Abstract
Purpose
Snoring is closely related to obstructive sleep apnea in adults. The increasing abundance and availability of smartphone technology has facilitated the examination and monitoring of snoring at home through snoring apps. However, the accuracy of snoring detection by snoring apps is unclear. This study explored the snoring detection accuracy of Snore Clock—a paid snoring detection app for smartphones.
Methods
Snoring rates were detected by smartphones that had been installed with the paid app Snore Clock. The app provides information on the following variables: sleep duration, snoring duration, snoring loudness (in dB), maximum snoring loudness (in dB), and snoring duration rate (%). In brief, we first reviewed the snoring rates detected by Snore Clock; thereafter, an ear, nose, and throat specialist reviewed the actual snoring rates by using the playback of the app recordings.
Results
In total, the 201 snoring records of 11 patients were analyzed. Snoring rates measured by Snore Clock and those measured manually were closely correlated (r = 0.907). The mean snoring detection accuracy rate of Snore Clock was 95%, with a positive predictive value, negative predictive value, sensitivity, and specificity of 65% ± 35%, 97% ± 4%, 78% ± 25%, and 97% ± 4%, respectively. However, the higher the snoring rates, the higher were the false-negative rates for the app.
Conclusion
Snore Clock is compatible with various brands of smartphones and has a high predictive value for snoring. Based on the strong correlation between Snore Clock and manual approaches for snoring detection, these findings have validated that Snore Clock has the capacity for at-home snoring detection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Snoring, defined as “the vibration of palatal soft tissue from obstruction of air movement on breathing during sleeping,” is believed to be a key indicator of possible obstructive sleep apnea syndrome (OSA) [1]. Snoring prevalence in Asian countries, in descending order, is Taiwan (59%) [2], Malaysia (47%) [3], Turkey (41%) [4], Japan (24% among men and 10% among women) [5], Singapore (7%) [6], and Thailand (5%) [7]. Snoring prevalence also differs among ethnicities. The higher snoring prevalence in Chinese descents compared with Caucasians might be due to Chinese people having narrower cranial bases and flatter mid-face structures [8].
OSA is closely associated with several serious illnesses, including systemic hypertension, coronary artery disease, stroke, and metabolic syndrome; it may also result in motor vehicle accidents and diminished quality of life [9,10,11]. OSA is insidious, and patients are often unaware of the associated symptoms. The cardinal manifestations of OSA include loud snoring, breathing pauses during sleep, fitful sleep quality, and excessive daytime sleepiness [12]. Although not all patients with snoring have clinically significant sleep apnea, snoring is the earliest and most common symptom of OSA, occurring in 70–95% of patients with OSA [13, 14]. In addition, snoring intensity increases with OSA severity [14], and snoring itself can present a vascular risk [15].
One related study distinguished between two types of snore: the first type has a very low frequency (<20 Hz) but large-amplitude vibrations lasting from 0 to 1 s and 2.5 to 4.5 s; and the second type involves high-frequency sounds with small-amplitude vibrations lasting from 1.0 to 1.5 s and 4.5 to 5.0 s [15]. Another study reported that snores can be categorized into irregular and regular snores and noted that patients with severe OSA had a shorter interval between regular snores [16]. Various obstruction sites also induce different snoring frequencies. Common obstruction sites include the velum, oropharynx, tongue base, and epiglottis [17]. The frequencies of more severe snoring differ considerably from those of habitual snoring, which range from 110 to 190 Hz [18, 19]. However, in patients with OSA, the snoring frequency might be higher than 800Hz [20, 21]. Notably, the average snoring sound intensity is higher for men than for women [19]. Polysomnography (PSG) is the gold standard method for diagnosing OSA and monitoring snoring [13]. However, PSG must be performed at special sleep treatment centers where patients sleep overnight. Patients undergoing PSG may experience some inconveniences. First, many patients do not sleep well during PSG examination because of the discomfort resulting from the cumbersome monitoring wires required for this test. Second, patients might face wait times of several weeks or even longer for a PSG examination in Taiwan. Third, the PSG test is a time-consuming procedure that can result in considerable patient discomfort [22]. Therefore, simplified recording and monitoring instruments that can conveniently and reliably diagnose snoring and OSA at home are necessary [23]. A related study suggested that sleep physicians consider repeat testing with home sleep apnea tests (HSATs) in patients with a negative PSG and clinical symptoms of OSA [24]. HSAT devices are classified by the United States Food and Drug Administration (FDA) as Class II medical devices, which the FDA defines as “devices for which general controls are insufficient to provide reasonable assurance of the safety and effectiveness of the device” [25]. However, HSATs have some limitations. For example, mispositioned pulse oximeters can yield false low readings [26]. HSAT devices that include cardiorespiratory portable monitors have sensors that can detect breathing patterns and pulse oxygen saturation, masks with tubes for insertion into patients’ nostrils, and sensors for patients’ abdomen and chest. These devices may interrupt sleep and be inconvenient for most patients, who may be unable to afford the cost of using HSAT devices at home every night. Finally, raw data from HSAT devices cannot be read directly and must be reviewed and interpreted by a certified physician.
