Abstract
Objective
Insomnia is a common sleep disorder that affects many adults either transiently or chronically. This study aimed to establish whether there is a relationship between the electroencephalographic (EEG) spectral analysis and salivary cortisol levels in insomnia and compared to healthy controls.
Materials and methods
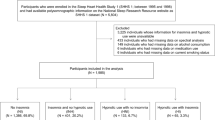
This case–control study included 15 insomnia patients and 15 healthy control subjects. Insomnia was determined according to the International Classification of Headache Disorders III diagnostic criteria. The EEG data were collected and processed with MATLAB software. Blood and salivary samples were taken for hematological and biochemical measurements. Salivary cortisol levels were calculated and compared statistically with the healthy group.
Results
The mean age of the patients was 46.5 ± 11 years. The salivary cortisol levels at 18:00 and 24:00 were found higher in the insomnia than in the healthy subjects (respectively, 0.12 (0.11) μg/dl, 0.07 (0.02) μg/dl). But this difference was not statistically significant (p > 0.05). No significant difference was observed in the spectral analysis of patients between the frontal, central, and occipital channel (p > 0.05). However, in the correlation between the frontal channel spectral analysis and at the 24:00 salivary cortisol of patient and control group, DeltaGmax (p = 0.002), DeltaGmean (p = 0.019) and, in the correlation with 18:00 salivary cortisol DeltaGmax (p = 0.010), were positively correlated.
Conclusion
In this study, no significant difference was found in spectral analysis and salivary cortisol levels in insomnia patients, but at 18:00 and 24:00, cortisol levels were correlated positively with theta and delta waves in EEG spectral analysis in some channels.

Similar content being viewed by others
References
Medicine, A.A.o.S (2014) International classification of sleep disorders—third edition (ICSD-3). AASM Resource Library [online]
Association, A.P (2013) Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub
Ohayon MM, Reynolds CF (2009) Epidemiological and clinical relevance of insomnia diagnosis algorithms according to the DSM-IV and the International Classification of Sleep Disorders (ICSD). Sleep Med 10:952–960
Can J (2011) Prevalence of insomnia and its treatment in Canada. Can J Psychiatr 56:540–548
Morin CM, Benca R (2012) Chronic insomnia. Lancet 379:1129–1141
Morin CM, LeBlanc M, Daley M, Gregoire JP, Mérette C (2006) Epidemiology of insomnia: prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Med 7:123–130
Roehrs T, Roth T (2019) Hyperarousal in insomnia: pre-sleep and diurnal cortisol levels in response to chronic zolpidem treatment. Sleep Med 61:52–56
Riemann D, Spiegelhalder K, Feige B, Voderholzer U, Berger M, Perlis M, Nissen C (2010) The hyperarousal model of insomnia: a review of the concept and its evidence. Sleep Med Rev 14:19–31
Pigeon WR (2010) Diagnosis, prevalence, pathways, consequences & treatment of insomnia. Indian J Med Res 131:321–332
Bastien CH (2011) Insomnia: neurophysiological and neuropsychological approaches. Neuropsychol Rev 21:22–40
Roth T, Roehrs T, Pies R (2007) Insomnia: pathophysiology and implications for treatment. Sleep Med Rev 11:71–79
Bonnet MH, Arand DL (2010) Hyperarousal and insomnia: state of the science. Sleep Med Rev 14:9–15
Abell JG, Shipley MJ, Ferrie JE, Kivimäki M, Kumari M (2016) Recurrent short sleep, chronic insomnia symptoms and salivary cortisol: a 10-year follow-up in the Whitehall II study. Psychoneuroendocrinology. 68:91–99
Rodenbeck A, Hajak G (2001) Neuroendocrine dysregulation in primary insomnia. Rev Neurol 157:57–61
Rodenbeck A, Huether G, Rüther E, Hajak G (2002) Interactions between evening and nocturnal cortisol secretion and sleep parameters in patients with severe chronic primary insomnia. Neurosci Lett 324:159–163
