Abstract
Purpose
Physical activity has been associated with several individual dimensions of sleep. However, the association between physical activity and sleep health, a construct that emphasizes the multidimensional nature of sleep, has not been explored. This analysis examined the relationship between physical activity and a composite measure of sleep health.
Methods
A total of 114 adults (66% female, 60.3 ± 9.2 years) were included in the analyses. Participants reported daily light-intensity physical activity (LPA) and moderate- and vigorous-intensity physical activity (MVPA) via diary, while wearing a pedometer (Omron HJ-720ITC) to measure daily steps. Sleep health was measured using the RU_SATED questionnaire, which addresses regularity of sleep patterns, satisfaction with sleep, daytime alertness, and sleep timing, efficiency, and duration. Multiple linear regression, binary logistic regression, and analysis of covariance (ANCOVA) were utilized for analyses.
Results
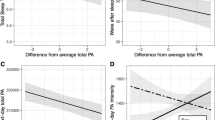
Mean sleep health score was 9.6 ± 2.4 (0 [poor]–12 [good]). Participants reported 62.9 ± 66.0 and 51.2 ± 51.2 min/day of LPA and MVPA, respectively, and took 5585.5 ± 2806.7 steps/day. Greater MVPA was associated with better sleep health (β = 0.27, P = 0.005) and sleep health scores differed between those reporting < 30 min/day and ≥ 60 min/day of MVPA (P = 0.004). Greater MVPA was associated with higher odds of having good sleep satisfaction (OR = 1.58 [1.14–2.20], P < 0.01), timing (OR = 2.07 [1.24–3.46], P < 0.01), and duration (OR = 1.48 [1.02–2.18], P = 0.04). Pedometer-based physical activity and LPA were not related to sleep health or its individual dimensions.
Conclusions
In middle- to older-aged adults, higher-intensity activity, but not lower-intensity or volume of activity, was associated with greater sleep health. These data suggest that physical activity intensity may be important for sleep health.

Similar content being viewed by others
References
Buysse DJ (2014) Sleep health: can we define it? Does it matter? Sleep 37(1):9–17. https://doi.org/10.5665/sleep.3298
Dalmases M, Benitez ID, Mas A, Garcia-Codina O, Medina-Bustos A, Escarrabill J, Salto E, Buysse DJ, Roure N, Sanchez-de-la-Torre M, Rue M, Barbe F, de Batlle J (2018) Assessing sleep health in a European population: results of the Catalan health survey 2015. PLoS One 13(4):e0194495. https://doi.org/10.1371/journal.pone.0194495
Furihata R, Hall MH, Stone KL, Ancoli-Israel S, Smagula SF, Cauley JA, Kaneita Y, Uchiyama M, Buysse DJ (2017) An aggregate measure of sleep health is associated with prevalent and incident clinically significant depression symptoms among community-dwelling older women. Sleep 40 (3):zsw075. https://doi.org/10.1093/sleep/zsw075
Jennings JR, Muldoon MF, Hall M, Buysse DJ, Manuck SB (2007) Self-reported sleep quality is associated with the metabolic syndrome. Sleep 30(2):219–223. https://doi.org/10.1093/sleep/30.2.219
Brindle RC, Cribbet MR, Samuelsson LB, Gao C, Frank E, Krafty RT, Thayer JF, Buysse DJ, Hall MH (2018) The relationship between childhood trauma and poor sleep health in adulthood. Psychosom Med 80(2):200–207. https://doi.org/10.1097/psy.0000000000000542
Wallace ML, Stone K, Smagula SF, Hall MH, Simsek B, Kado DM, Redline S, Vo TN, Buysse DJ (2018) Which sleep health characteristics predict all-cause mortality in older men? An application of flexible multivariable approaches. Sleep 41 (1):zsx189. https://doi.org/10.1093/sleep/zsx189
Irish LA, Kline CE, Gunn HE, Buysse DJ, Hall MH (2015) The role of sleep hygiene in promoting public health: a review of empirical evidence. Sleep Med Rev 22:23–36. https://doi.org/10.1016/j.smrv.2014.10.001
King AC, Oman RF, Brassington GS, Bliwise DL, Haskell WL (1997) Moderate-intensity exercise and self-rated quality of sleep in older adults. A randomized controlled trial. JAMA 277(1):32–37. https://doi.org/10.1001/jama.1997.03540250040029
Kredlow MA, Capozzoli MC, Hearon BA, Calkins AW, Otto MW (2015) The effects of physical activity on sleep: a meta-analytic review. J Behav Med 38(3):427–449. https://doi.org/10.1007/s10865-015-9617-6