Along with advances in science and technology, the functions of smartphones have expanded dramatically and rapidly. In addition to their communication features, smartphones allow users to download apps through online stores. More than 100,000 health apps are available on the Android and iOS platforms, with one target for health and fitness apps being sleep and sleep hygiene [27]. Snoring apps are software applications that run on smartphones and record sound information while the user sleeps; such apps have been available for several years and enable convenient and personalized sleep care [28]. Snoring apps are undoubtedly a simple and feasible option for monitoring snoring. With the progress of innovative monitoring mechanisms and techniques, these apps can be used regularly at home for examinations without interrupting a person’s sleep. The precision of smartphone apps for predicting snoring reportedly ranges from 93 to 96%, with a sensitivity ranging from 64 to 96%; however, app performance can vary greatly among smartphone models [29]. This study explored snoring detection accuracy in one of these smartphone apps, Snore Clock.
Materials and methods
Patients and methods
Patients with snoring problems using the Lin oral appliance (I602555 [Taiwan], ZL 2013 1 0753192.9 [China]) [30] were recruited from a dental clinic. The inclusion criteria were patients with snoring problems who volunteered to participate in this study. The patients independently downloaded the paid app SnoreClock. Patients aged <20 years were excluded from the study. All patients placed their smartphones within arm’s reach just before falling asleep. Smartphones were positioned on the upper side of the shoulder within 30 cm of the head for optimal recording of snoring sounds. However, no special restrictions with respect to placing the phone on the bed or on a bedside table were applied. The patients recorded their snoring using SnoreClock, following their natural sleep habits for 2–3 weeks, after which the smartphones were returned to the researchers.
Snore Clock
Snore Clock provides the following data on the duration and intensity of snoring: sleep duration, snoring duration, snoring loudness (dB), maximum snoring loudness (dB), and rate of snoring duration (%). Snore Clock also has a feature that enables users to focus on particular snoring events to facilitate playback of the most notable snoring sounds. This app is available for both iOS and Android devices. The author of Snore Clock was not involved in this study.
All the recordings from Snore Clock were replayed and verified. Snoring was defined as snorting or grunting sounds while asleep. If Snore Clock displayed signals with no spiking waves, snoring was likely to be absent. However, segments of spiking waves indicated a higher possibility of snoring. The app marked snoring periods (including snoring signals and pauses) with red bands and calculated the rate of total snoring duration for all recording sessions.
Before we determined the presence of snoring signals, we conducted a test: the snoring of a randomly selected case (28-year-old man; body mass index = 23.3) was recorded simultaneously with a digital sound recorder using linear pulse-code modulation (ICD SX-2000, Sony Electronics Inc., Tokyo, Japan) and Snore Clock during sleep. The sound recorder had two built-in high-performance dynamic microphones. We set the low-cut filter switch to “OFF” in order to obtain snoring and breathing sounds, and we set the sampling rate to 44,100 Hz. We analyzed the dominant frequencies every 0.01 s. We carefully listened to this recording on the computer and compared the results between the digital recorder and SnoreClock. We noted that interrupted sounds with a large volume (higher dB in the app) were easily recognized as snoring by the app. These noisy sounds included signals with low frequencies (<1000 Hz) or high frequencies (wide frequency bands, as high as 15,762 Hz). However, sounds with smaller volumes with frequency spectrograms resembling snoring sounds on the computer were generally neglected by this app. These sounds were similar to stronger expiration air flows on the smartphone (frequencies < 5000Hz). All these processes required >10 h to complete.
We then carefully listened to the recordings; any equivocal sounds were confirmed by an ear, nose, and throat (ENT) specialist (Ching-Shiung Ting, M.D.): this is referred to as the “manual method” hereafter. The snoring epoch is composed of several snoring signals interrupted by pauses (<10 s) [31]. Therefore, the duration of snoring was represented by the sum of total snoring epochs.