Seelig E et al (2013) Neuroendocrine regulation and metabolism of glucose and lipids in primary chronic insomnia: a prospective case-control study. PLoS One 8:e61780
Kumari M, Badrick E, Ferrie J, Perski A, Marmot M, Chandola T (2009) Self-reported sleep duration and sleep disturbance are independently associated with cortisol secretion in the Whitehall II study. J Clin Endocrinol Metab 94:4801–4809
Vgontzas AN, Bixler EO, Lin HM, Prolo P, Mastorakos G, Vela-Bueno A, Kales A, Chrousos GP (2001) Chronic insomnia is associated with nyctohemeral activation of the hypothalamic-pituitary-adrenal axis: clinical implications. J Clin Endocrinol Metab 86:3787–3794
Krystal AD, Edinger JD, Wohlgemuth WK, Marsh GR (2002) NREM sleep EEG frequency spectral correlates of sleep complaints in primary insomnia subtypes. Sleep 25:630–640
Svetnik V, Snyder ES, Ma J et al (2017) EEG spectral analysis of NREM sleep in a large sample of patients with insomnia and good sleepers: effects of age, sex and part of the night. J Sleep Res 26:92–104
Wu YM, Regina Pietrone J, Cashmere D et al (2013) EEG power during waking and NREM sleep in primary insomnia. J Clin Sleep Med 9:1031–1037
Lattova Z, Keckeis M, Maurovich-Horvat E, Wetter TC, Wilde-Frenz J, Schuld A, Pollmächer T (2011) The stress hormone system in various sleep disorders. J Psychiatr Res 45:1223–1228
Varkevisser M, Van Dongen H, Kerkhof G (2005) Physiologic indexes in chronic insomnia during a constant routine: evidence for general hyperarousal. Sleep 28:1588–1596
Backhaus J, Junghanns K, Hohagen F (2004) Sleep disturbances are correlated with decreased morning awakening salivary cortisol. Psychoneuroendocrinology 29:1184–1191
Perlis ML, Kehr EL, Smith MT, Andrews PJ, Orff H, Giles DE (2001) Temporal and stagewise distribution of high frequency EEG activity in patients with primary and secondary insomnia and in good sleeper controls. J Sleep Res 10:93–104
Buysse DJ, Germain A, Hall ML, Moul DE, Nofzinger EA, Begley A, Ehlers CL, Thompson W, Kupfer DJ (2008) EEG spectral analysis in primary insomnia: NREM period effects and sex differences. Sleep 31:1673–1682
Riedner BA et al (2015) Regional patterns of elevated alpha and high-frequency electroencephalographic activity during nonrapid eye movement sleep in chronic insomnia: a pilot study. Sleep 39:801–812
Buckelew SP, DeGood D, Roberts KD, Butkovic JD, MacKewn A (2009) Awake EEG disregulation in good compared to poor sleepers. Appl Psychophysiol Biofeedback 34:99–103
Knyazev GG, Slobodskaya HR (2003) Personality trait of behavioral inhibition is associated with oscillatory systems reciprocal relationships. Int J Psychophysiol 48:247–261
Schutter DJ, Van Honk E (2005) Salivary cortisol levels and the coupling of midfrontal delta-beta oscillations. Int J Psychophysiol 55:127–129
Van Peer JM, Roelofs K, Spinhoven P (2008) Cortisol administration enhances the coupling of midfrontal delta and beta oscillations. Int J Psychophysiol 67:144–150
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Before the study, approval of local ethics committee was obtained from Faculty of Medicine Dean’s Office (ethics committee approval no: 2014/171), and the study was in compliance with Helsinki declaration. All of the patients included in the study were informed about the tests, testing methods, and side effects. All the patients gave written consent required to perform the tests.
Conflict of interest
The authors declare that they have no conflict of interest.
DisclaimerThe authors alone are responsible for the content and writing of the paper.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bolattürk, Ö.F., İsmailoğullari, S., Aldemir, R. et al. The correlation between the electroencephalographic spectral analysis and salivary cortisol rhythm in insomnia. Sleep Breath 24, 661–667 (2020). https://doi.org/10.1007/s11325-020-02032-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-020-02032-1