Abstract
Purpose
Obstructive sleep apnea (OSA) is highly prevalent in post-stroke patients and observational evidence suggests that untreated it is a harbinger of poorer outcomes in this population. Clinical trials on the impact of treatment of OSA with continuous positive airway pressure (CPAP) have countered difficulties with patient engagement and adherence to CPAP therapy. Real-world data on continuous positive airway pressure initiation and usage in the post-stroke population with obstructive sleep apnea is limited.
Methods
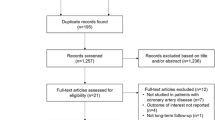
We performed a clinical retrospective study between January 2006 and June 2015 to describe the short- and long-term CPAP usage in the post-stroke population with OSA, and to assess which patient, disease, and treatment-related factors were associated with CPAP purchase, initiation, and usage in this population.
Results
Of 191 post-stroke patients’ recommended CPAP therapy, post-prescription usage at 3, 6, 12, 24, and 60 months was 58%, 53%, 48%, 45%, and 39% respectively. OSA severity-related factors, such as AHI or degree of nocturnal hypoxemia, were not significantly associated with CPAP usage. Predictors of CPAP usage at all time points were younger age, male sex, never smokers, and no history of hypertension. There were some differences in predictors of CPAP usage between early and later time periods.
Conclusions
We demonstrated that the long-term usage of CPAP therapy is possible with most of the attrition occurring in the first 3 months. Upfront healthcare resource allocation to CPAP initiation and usage in this population may improve longer-term usage.




Similar content being viewed by others
Abbreviations
- AHI:
-
apnea-hypopnea index
- BMI:
-
body mass index
- CCI:
-
Charlson comorbidity index
- CPAP:
-
continuous positive airway pressure
- ESS:
-
Epworth sleepiness scale
- IQR:
-
interquartile range
- ODI:
-
oxygen desaturation index
- OSA:
-
obstructive sleep apnea
- PSG:
-
polysomnogram
- SpO2 :
-
peripheral arterial oxygen saturation
- UHN:
-
University Health Network
References
Schwartz M, Acosta L, Hung YL, Padilla M, Enciso R (2017) Effects of CPAP and mandibular advancement device treatment in obstructive sleep apnea patients: a systematic review and meta-analysis. Sleep Breath 22:555–568. https://doi.org/10.1007/s11325-017-1590-6
Jennum P, Kjellberg J (2011) Health, social and economical consequences of sleep-disordered breathing: a controlled national study. Thorax 66(7):560–566. https://doi.org/10.1136/thx.2010.143958
Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V (2005) Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med 353(19):2034–2041
Siccoli MM, Pepperell JC, Kohler M, Craig SE, Davies RJ, Stradling JR (2008) Effects of continuous positive airway pressure on quality of life in patients with moderate to severe obstructive sleep apnea: data from a randomized controlled trial. Sleep 31(11):1551–1558
Rotenberg BW, Murariu D, Pang KP (2016) Trends in CPAP adherence over twenty years of data collection: a flattened curve. J Otolaryngol Head Neck Surg 45(1):43. https://doi.org/10.1186/s40463-016-0156-0
Lyons OD, Ryan CM (2015) Sleep apnea and stroke. Can J Cardiol 31(7):918–927. https://doi.org/10.1016/j.cjca.2015.03.014
Bravata DM, McClain V, Austin C, Ferguson J, Burrus N, Miech EJ, Matthias MS, Chumbler N, Ofner S, Foresman B, Sico J, Vaz Fragoso CA, Williams LS, Agarwal R, Concato J, Klar Yaggi H (2017) Diagnosing and managing sleep apnea in patients with chronic cerebrovascular disease: a randomized trial of a home-based strategy. Sleep Breath 21:713–725. https://doi.org/10.1007/s11325-017-1494-5
Bassetti C, Aldrich MS (1999) Sleep apnea in acute cerebrovascular diseases: final report on 128 patients. Sleep 22(2):217–223
Ryan CM, Bayley M, Green R, Murray BJ, Bradley TD (2011) Influence of continuous positive airway pressure on outcomes of rehabilitation in stroke patients with obstructive sleep apnea. Stroke 42(4):1062–1067