The study protocol was reviewed and approved by the Research Ethics Committee of the Buddhist Dalin Tzu Chi Hospital in Taiwan (No. B10703013).
Statistical analysis
Statistical software R (version 3.6.1) was used for all statistical analyses. Statistical significance was set at p < 0.05, and all tests were two-tailed. Categorical variables are presented as frequency and percentage, and continuous variables are presented as mean ± standard deviation. Univariate linear regression analyses and correlations were performed to evaluate the factors associated with snoring rates. The sensitivity, specificity, positive predictive value, and negative predictive value of the app were calculated. Analysis of variance (ANOVA) was performed to test the mean differences between groups.
Results
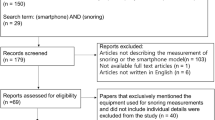
In total, 220 recordings from 11 patients were collected. We excluded recordings of <5 h (19 recordings) and finally included 201 recordings for further analysis. Three Asus ZenFone Max Plus (M1), three Apple iPhone 6, three Sony Xperia, one HTC One, and one Xiaomi Redmi 5 were used for the recordings. Short recordings (<5 h) were excluded because they might be reflective of patients with poor sleep or insufficient phone battery power. The patients’ basic demographic data are presented in Table 1. No patient had a history of diabetes, respiratory disease, sleep disorders, or alcohol or smoking problems.
The mean accuracy rate for snoring detection by SnoreClock was 95% (comprising 9% snoring rate and 86% non-snoring rate, approved both by the app and manual method). The mean snoring rates calculated by SnoreClock were only 0.3% less than those calculated using the manual method (11.3% ± 10.8% vs. 11.6% ± 12.9%; Table 2). The snoring rates measured by SnoreClock were highly correlated with the snoring rates measured using the manual method (r = 0.907, β = 1.09, p < 0.001; Fig. 1). Moreover, the false-negative rates for SnoreClock positively correlated with the false-negative rates for the manual method (r = 0.431, β = 1.06, p < 0.001; Table 3 and Fig. 2). The snoring rates determined using SnoreClock were then compared with those obtained using the manual method. The mean values of SnoreClock’s sensitivity, specificity, negative predictive value, and positive predictive value were 78% ± 25%, 97% ± 4%, 97% ± 4%, and 65% ± 35%, respectively (Table 4). Sensitivity versus 1−specificity was plotted with a smoothing line (Fig. 3). Different points according to different sensitivities and specificities had distinct positive and negative predictive values. We carefully calculated the area under the receiver operating characteristic curve (AUC) for every recording (201 AUCs for 201 recordings). The mean value of the AUC was 0.946 ± 0.528. Thus, Snore Clock had a high predictive value for snoring.
These recordings were time-series data. Each night’s sleep data were represented on 941 ± 199 px (range 540–1125 px) on the smartphone screens. Therefore, 1 px represented 28.0 ± 7.8 s. The app displayed the time bands of snoring on the screen. Manual snoring bands could also be drawn. We compared these snoring bands for every record. The chance of making a type II error (i.e., false-negative rate) is known as beta (β). We examined the false-negative rate for every recording. The power, represented by 1 − β, was acquired for every recording, and the mean power in our study was 97% ± 4%. The mean differences in snoring rates between the measurements by SnoreClock and estimation from the manual method for different phone brands were within ±5%. The p value of ANOVA for these mean differences between the iOS group and non-iOS group was 0.802.
Discussion
In the current study, we used the variable snoring rate (i.e., snoring duration or sleep duration) to determine Snore Clock’s accuracy. A strong correlation was observed between the results obtained through a manual measurement of snoring and Snore Clock, which were reviewed by an ENT specialist. The correlation between SnoreClock and the manual method for detecting snoring was 0.907 (p < 0.001).
The results indicated that SnoreClock is a highly accurate app for detecting snoring. The findings also revealed that the snoring rate was significantly underestimated if SnoreClock indicated a higher snoring rate.
The positive predictive value for snoring was 65% ± 35% in the current study; elsewhere, the results have been 70% [22] and 93–96% [29]. In Shin’s study [22], researchers detected snoring using a smartphone app at users’ homes. Non-snore noises are more common at home, which affected both the present and Shin’s study; such noises were less of a concern in Camacho’s study [29], which was conducted in a hospital. Non-snore noises in patients’ sleep areas, such as bedding noise, coughing, and environmental noise [32], might be the causes of false-positive snoring recorded in this study. In addition, in their study, Camacho used the app Quit Snoring and compared the results with in-laboratory PSG data. However, they used data from only two patients undergoing in-laboratory PSG and one case study and set 53 dB as the snoring threshold in Quit Snoring. In the current study, we used snoring rate during sleep time as a variable for analysis because the snoring event is actually a period.
