Abstract
Purpose
Obstructive sleep apnea (OSA) may contribute to metabolic and inflammatory deregulation but previous studies failed to consider sleep duration, sleep fragmentation, insomnia, and daytime sleepiness as potential confounders.
Methods
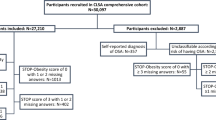
Consecutive non-diabetic middle-aged participants from the ELSA-Brasil cohort were invited to perform a clinical evaluation, home sleep study for 1 night, and wrist actigraphy for 7 days. OSA was defined by an apnea-hypopnea index ≥ 15 events/h. Participants were stratified according to the presence of OSA measuring the following markers: fasting glucose, glucose tolerance test, homeostatic model assessment of insulin resistance (HOMA-IR) index, fasting insulin, insulin after 2 h of glucose load, glycated hemoglobin, total cholesterol and their fractions, triglycerides, C-reactive protein, TNF-alpha, interleukin-6, interleukin-10, leptin, adiponectin, E-selectin, ADMA, MCP-1, TGF, apolipoprotein B, fibrinogen, and lipoprotein(a). Differences between groups were identified by chi-square test and ANOVA.
Results
We studied 708 participants (mean age: 46 ± 5 years, men: 44%, BMI 26.1 ± 4.1 kg/m2). Compared to no OSA, participants with OSA presented higher levels while fasting and after 2 h glucose load of insulin, HOMA-IR, cholesterol, triglycerides, and C-reactive protein (all p < 0.001). After linear regression analysis adjusting for traditional risk factors plus sleep duration, fragmentation, insomnia, and daytime sleepiness, OSA was negatively associated with adiponectin (β = − 0.271 CI 95% − 0.456 − 0.085) and positively associated with cholesterol (β = 9.707 CI 95% 2.737 16.678). Sex-stratification revealed that these associations were significant for men but not women.
Conclusions
In non-diabetic middle-age adults, men with OSA presented with lower adiponectin and higher cholesterol levels independently of sleep duration, sleep fragmentation, insomnia, and daytime sleepiness.

Similar content being viewed by others
References
Drager LF, McEvoy RD, Barbe F, Lorenzi-Filho G, Redline S (2017) Sleep apnea and cardiovascular disease: lessons from recent trials and need for team science. Circulation 136(19):1840–1850
Marin JM, Carrizo SJ, Vicente E, Augusti AGN (2005) Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. The Lancet 365(9464):1046–1053
Drager LF, Togeiro SM, Polotsky VY, Lorenzi-Filho G (2013) Obstructive sleep apnea: a cardiometabolic risk in obesity and the metabolic syndrome. J Am Coll Cardiol. 62(7):569–576
Guilleminault C, Ceyda K, Maurice MO (2004) C-reactive protein and sleep-disordered breathing. Sleep 27(8):1507–1517
Taheri S, Austin D, Lin L, Nieto J, Young T, Mignot E (2007) Correlates of serum C-reactive protein (CRP)—no association with sleep duration or sleep disordered breathing. Sleep 30(8):991–996
Sharma SK, Mishra HK, Sharma H, Goel A, Sreenivas V, Gulati V, Mohammad T (2008) Obesity, and not obstructive sleep apnea, is responsible for increased serum hs-CRP levels in patients with sleep-disordered breathing in Delhi. Sleep Med 9(2):149–156
Vgontzas AN, Liao D, Pejovic S, Calhoun S, Karataraki M, Bixler EO (2009) Insomnia with objective short sleep duration is associated with type 2 diabetes: a population-based study. Diabetes Care 32(11):1980–1985
Ramos AR, Weng J, Wallace DM, Petrov MR, Wohlgemuth WK, Sotres-Alverez D et al (2018) Sleep patterns and hypertension using actigraphy in the Hispanic Community Health Study/Study of Latinos. Chest 153(1):87–93
Scharf SM, Tubman A, Smale P (2005) Prevalence of concomitant sleep disorders in patients with obstructive sleep apnea. Sleep Breath 9(2):50–56
Patel SR, Hu FB (2008) Short sleep duration and weight gain: a systematic review. Obesity 16(3):643–653