Birkbak J, Clark AJ, Rod NH (2014) The effect of sleep disordered breathing on the outcome of stroke and transient ischemic attack: a systematic review. J Clin Sleep Med 10(1):103–108. https://doi.org/10.5664/jcsm.3376
Rola R, Jarosz H, Wierzbicka A, Wichniak A, Richter P, Ryglewicz D, Jernajczyk W (2008) Sleep disorderd breathing and recurrence of cerebrovascular events, case-fatality, and functional outcome in patients with ischemic stroke or transient ischemic attack. J Physiol Pharmacol 59(Suppl 6):615–621
Brill AK, Horvath T, Seiler A, Camilo M, Haynes AG, Ott SR, Egger M, Bassetti CL (2018) CPAP as treatment of sleep apnea after stroke: a meta-analysis of randomized trials. Neurology 90(14):e1222–e1230. https://doi.org/10.1212/WNL.0000000000005262
Parra O, Sanchez-Armengol A, Bonnin M, Arboix A, Campos-Rodriguez F, Perez-Ronchel J, Duran-Cantolla J, de la Torre G, Gonzalez Marcos JR, de la Pena M, Carmen Jimenez M, Masa F, Casado I, Luz Alonso M, Macarron JL (2011) Early treatment of obstructive apnoea and stroke outcome: a randomised controlled trial. Eur Respir J 37(5):1128–1136
Sacco RL, Kasner SE, Broderick JP, Caplan LR, Connors JJ, Culebras A, Elkind MS, George MG, Hamdan AD, Higashida RT, Hoh BL, Janis LS, Kase CS, Kleindorfer DO, Lee JM, Moseley ME, Peterson ED, Turan TN, Valderrama AL, Vinters HV, American Heart Association Stroke Council CoCS, Anesthesia, Council on Cardiovascular R, Intervention, Council on C, Stroke N, Council on E, Prevention, Council on Peripheral Vascular D, Council on Nutrition PA, Metabolism (2013) An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 44(7):2064–2089. https://doi.org/10.1161/STR.0b013e318296aeca
American Academy of Sleep Medicine.(2014) International classification of sleep disorders
Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, Marsh EE 3rd (1993) Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 24(1):35–41
Berry R, Brooks R, Gamaldo C, Harding S, Lloyd R, Marcus C, and Vaughn B, Medicine. ftAAoS (2015) Respiratory rules for adults. In: The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications, version 2.2. American Academy of Sleep Medicine, Darien, Illinois, pp 50–56
Johns MW (1992) Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep 15(4):376–381
Charlson M, Szatrowski TP, Peterson J, Gold J (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47(11):1245–1251
Goldstein LB, Samsa GP, Matchar DB, Horner RD (2004) Charlson index comorbidity adjustment for ischemic stroke outcome studies. Stroke 35(8):1941–1945. https://doi.org/10.1161/01.STR.0000135225.80898.1c
Statistical RCTRAlaefscRFf, Computing V, Austria. (2017) A language and environment for statistical computing. R Foundation for Statistical Computing
King S, Cuellar N (2016) Obstructive sleep apnea as an independent stroke risk factor: a review of the evidence, stroke prevention guidelines, and implications for neuroscience nursing practice. J Neurosci Nurs 48(3):133–142. https://doi.org/10.1097/JNN.0000000000000196
Kaneko Y, Hajek VE, Zivanovic V, Raboud J, Bradley TD (2003) Relationship of sleep apnea to functional capacity and length of hospitalization following stroke. Sleep 26(3):293–297
Parra O, Sanchez-Armengol A, Capote F, Bonnin M, Arboix A, Campos-Rodriguez F, Perez-Ronchel J, Duran-Cantolla J, Martinez-Null C, de la Pena M, Jimenez MC, Masa F, Casadon I, Alonso ML, Macarron JL (2015) Efficacy of continuous positive airway pressure treatment on 5-year survival in patients with ischaemic stroke and obstructive sleep apnea: a randomized controlled trial. J Sleep Res 24(1):47–53. https://doi.org/10.1111/jsr.12181
Weaver TE, Grunstein RR (2008) Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc 5(2):173–178. https://doi.org/10.1513/pats.200708-119MG
Russell JO, Gales J, Bae C, Kominsky A (2015) Referral patterns and positive airway pressure adherence upon diagnosis of obstructive sleep apnea. J Neurosci Nurs 153(5):881–887. https://doi.org/10.1177/0194599815596169