Rubio-Arias JA, Marin-Cascales E, Ramos-Campo DJ, Hernandez AV, Perez-Lopez FR (2017) Effect of exercise on sleep quality and insomnia in middle-aged women: a systematic review and meta-analysis of randomized controlled trials. Maturitas 100:49–56. https://doi.org/10.1016/j.maturitas.2017.04.003
Yang PY, Ho KH, Chen HC, Chien MY (2012) Exercise training improves sleep quality in middle-aged and older adults with sleep problems: a systematic review. J Physiother 58 (3):157–163. https://doi.org/10.1016/s1836-9553(12)70106-6
Hall MH, Mulukutla S, Kline CE, Samuelsson LB, Taylor BJ, Thayer JF, Krafty RT, Frank E, Kupfer DJ (2017) Objective sleep duration is prospectively associated with endothelial health. Sleep 40 (1):zsw003. https://doi.org/10.1093/sleep/zsw003
Jake-Schoffman DE, Silfee VJ, Sreedhara M, Rosal MC, May CN, Lopez-Cepero A, Lemon SC, Haughton CF (in press) Reporting of physical activity device measurement and analysis protocols in lifestyle interventions. Am J Lifestyle Med. https://doi.org/10.1177/1559827619862179
Hasson RE, Haller J, Pober DM, Staudenmayer J, Freedson PS (2009) Validity of the Omron HJ-112 pedometer during treadmill walking. Med Sci Sports Exerc 41(4):805–809. https://doi.org/10.1249/MSS.0b013e31818d9fc2
Smith KA, Egercic L, Bramble A, Secich JJ (2017) Reliability and validity of the Omron HJ-720 ITC pedometer when worn at four different locations on the body. Cogent Med 4(1):1311461. https://doi.org/10.1080/2331205X.2017.1311461
Becker NB, Martins RIS, de Neves JS, Chiodelli R, Rieber MS (2018) Sleep health assessment: a scale validation. Psychiatry Res 259:51–55. https://doi.org/10.1016/j.psychres.2017.10.014
Ishak NAM, Ahmad S (2018) Estimating optimal parameter of Box-Cox transformation in multiple regression with non-normal data. In: Regional conference on science, technology and social sciences (RCSTSS 2016). Singapore: Springer, pp 1039–1046. https://doi.org/10.1007/978-981-13-0074-5_102
Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, George SM, Olson RD (2018) The physical activity guidelines for Americans. JAMA 320(19):2020–2028. https://doi.org/10.1001/jama.2018.14854
Tudor-Locke C, Craig CL, Thyfault JP, Spence JC (2013) A step-defined sedentary lifestyle index: < 5000 steps/day. Appl Physiol Nutr Metab 38(2):100–114. https://doi.org/10.1139/apnm-2012-0235
Richardson JT (2011) Eta squared and partial eta squared as measures of effect size in educational research. Educ Res Rev 6(2):135–147. https://doi.org/10.1016/j.edurev.2010.12.001
Achttien R, van Lieshout J, Wensing M, van der Sanden MN, Staal JB (2019) Symptoms of depression are associated with physical inactivity but not modified by gender or the presence of a cardiovascular disease; a cross-sectional study. BMC Cardiovasc Disord 19(1):95. https://doi.org/10.1186/s12872-019-1065-8
Fluetsch N, Levy C, Tallon L (2019) The relationship of physical activity to mental health: a 2015 behavioral risk factor surveillance system data analysis. J Affect Disord 253:96–101. https://doi.org/10.1016/j.jad.2019.04.086
Zhai L, Zhang H, Zhang D (2015) Sleep duration and depression among adults: a meta-analysis of prospective studies. Depress Anxiety 32(9):664–670. https://doi.org/10.1002/da.22386
Banno M, Harada Y, Taniguchi M, Tobita R, Tsujimoto H, Tsujimoto Y, Kataoka Y, Noda A (2018) Exercise can improve sleep quality: a systematic review and meta-analysis. PeerJ 6:e5172. https://doi.org/10.7717/peerj.5172
Kline CE, Sui X, Hall MH, Youngstedt SD, Blair SN, Earnest CP, Church TS (2012) Dose-response effects of exercise training on the subjective sleep quality of postmenopausal women: exploratory analyses of a randomised controlled trial. BMJ Open 2(4):e001044. https://doi.org/10.1136/bmjopen-2012-001044
Passos GS, Poyares D, Santana MG, Garbuio SA, Tufik S, de Mello MT (2010) Effect of acute physical exercise on patients with chronic primary insomnia. J Clin Sleep Med 6(3):270–275
Richards KC, Lambert C, Beck CK, Bliwise DL, Evans WJ, Kalra GK, Kleban MH, Lorenz R, Rose K, Gooneratne NS, Sullivan DH (2011) Strength training, walking, and social activity improve sleep in nursing home and assisted living residents: randomized controlled trial. J Am Geriatr Soc 59(2):214–223. https://doi.org/10.1111/j.1532-5415.2010.03246.x