Cappuccio FP, Taggarat FM, Kandala N, Currie A, Peile E, Stranges S et al (2008) Meta-analysis of short sleep duration and obesity in children and adults. Sleep 31(5):619–626
Gangwisch JE, Heymsfield SB, Boden-Albala B, Bujis RM, Kreier F, Pickering TG et al (2007) Sleep duration as a risk factor for diabetes incidence in a large US sample. Sleep 30(12):1667–1673
Mullington JM, Simpson NS, Meier-Ewert HK, Haak M (2010) Sleep loss and inflammation. Best Pract Res Clin Endocrinol Metab 24(5):775–784
Luyster FS, Buysse DJ, Strollo PJ (2010) Comorbid insomnia and obstructive sleep apnea: challenges for clinical practice and research. J Clin Sleep Med 6(2):196–204
Aquino EML, Barreto SM, Bensenor IM, Carvalho MS, Chor D, Duncan BB et al (2012) Brazilian longitudinal study of adult health (ELSA-Brasil): objectives and design. Am J Epidemiol 175(4):315–324
Drager LF, Santos RB, Silva WA, Parise BK, Giatti S, Aielo AN et al (2019) OSA, short sleep duration, and their interactions with sleepiness and cardiometabolic risk factors in adults: the ELSA-Brasil Study. Chest 155(6):1190–1198
Schmidt MI, Duncan BB, Mill JG, Lotufo PA, Chor D, Barreto SM et al (2014) Cohort profile: longitudinal study of adult health (ELSA-Brasil). Int J Epidemiol 44(1):68–75
Bensenor IM, Griep RH, Pinto KA, Faria CP, Felisbino-Mendes M, Caetano EI et al (2013) Routines of organization of clinical tests and interviews in the ELSA-Brasil investigation center. Rev Saude Publ 47(suppl 2):37–47
Treff C, Benseñor IM, Lotufo PA (2017) Leisure-time and commuting physical activity and high blood pressure: the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). J Human Hypertens 31(4):278–283
American Diabetes Association (2010) Diagnosis and classification of diabetes mellitus. Diab Care. 33(Suppl.1):S62–S69
Mill JG, Pinto K, Griep RH, Goulart A, Foppa M, Lotufo PA et al (2013) Medical assessments and measurements in ELSA-Brasil. Rev Saude Publ 47(suppl2):54–62
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14(6):540–545
Bertolazi AN, Fagondes SC, Hoff LS, Pedro VD, Barreto SSM, Johns MW (2009) Portuguese-language version of the Epworth sleepiness scale: validation for use in Brazil. J Bras Pneumol 35(9):877–883
Nunes MA, Alves MGM, Chor D, Schmidt MI, Duncan BB (2011) Cross-cultural adaptation of CIS-R (clinical interview schedule-revised version) for portuguese in longitudinal study of adult health (ELSA). Rev HCPA 31:487–490
Stewart R, Besset A, Bebbington P, Brugha T, Lindesay J, Jenkins R et al (2006) Insomnia comorbidity and impact and hypnotic use by age group in a national survey population aged 16 to 74 years. Sleep 29:1391–1397
Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L (2015) National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health 1(1):40–43
Chen X, Wang R, Zee P, Lutsey PL, Javaheri S, Alcántara C et al (2015) Racial/ethnic differences in sleep disturbances: the Multi-Ethnic Study of Atherosclerosis (MESA). Sleep 38(6):877–888
Ogilvie RP, Redline S, Bertoni AG, Chen X, Ouyang P, Szklo M, Lutsey PL (2016) Actigraphy measured sleep indices and adiposity: the Multi-Ethnic Study of Atherosclerosis (MESA). Sleep 39(9):1701–1708
Ng SSS, Chan T, To K, Ngai J, Tung A, Ko FWS (2010) Validation of Embletta portable diagnostic system for identifying patients with suspected obstructive sleep apnoea syndrome (OSAS). Respirology 15(2):336–342
Verse T, Prisig W, Junge-Hulsing B, Junge-Hulsing B, Kroker B (2000) Validation of the POLY-MESAM seven-channel ambulatory recording unit. Chest 117(6):1613–1618
Calleja JM, Esnaola S, Rubio R, Durán J (2002) Comparison of a cardiorespiratory device versus polysomnography for diagnosis of sleep apnoea. Eur Respir J. 20:1505–1510