Riachy M, Najem S, Iskandar M, Choucair J, Ibrahim I, Juvelikian G (2017) Factors predicting CPAP adherence in obstructive sleep apnea syndrome. Sleep Breath 21(2):295–302. https://doi.org/10.1007/s11325-016-1408-y
Kohler M, Smith D, Tippett V, Stradling JR (2010) Predictors of long-term compliance with continuous positive airway pressure. Thorax 65(9):829–832. https://doi.org/10.1136/thx.2010.135848
Tokunaga T, Ninomiya T, Kato Y, Ito Y, Takabayashi T, Tokuriki M, Sunaga H, Fujieda S (2013) Long-term compliance with nasal continuous positive airway pressure therapy for sleep apnea syndrome in an otorhinolaryngological office. J Neurosci Nurs 270(8):2267–2273. https://doi.org/10.1007/s00405-013-2483-3
Arzt M, Young T, Peppard PE, Finn L, Ryan CM, Bayley M, Bradley TD (2010) Dissociation of obstructive sleep apnea from hypersomnolence and obesity in patients with stroke. Stroke 41(3):e129–e134
Nadal N, de Batlle J, Barbe F, Marsal JR, Sanchez-de-la-Torre A, Tarraubella N, Lavega M, Sanchez-de-la-Torre M (2017) Predictors of CPAP compliance in different clinical settings: primary care versus sleep unit. Sleep Breath 22:157–163. https://doi.org/10.1007/s11325-017-1549-7
Weaver TE, Chasens ER (2007) Continuous positive airway pressure treatment for sleep apnea in older adults. Sleep Med Rev 11(2):99–111. https://doi.org/10.1016/j.smrv.2006.08.001
Russo-Magno P, O'Brien A, Panciera T, Rounds S (2001) Compliance with CPAP therapy in older men with obstructive sleep apnea. J Am Geriatr Soc 49(9):1205–1211
Lopez-Padilla D, Alonso-Moralejo R, Martinez-Garcia MA, De la Torre Carazo S, Diaz de Atauri MJ (2016) Continuous positive airway pressure and survival of very elderly persons with moderate to severe obstructive sleep apnea. Sleep Med 19:23–29. https://doi.org/10.1016/j.sleep.2015.10.015
Wessendorf TE, Wang YM, Thilmann AF, Sorgenfrei U, Konietzko N, Teschler H (2001) Treatment of obstructive sleep apnoea with nasal continuous positive airway pressure in stroke. Eur Respir J 18(4):623–629
Martinez-Garcia MA, Soler-Cataluna JJ, Ejarque-Martinez L, Soriano Y, Roman-Sanchez P, Illa FB, Canal JM, Duran-Cantolla J (2009) Continuous positive airway pressure treatment reduces mortality in patients with ischemic stroke and obstructive sleep apnea: a 5-year follow-up study. Am J Respir Crit Care Med 180(1):36–41
Chai-Coetzer CL, Luo YM, Antic NA, Zhang XL, Chen BY, He QY, Heeley E, Huang SG, Anderson C, Zhong NS, McEvoy RD (2013) Predictors of long-term adherence to continuous positive airway pressure therapy in patients with obstructive sleep apnea and cardiovascular disease in the SAVE study. Sleep 36(12):1929–1937. https://doi.org/10.5665/sleep.3232
Rauscher H, Formanek D, Popp W, Zwick H (1993) Self-reported vs measured compliance with nasal CPAP for obstructive sleep apnea. Chest 103(6):1675–1680
Fung CH, Martin JL, Hays RD, Patterson ES, Aysola R, Col N, Mitchell MN, Truong C, Dzierzewski JM, Jouldjian S, Song Y, Rodriguez JC, Josephson K, Alessi C (2017) Patient-reported usability of positive airway pressure equipment is associated with adherence in older adults. Sleep 40(3). https://doi.org/10.1093/sleep/zsx007
Kendzerska T, Gershon AS, Tomlinson G, Leung RS (2016) The effect of patient neighborhood income level on the purchase of continuous positive airway pressure treatment among patients with sleep apnea. Ann Am Thorac Soc 13(1):93–100. https://doi.org/10.1513/AnnalsATS.201505-294OC
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The work was performed at the University Health Network, Toronto, Canada.
All authors have seen and approved the manuscript.
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kendzerska, T., Wilton, K., Bahar, R. et al. Short- and long-term continuous positive airway pressure usage in the post-stroke population with obstructive sleep apnea. Sleep Breath 23, 1233–1244 (2019). https://doi.org/10.1007/s11325-019-01811-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-019-01811-9