Abstract
Background
Continuous positive airway pressure (CPAP) is considered the gold standard treatment of obstructive sleep apnea (OSA). However, it can be a challenge in some patients to find an effective CPAP setting that is well tolerated. A lower CPAP setting may improve patient tolerance of the treatment. The objective of this study was to evaluate the effect of approximately 30° torso elevation on minimum effective CPAP for the treatment of OSA.
Methods
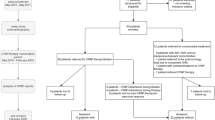
A retrospective chart review was performed to determine the effective CPAP setting required to treat OSA in patients who underwent CPAP titration with torso elevation using a wedge cushion, after having failed during the same titration study to achieve therapeutic results at CPAP of 20 cm H2O without torso elevation.
Results
Thirty-nine patients who underwent CPAP titration with and without torso elevation utilizing a wedge cushion had statistically significant lowering of the minimum effective CPAP setting with torso elevation, with a mean CPAP reduction of 4.7 (p < 0.001) compared to ineffective treatment at CPAP of 20 cm H2O without torso elevation. Apnea hypopnea index (AHI), respiratory disturbance index (RDI), and lowest oxygen saturation (SpO2) were all improved with torso elevation, with a mean AHI difference of 4.4 (p = 0.03), mean RDI difference of 14.2 (p = 0.001), and mean SpO2 difference of 5.9% (p = 0.002). Age and BMI were inversely correlated, and gender had no correlation with therapeutic CPAP settings with use of torso elevation.
Conclusion
Torso elevation of approximately 30° resulted in effective CPAP treatment at settings significantly lower than 20 cm H2O in all reviewed OSA patients, who had been ineffectively treated without torso elevation at the maximum tested setting of 20 cm H2O. This intervention may be a useful adjunct during in-lab titration studies for patients who are not effectively treated at or cannot tolerate high CPAP settings.
Similar content being viewed by others
Abbreviations
- CPAP:
-
continuous positive airway pressure
- SpO2:
-
oxygen saturation
- RDI:
-
respiratory disturbance index
- AHI:
-
apnea hypopnea index
- EDS:
-
excessive daytime sleepiness
- SHEP:
-
shoulder head elevation pillow
- Pcrit:
-
upper airway critical closing pressure
- CI:
-
confidence intervals
- OSA:
-
obstructive sleep apnea
References
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM (2013) Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 177(9):1006–1014
Somers VK, White DP, Amin R, Abraham WT, Costa F, Culebras A, Daniels S, Floras JS, Hunt CE, Olson LJ, Pickering TG, Russell R, Woo M, Young T. Sleep apnea and cardiovascular disease: an American Heart Association/American College of Cardiology Foundation scientific statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council on Cardiovascular Nursing. J Am Coll Cardiol 2008;52:686–717
Dyken ME, Im KB (2009) Obstructive sleep apnea and stroke. Chest 136:1668–1677
Sullivan CE, Issa FG, Berthon-Jones M, Eves L (1981) Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. Lancet 1:862–865
Gay P, Weaver T, Loube D, Iber C (2006) Positive Airway Pressure Task Force, Standards of Practice Committee, American Academy of Sleep Medicine. Evaluation of positive airway pressure treatment for sleep related breathing disorders in adults. Sleep 29:381–401
Kushida CA, Chediak A, Berry RB, Brown LK, Gozal D, Iber C et al (2008) Clinical guidelines for the manual titration of positive airway pressure in patients with obstructive sleep apnea. J Clin Sleep Med 4(2):157–171
Sanders MH, Kern N (1990) Obstructive sleep apnea treated by independently adjusted inspiratory and expiratory positive airway pressures via nasal mask. Physiologic and clinical implications. Chest 98:317–324
Weaver TE, Grunstein RR (2008) Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc.Am.Thorac.Soc. 5:173–178
Salepci B, Caglayan B, Kiral N, Parmaksiz ET, Comert SS, Sarac G, Fidan A, Gungor GA (2013) CPAP adherence of patients with obstructive sleep apnea. Respir Care 58:1467–1473
Oksenberg A, Silverberg DS, Arons E, Radwan H (1997) Positional vs nonpositional obstructive sleep apnea patients: anthropomorphic, nocturnal polysomnographic, and multiple sleep latency test data. Chest. 112(3):629–639
van Kesteren ER, van Maanen JP, Hilgevoord AA, Laman DM, de Vries N (2011) Quantitative effects of trunk and head position on the apnea hypopnea index in obstructive sleep apnea. Sleep 34(8):1075–1081
Cartwright RD, Diaz F, Lloyd S (1991) The effects of sleep posture and sleep stage on apnea frequency. Sleep. 14(4):351–353