Another novel finding of the current study is that snoring rate might be underestimated if the snoring rate percentage is higher in SnoreClock. A similar result was also obtained in the study of Kreivi, where researchers recorded snoring with an MP3 recorder [33]. One reason for this might be that the sensitivity was set to a higher level to increase snoring detection [27]. Another reason might be the different frequencies of snoring to which the app was set.
Limitations
This study has limitations. First, snoring apps might be unable to distinguish between the snores of different people in a room. Second, the accuracy of Snore Clock was validated by an ENT specialist, not through PSG testing, despite PSG being the gold standard method to diagnose snoring. Third, the app might be unable to determine snoring when the sounds have low volumes or their frequencies are similar to those of the background. Fourth, the recording time represented sleep duration. The definite timing of falling sleep and waking up could not be detected by Snore Clock. Fifth, we experienced difficulty in investigating the hardware with regard to the bandwidth, amplification, and filter settings. These settings may have influenced the snoring detection output. Finally, all the patients in the present study were middle aged (30–52 years), implying that the results cannot be extrapolated to other age groups.
Conclusion
The mean accuracy rate for snoring detection by SnoreClock was 95%. The correlation between SnoreClock and the manual method for detecting snoring was strong. SnoreClock can be used on various smartphone brands and has a high predictive value for snoring. Our results validate at-home snoring detection through SnoreClock.
Abbreviations
- App:
-
application;
- AUC:
-
area under the curve (receiver operating characteristic curve);
- BMI:
-
body mass index;
- dB:
-
decibel;
- ENT:
-
ear, nose, and throat;
- HSATs:
-
home sleep apnea tests;
- Hz:
-
hertz;
- OSA:
-
obstructive sleep apnea;
- PSG:
-
polysomnography
References
Nakano H, Hirayama K, Sadamitsu Y, Toshimitsu A, Fujita H, Shin S, Tanigawa T (2014) Monitoring sound to quantify snoring and sleep apnea severity using a smartphone: proof of concept. J Clin Sleep Med 10(1):73–78
Chuang LP, Hsu SC, Lin SW, Ko WS, Chen NH, Tsai YH (2008) Prevalence of snoring and witnessed apnea in Taiwanese adults. Chang Gung Med J 31(2):175–181
Kamil MA, Teng CL, Hassan SA (2007) Snoring and breathing pauses during sleep in the Malaysian population. Respirology 12(3):375–380
Kart L, Dutkun Y, Altin R, Ornek T, Kıran S (2010) Prevalence of major obstructive sleep apnea syndrome symptoms in coal miners and healthy adults. Tuberk Toraks 58(3):261–267
Nagayoshi M, Yamagishi K, Tanigawa T et al (2011) Risk factors for snoring among Japanese men and women: a community-based cross-sectional study. Sleep Breath 15(1):63–69
Khoo SM, Tan WC, Ng TP, Ho CH (2004) Risk factors associated with habitual snoring and sleep-disordered breathing in a multi-ethnic Asian population: a population-based study. Respir Med 98(6):557–566
Suwanprathes P, Won C, Komoltri C, Nana A, Kotchabhakdi N, Guilleminault C (2010) Epidemiology of sleep-related complaints associated with sleep-disordered breathing in Bangkok, Thailand. Sleep Med 11(10):1025–1030
Lam B, Ip MS, Tench E, Ryan CF (2005) Craniofacial profile in Asian and white subjects with obstructive sleep apnoea. Thorax 60(6):504–510
Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V (2005) Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med 353(19):2034–2041
Nieto FJ, Young TB, Lind BK, Shahar E, Samet JM, Redline S, D'Agostino RB, Newman AB, Lebowitz MD, Pickering TG (2000) Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health Study. JAMA 283(14):1829–1836
Young T, Peppard PE, Gottlieb DJ (2002) Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med 165(9):1217–1239
Punjabi NM (2008) The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc 5(2):136–143
Abeyratne UR, Wakwella AS, Hukins C (2005) Pitch jump probability measures for the analysis of snoring sounds in apnea. Physiol Meas 26(5):779–798
Maimon N, Hanly PJ (2010) Does snoring intensity correlate with the severity of obstructive sleep apnea? J Clin Sleep Med 6(5):475–478
