1371/journal.pmed.0010062
Gottlieb DJ, Redline S, Nieto FJ et al (2006) Association of usual sleep duration with hypertension: the Sleep Heart Health Study. Sleep 29:1009–1014. https://doi.org/10.1093/sleep/29.8.1009
Meier-Ewert HK, Ridker PM, Rifai N et al (2004) Effect of sleep loss on C-reactive protein, an inflammatory marker of cardiovascular risk. J Am Coll Cardiol 43:678–683. https://doi.org/10.1016/j.jacc.2003.07.050
Budhiraja R, Siddiqi TA, Quan SF (2015) Sleep disorders in chronic obstructive pulmonary disease: etiology, impact, and management. J Clin Sleep Med 11:259–270
Zamarrón C, Paz VG, Morete E, del Campo Matías F (2008) Association of chronic obstructive pulmonary disease and obstructive sleep apnea consequences. Int J COPD 3:671–682
McNicholas WT (2000) Impact of sleep in COPD. Chest 117:48S–53S. https://doi.org/10.1378/chest.117.2_suppl.48S
Calverley PMA, Brezinova V, Douglas NJ et al (1982) The effect of oxygenation on sleep quality in chronic bronchitis and emphysema. Am Rev Respir Dis 126:206–210. https://doi.org/10.1164/arrd.1982.126.2.206
Ganga HV, Nair SU, Puppala VK, Miller WL (2013) Risk of new-onset atrial fibrillation in elderly patients with the overlap syndrome: a retrospective cohort study. J Geriatr Cardiol 10:129–134. https://doi.org/10.3969/j.issn.1671-5411.2013.02.001
Polkey MI, Kyroussis D, Hamnegard CH et al (1996) Diaphragm strength in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 154:1310–1317. https://doi.org/10.1164/ajrccm.154.5.8912741
Begin P, Grassino A (1991) Inspiratory muscle dysfunction and chronic hypercapnia in chronic obstructive pulmonary disease. Am Rev Respir Dis 143:905–912. https://doi.org/10.1164/ajrccm/143.5_pt_1.905
Spruit MA, Gosselink R, Troosters T et al (2003) Muscle force during an acute exacerbation in hospitalised patients with COPD and its relationship with CXCL8 and IGF-I. Thorax 58:752–756. https://doi.org/10.1136/thorax.58.9.752
Carpagnano GE, Kharitonov SA, Foschino-Barbaro MP et al (2004) Supplementary oxygen in healthy subjects and those with COPD increases oxidative stress and airway inflammation. Thorax 59:1016–1019. https://doi.org/10.1136/thx.2003.020768
Davidson AC, Leach R, George RJD, Geddes DM (1988) Supplemental oxygen and exercise ability in chronic obstructive airways disease. Thorax 43:965–971. https://doi.org/10.1136/thx.43.12.965
Connaughton JJ, Catterall JR, Elton RA et al (1988) Do sleep studies contribute to the management of patients with severe chronic obstructive pulmonary disease? Am Rev Respir Dis 138:341–344. https://doi.org/10.1164/ajrccm/138.2.341
Fletcher EC, Donner CF, Midgren B et al (1992) Survival in COPD patients with a daytime PaO2 >60 mm Hg with and without nocturnal oxyhemoglobin desaturation. Chest 101:649–655. https://doi.org/10.1378/chest.101.3.649
Machado MCL, Vollmer WM, Togeiro SM et al (2010) CPAP and survival in moderate-to-severe obstructive sleep apnoea syndrome and hypoxaemic COPD. Eur Respir J 35:132–137. https://doi.org/10.1183/09031936.00192008
Acknowledgements
We thank all the physicians, nurses, and healthcare professionals who gave us great support
during this study.
Author information
Authors and Affiliations
Contributions
Dr Andrea Portacci participated in the design of the study, in the sequence of alignment, in the statistical analysis, and drafted the manuscript. Dr Carla Santomasi participated in the design of the study, in the interpetation of the results, and drafted the manuscript. Dr Valentina Di Lecce participated in the design of the study, in the interpetation of the results, and drafted the manuscript. Dr Federica Barratta participated in the in the literature research and in data acquisition. Dr Maria Luisa De Candia participated in the literature research and in data acquisition. Prof Onofrio Resta participated in the design of the study and in the final revision ot the manuscript. Prof Giovanna Elisiana Carpagnano participated in the design of the study, in the interpetation of the results, and in the final revision ot the manuscript. All authors read and approved the final manuscript. All the authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ethics declarations
Ethics approval
The current study has been approved by Institutional Review Board of teaching Hospital Policlinic of Bari (Ethical Committee number: 6750) and, due to the nature of retrospective study, waived the need for informed consent from individual patients.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 14 kb)
Rights and permissions
About this article
Cite this article
Portacci, A., Santomasi, C., Di Lecce, V. et al. Predictive tools for nocturnal respiratory failure in patients with moderate and severe OSAS. Sleep Breath 27, 611–620 (2023). https://doi.org/10.1007/s11325-022-02666-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-022-02666-3