Camacho M, Capasso R, Schendel S (2014) Airway changes in obstructive sleep apnoea patients associated with a supine versus an upright position examined using cone beam computed tomography. J Laryngol Otol 128(9):824–830
Neill AM, Angus SM, Sajkov D, McEvoy RD (1997) Effects of sleep posture on upper airway stability in patients with obstructive sleep apnea. Am J Respir Crit Care Med 155(1):199–204
McEvoy RD, Sharp DJ, Thornton AT (1986) The effects of posture on obstructive sleep apnea. Am Rev Respir Dis 133(4):662–666
Hakala K, Maasilta P, Sovijarvi AR (2000) Upright body position and weight loss improve respiratory mechanics and daytime oxygenation in obese patients with obstructive sleep apnoea. Clin Physiol 20(1):50–55
Hoffstein V, Zamel N, Phillipson EA (1984) Lung volume dependence of pharyngeal cross-sectional area in patients with obstructive sleep apnea. Am Rev Respir Dis 130(2):175–178
Series F, Cormier Y, Lampron N, La Forge J (1988) Increasing the functional residual capacity may reverse obstructive sleep apnea. Sleep. 11(4):349–353
Linderholm H (1963) Lung mechanics in sitting and horizontal postures studied by body plethysmographic methods. Am J Physiol--Legacy Content 204(1):85–91
Gleadhill IC, Schwartz AR, Schubert N, Wise RA, Permutt S, Smith PL (1991) Upper airway collapsibility in snorers and in patients with obstructive hypopnea and apnea. Am Rev Respir Dis 143(6):1300–1303
Brown IB, McClean PA, Boucher R, Zamel N, Hoffstein V (1987) Changes in pharyngeal cross-sectional area with posture and application of continuous positive airway pressure in patients with obstructive sleep apnea. Am Rev Respir Dis 136(3):628–632
Fouke JM, Strohl KP (1987) Effect of position and lung volume on upper airway geometry. J Appl Physiol (1985) 63(1):375–380
Skinner MA, Kingshott RN, Jones DR, Homan SD, Taylor DR (2004) Elevated posture for the management of obstructive sleep apnea. Sleep Breath 8(4):193–200
Kraiczi H, Caidahl K, Samuelsson A, Peker Y, Hedner J (2001) Impairment of vascular endothelial function and left ventricular filling : association with the severity of apnea-induced hypoxemia during sleep. Chest 119(4):1085–1091
Appleton SL, Vakulin A, McEvoy RD, Wittert GA, Martin SA, Grant JF et al (2014) Nocturnal hypoxemia and severe obstructive sleep apnea are associated with incident type 2 diabetes in a population cohort of men. J Clin Sleep Med
Redline S, Kump K, Tishler PV, Browner I, Ferrette V (1994) Gender differences in sleep disordered breathing in a community-based sample. Am J Respir Crit Care Med 149(3 Pt 1):722–726
Brooks LJ, Strohl KP (1992) Size and mechanical properties of the pharynx in healthy men and women. Am Rev Respir Dis 146(6):1394–1397
Trinder J, Kay A, Kleiman J, Dunai J (1997) Gender differences in airway resistance during sleep. J Appl Physiol (1985) 83(6):1986–1997
Souza FJ, Evangelista AR, Silva JV, Perico GV, Madeira K (2016) Cervical computed tomography in patients with obstructive sleep apnea: influence of head elevation on the assessment of upper airway volume. J Bras Pneumol 42:55–60
Redolfi S, Yumino D, Ruttanaumpawan P, Yau B, Su MC, Lam J, Bradley TD (2009) Relationship between overnight rostral fluid shift and obstructive sleep apnea in nonobese men. Am J Respir Crit Care Med 179:241–246
Pevernagie DA, Shepard JW Jr (1992) Relations between sleep stage, posture and effective nasal CPAP levels in OSA. Sleep. 15(2):162–167
Acknowledgments
The authors acknowledge Susan Hughes and Dr. Kenneth Guire for assistance with statistical analysis.
Author information
Authors and Affiliations
Contributions
MR is the guarantor of the manuscript and takes full responsibility for the integrity of this manuscript, and presented and analyzed the data. AB and MR contributed to the study design, data acquisition, data analysis, data interpretation, drafting of the manuscript, and approval of the final manuscript. GN, SR, and DO contributed to the data acquisition, data analysis, data interpretation, revision of the manuscript, and approval of the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional (University of Mississippi Medical Center) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Institutions where worked was performed: University of Mississippi Medical Center, and University of Michigan Health System
Rights and permissions
About this article
Cite this article
Riaz, M., Ravula, S., Obesso, P.D. et al. The effect of torso elevation on minimum effective continuous positive airway pressure for treatment of obstructive sleep apnea. Sleep Breath 24, 499–504 (2020). https://doi.org/10.1007/s11325-019-01880-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-019-01880-w