Lee GS, Lee LA, Wang CY, Chen NH, Fang TJ, Huang CG, Cheng WN, Li HY (2016) The Frequency and Energy of Snoring Sounds Are Associated with Common Carotid Artery Intima-Media Thickness in Obstructive Sleep Apnea Patients. Sci Rep 6:30559
Mesquita J, Sola-Soler J, Fiz JA, Morera J, Jané R (2012) All night analysis of time interval between snores in subjects with sleep apnea hypopnea syndrome. Med Biol Eng Comput 50(4):373–381
Lee LA, Lo YL, Yu JF, Lee GS, Ni YL, Chen NH, Fang TJ, Huang CG, Cheng WN, Li HY (2016) Snoring Sounds Predict Obstruction Sites and Surgical Response in Patients with Obstructive Sleep Apnea Hypopnea Syndrome. Sci Rep 6:30629
Cavusoglu M, Kamasak M, Erogul O, Ciloglu T, Serinagaoglu Y, Akcam T (2007) An efficient method for snore/nonsnore classification of sleep sounds. Physiol Meas 28(8):841–853
Pevernagie D, Aarts RM, De Meyer M (2010) The acoustics of snoring. Sleep Med Rev 14(2):131–144
Perez-Padilla JR, Slawinski E, Difrancesco LM, Feige RR, Remmers JE, Whitelaw WA (1993) Characteristics of the snoring noise in patients with and without occlusive sleep apnea. Am Rev Respir Dis 147(3):635–644
Fiz JA, Abad J, Jane R et al (1996) Acoustic analysis of snoring sound in patients with simple snoring and obstructive sleep apnoea. Eur Respir J 9(11):2365–2370
Shin H, Cho J (2014) Unconstrained snoring detection using a smartphone during ordinary sleep. Biomed Eng Online 13:116
Dalmasso F, Benedetto G, Pogolotti R, Righini G, Spagnolo R (1990) Digital processing of snoring sounds. Eur Respir J Suppl 11:528s–532s
Lipatov K, Hayek A, Ghamande S, Boethel C, Chen W, Jones S (2018) Predictors of Obstructive Sleep Apnea on a Home Sleep Apnea Test After a Negative Attended Polysomnography. J Clin Sleep Med 14(11):1889–1894
U.S. FOOD & DRUG ADMINISTRATION. 2020 https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpcd/classification.cfm. Accessed 19 Dec 2020
Kapoor M (2019) Positive Home Sleep Apnea Test After a Negative Polysomnogram: Role of Potential Confounding Factors. J Clin Sleep Med 15(3):519–520
Ong AA, Gillespie MB (2016) Overview of smartphone applications for sleep analysis. World J Otorhinolaryngol Head Neck Surg 2(1):45–49
Shin H, Choi B, Kim D, Cho J (2014) Robust sleep quality quantification method for a personal handheld device. Telemed J E Health 20(6):522–530
Camacho M, Robertson M, Abdullatif J, Certal V, Kram YA, Ruoff CM, Brietzke SE, Capasso R (2015) Smartphone apps for snoring. J Laryngol Otol 129(10):974–979
Nature Dental Clinic. 2019 http://www.alliswell.tw/braces/ Accessed September 7, 2019
Lee SA, Amis TC, Byth K, Larcos G, Kairaitis K, Robinson TD, Wheatley JR (2008) Heavy snoring as a cause of carotid artery atherosclerosis. Sleep 31(9):1207–1213
Dafna E, Tarasiuk A, Zigel Y (2013) Automatic detection of whole night snoring events using non-contact microphone. PLoS One 8(12):e84139
Kreivi HR, Salmi T, Maasilta P, Bachour A (2013) Screening of snoring with an MP3 recorder. Sleep Breath 17(1):77–84
Funding
JK Chiang received grants from the Dalin Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation (DTCRD108(2)-E-09). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The author of the SnoreClock app did not have involvement of this study.
Author information
Authors and Affiliations
Contributions
YHK, CWL, and JKC contributed to conception, design, and drafting of the manuscript. JKC analyzed and interpreted the data. YCL, YCY, CST, and YYC wrote the manuscript. All authors revised and approved the final version. YH Kao and CW Lin contributed equally.
Corresponding author
Ethics declarations
Ethical approval
The study protocol was reviewed and approved by the Research Ethics Committee of the Buddhist Dalin Tzu Chi Hospital in Taiwan (No. B10703013).
Informed consent
Informed consent was obtained from all individual participants included in this study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chiang, JK., Lin, YC., Lin, CW. et al. Validation of snoring detection using a smartphone app. Sleep Breath 26, 81–87 (2022). https://doi.org/10.1007/s11325-021-02359-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02359-3