Oliveira ACT, Martinez D, Vasconcelos LFT, Gonçalves SC, Lenz MC, Fuchs FC Diagnosis of obstructive sleep apnea syndrome and its outcomes with home portable monitoring. Chest 135(2):330–336
Aielo AN, Santos RB, Silva WA, Giatti S, Parise BK et al (2019) Pragmatic validation of home portable sleep monitor for diagnosing obstructive sleep apnea in a non-referred population: the ELSA-Brasil. Sleep Sci 12(2):65–71
Berry RB, Budhijara R, Gottilied D, Gozal D, Iber C, Kapur V et al (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events. J Clin Sleep Med 8(5):597–619
Chowdhuri S, Quan SF, Almeida F, Ayappa I, Batool-Anwar S, Budhiraja R et al (2016) An official American Thoracic Society research statement: impact of mild obstructive sleep apnea in adults. Am J Respir Crit Care Med 193(9):e37–e54
Almeida-Pititto B, Ribeiro-Filho FF, Santos IS, Lotufo PA, Bensenor IM, Ferreira SRG (2017) Association between carotid intima-media thickness and adiponectin in participants without diabetes or cardiovascular disease of the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). Eur J Prev Cardiol 24(2):116–122
Reichmuth KJ, Austin D, Skatrud JB, Young T (2005) Association of sleep apnea and type II diabetes: a population-based study. Am J Respir and Crit Care Med 172(12):1590–1595
Nadeem R, Singh M, Nida M, Waheed I, Khan A, Ahmed S et al (2014) Effect of obstructive sleep apnea hypopnea syndrome on lipid profile: a meta-regression analysis. J Clin Sleep Med 10(5):475–489
Punjabi NM, Sorkin JD, Katzel LI, Goldberg AP, Schwartz AR, Smith PL (2002) Sleep-disordered breathing and insulin resistance in middle-aged and overweight men. Am J Respir Crit Care Med 165(5):677–682
Drager LF, Yao Q, Hernandez KL, Shin MK, Bevans-Fonti S, Gay J et al (2013) Chronic intermittent hypoxia induces atherosclerosis via activation of adipose angiopoietin-like 4. Am J Respir Crit Care Med. 188(2):240–248
Drager LF, Tavoni TM, Silva VM, Santos RD, Pedrosa RP, Bortolotto LA et al (2018) Obstructive sleep apnea and effects of continuous positive airway pressure on triglyceride-rich lipoprotein metabolism. J Lipid Res. 59(6):1027–1033
Toyama Y, Chin K, Chihara Y, Takegami M, Takahashi K, Sumi K et al (2013) Association between sleep apnea, sleep duration, and serum lipid profile in an urban, male, working population in Japan. Chest 143(3):720–728
Seelig E, Keller U, Klarhofer M, Scheffler K, Brand S, Holsboer-Trachsle E et al (2013) Neuroendocrine regulation and metabolism of glucose and lipids in primary chronic insomnia: a prospective case-control study. Plos One 8(4):e61780
Mallon L, Broman J, Hetta J (2005) High incidence of diabetes in men with sleep complaints or short sleep duration: a 12-year follow-up study of a middle-aged population. Diabetes Care 28(11):2762–2767
Risso TT, Poyares D, Rizzi CF, Pulz C, Guilleminault C, Tufik S et al (2013) The impact of sleep duration in obstructive sleep apnea patients. Sleep Breath. 17(2):837–843
Kritikou I, Basta M, Vgontzas AN, Pejovik S, Liao D, Tsaoussoglou M et al (2014) Sleep apnoea, sleepiness, inflammation and insulin resistance in middle-aged males and females. Eur Respir J. 43(1):145–155
Sharma SK, Kumpawat S, Goel A, Banga A, Ramakrishnan L, Chaturdevi P (2007) Obesity, and not obstructive sleep apnea, is responsible for metabolic abnormalities in a cohort with sleep-disordered breathing. Sleep Med 8(1):12–17
Lu M, Fang F, Wang Z, Wei P, Hu C, Wei Y (2019) Association between serum/plasma levels of adiponectin and obstructive sleep apnea hypopnea syndrome: a meta-analysis. Lipids Health Dis 18(1):30
Zhang XL, Yin KL, Wang H, Su S (2006) Serum adiponectin levels in adult male patients with obstructive sleep apnea hypopnea syndrome. Respiration 73(1):73–77
Ng SSS, Liu EKH, Ma RCW, Chan T, Wang K, To KW et al (2017) Effects of CPAP therapy on visceral fat thickness, carotid intima-media thickness and adipokines in patients with obstructive sleep apnoea. Respirology 22(4):786–792