Reis C, Dias S, Rodrigues AM, Sousa RD, Gregorio MJ, Branco J, Canhao H, Paiva T (2018) Sleep duration, lifestyles and chronic diseases: a cross-sectional population-based study. Sleep Sci 11(4):217–230. https://doi.org/10.5935/1984-0063.20180036
Best JR, Falck RS, Landry GJ, Liu-Ambrose T (2019) Analysis of dynamic, bidirectional associations in older adult physical activity and sleep quality. J Sleep Res 28(4):e12769. https://doi.org/10.1111/jsr.12769
Haraszti RA, Purebl G, Salavecz G, Poole L, Dockray S, Steptoe A (2014) Morningness-eveningness interferes with perceived health, physical activity, diet and stress levels in working women: a cross-sectional study. Chronobiol Int 31(7):829–837. https://doi.org/10.3109/07420528.2014.911188
Shechter A, St-Onge MP (2014) Delayed sleep timing is associated with low levels of free-living physical activity in normal sleeping adults. Sleep Med 15(12):1586–1589. https://doi.org/10.1016/j.sleep.2014.07.010
Baron KG, Reid KJ, Malkani RG, Kang J, Zee PC (2017) Sleep variability among older adults with insomnia: associations with sleep quality and cardiometabolic disease risk. Behav Sleep Med 15(2):144–157. https://doi.org/10.1080/15402002.2015.1120200
Breneman CB, Kline CE, West DS, Sui X, Porter RR, Bowyer KP, Custer S, Wang X (2019) The effect of moderate-intensity exercise on nightly variability in objectively measured sleep parameters among older women. Behav Sleep Med 17(4):459–469. https://doi.org/10.1080/15402002.2017.1395337
Buman MP, Hekler EB, Bliwise DL, King AC (2011) Exercise effects on night-to-night fluctuations in self-rated sleep among older adults with sleep complaints. J Sleep Res 20(1 Pt 1):28–37. https://doi.org/10.1111/j.1365-2869.2010.00866.x
Tudor-Locke C, Williams JE, Reis JP, Pluto D (2002) Utility of pedometers for assessing physical activity: convergent validity. Sports Med 32(12):795–808. https://doi.org/10.2165/00007256-200232120-00004
Kline CE, Irish LA, Krafty RT, Sternfeld B, Kravitz HM, Buysse DJ, Bromberger JT, Dugan SA, Hall MH (2013) Consistently high sports/exercise activity is associated with better sleep quality, continuity and depth in midlife women: the SWAN sleep study. Sleep 36(9):1279–1288. https://doi.org/10.5665/sleep.2946
Wang X, Youngstedt SD (2014) Sleep quality improved following a single session of moderate-intensity aerobic exercise in older women: results from a pilot study. J Sport Health Sci 3(4):338–342. https://doi.org/10.1016/j.jshs.2013.11.004
Chen LJ, Fox KR, Sun WJ, Tsai PS, Ku PW, Chu D (2018) Associations between walking parameters and subsequent sleep difficulty in older adults: a 2-year follow-up study. J Sport Health Sci 7(1):95–101. https://doi.org/10.1016/j.jshs.2017.01.007
Sallis JF, Saelens BE (2000) Assessment of physical activity by self-report: status, limitations, and future directions. Res Q Exerc Sport 71(2):1–14. https://doi.org/10.1080/02701367.2000.11082780
Youngstedt SD, Elliott JA, Kripke DF (2019) Human circadian phase-response curves for exercise. J Physiol 597(8):2253–2268. https://doi.org/10.1113/jp276943
Acknowledgments
The authors are grateful to all study staff and participants that made this dataset a reality for secondary analyses such as these.
Funding
This study was funded by National Institutes of Health (NIH) grant R01HL104607 (PI: Hall). Additional investigator support was provided by NIH grants K23HL118318 (PI: Kline) and R01GM113243 (PI: Krafty).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
DJB, RTK, MHH, and CEK have received grant support independent from this project from the NIH. DJB has served as a paid consultant for Weight Watchers, Bayer, and Emmi Solutions; received fees for educational products and programs sponsored by the American Academy of Physician Assistants, CME Institute, and Eisai; received licensing fees for the Pittsburgh Sleep Quality Index, copyrighted to the University of Pittsburgh, and the Consensus Sleep Diary, licensed to Ryerson University. RCB and JFT declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kubala, A.G., Buysse, D.J., Brindle, R.C. et al. The association between physical activity and a composite measure of sleep health. Sleep Breath 24, 1207–1214 (2020). https://doi.org/10.1007/s11325-019-02007-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-019-02007-x