Nakagawa Y, Kishida K, Kihara S, Sonoda M, Hirata A, Nishizawa H et al (2008) Nocturnal reduction in circulating adiponectin concentrations related to hypoxic stress in severe obstructive sleep apnea-hypopnea syndrome. Am J Physiol-Endocrinol Metab 294(4):E778–E784
Vatansever E, Surmen-Gur E, Ursavas A, Karadag M (2011) Obstructive sleep apnea causes oxidative damage to plasma lipids and proteins and decreases adiponectin levels. Sleep Breath 15(3):275–282
Lam JCM, Xu A, Tam S, Khong P, Yao P, Lam DCL et al (2008) Hypoadiponectinemia is related to sympathetic activation and severity of obstructive sleep apnea. Sleep 31(12):1721–1727
Magalang UJ, Cruff JP, Rajappan R, Hunter MG, Patel T, Marsh CB et al (2009) Intermittent hypoxia suppresses adiponectin secretion by adipocytes. Exp Clin Endocrinol Diabetes. 117(3):129–134
Hafiane A, Gasbarrino K (2019) DaskalopoulouSS. Adiponectin and cholesterol efflux. Metabolism 153953
Tan KC, Chow WS, Lam JC, Lam B, Wong WK, Tam S et al (2006) HDL dysfunction in obstructive sleep apnea. Atherosclerosis. 184:377–382
McArdle N, Hillman D, Beilin L, Watts G (2007) Metabolic risk factors for vascular disease in obstructive sleep apnea: a matched controlled study. Am J Respir Crit Care Med 175(2):190–195
Li J, Thorne LN, Punjabi NM, Sun C, Schwartz AR, Smith PL et al (2005) Intermitent hypoxia induces hyperlipidemia in lean mice. Circ Res 97(7):698–706
Pilkauskaite G, Miliauskas S, Vitkauskiene A, Sakalauskas R (2014) Vascular adhesion molecules in men with obstructive sleep apnea: associations with obesity and metabolic syndrome. Sleep Breath. 18(4):869–874
Peres BU, Allen AJH, Kendzerska T, Shah A, Fox N, Laher I, Almeida F, Jen R, Sandford AJ, van Eeden SF, Ayas NT. Obstructive sleep apnea severity, body mass index, and circulating levels of cellular adhesion molecules. Lung 2020. https://doi.org/10.1007/s00408-020-00401-x. Online ahead of print.
Funding
This work was supported by a research grant from FAPESP [Grant 2012/02953-2]. The Brazilian Longitudinal Study of Adult Health (ELSA-Brasil) was supported by the Brazilian Ministry of Health (Science and Technology Department) and the Brazilian Ministry of Science and Technology (Financiadora de Estudos e Projetos and CNPq National Research Council) [Grants01 06 0010.00 RS, 01 06 0212.00 BA, 01 06 0300.00 ES, 01 060278.00 MG, 01 06 0115.00 SP, 01.10.0773.00 SP, and 01 060071.00 RJ]
Author information
Authors and Affiliations
Contributions
Conceptualization: Wagner A. Silva, Bianca Almeida-Pititto, Luciano F. Drager
Methodology: Wagner A. Silva, Bianca Almeida-Pititto, Ronaldo B. Santos, Luciano F. Drager
Formal analysis and investigation: Wagner A. Silva, Bianca Almeida-Pititto. Ronaldo B. Santos, Aline N. Aielo, Soraya Giatti, Barbara K. Parise, Silvana P. Souza
Writing—original draft preparation: Wagner A. Silva, Bianca Almeida-Pititto, Luciano F. Drager
Writing—review and editing: All authors
Funding acquisition: Sandra F. Vivolo, Paulo A. Lotufo, Isabela M. Bensenor, and Luciano F. Drager
Corresponding author
Ethics declarations
Ethical approval
This study has been approved by the local Ethics Committee, under number 1478/15, in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOC 49 kb)
Rights and permissions
About this article
Cite this article
Silva, W.A., Almeida-Pititto, B., Santos, R.B. et al. Obstructive sleep apnea is associated with lower adiponectin and higher cholesterol levels independently of traditional factors and other sleep disorders in middle-aged adults: the ELSA-Brasil cohort. Sleep Breath 25, 1935–1944 (2021). https://doi.org/10.1007/s11325-021-02290-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02290-7