Abstract
Purpose
The aim of the present study was to assess prevalence of associated comorbidities in a group of patients diagnosed with obstructive sleep apnea syndrome (OSAS).
Methods
This retrospective study enrolled 244 consecutive patients diagnosed by polysomnogram with OSAS between October 2010 and January 2015 after being referred to our Sleep-Related Breathing Disorders Unit, Chest Diseases Department, in the Alexandria Main University Hospital.
Results
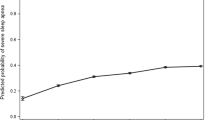
Of 244 patients, 47% were men, mean age was 56.9 years, and mean apnea–hypopnea index was 43.6 events per hour. Patients were categorized into two groups: group 1 (38%), mild and moderate OSAS, and group 2 (62%), severe, very severe, and extreme OSAS. Comorbidities were present in 91% of patients. The most common comorbidities were obesity, hypertension (HTN), and diabetes mellitus (DM). Prevalence of obesity, HTN, DM, congestive heart failure, deep vein thrombosis, pulmonary embolism (PE), and hypothyroidism was significantly higher in severity group 2. PE, bronchial asthma, and chronic obstructive pulmonary disease were significantly higher among men, whereas hypothyroidism was significantly higher among women. During this period of over 4 years, mortality rate was 8%. The majority of deaths occurred at night. Most of the studied patients (60%) either received no treatment or were not adherent to positive airway pressure (PAP) therapy. None of the patients received surgicaltreatment. The majority (50%) gained access to PAP therapy through donations. Associated hypoventilation was the only significant predictor of PAP adherence. Quality of life was significantly better among PAP adherent patients.
Conclusions
Patients suffering from OSAS have very high prevalence of comorbidities indicating a great burden on the healthcare system. Despite this fact, over 50% of the patients studied did not receive any treatment. Charities were the main portal fortreatment.





Similar content being viewed by others
References
Mohamed-Hussein AAR, Wafy S (2010) Prevalence and risk factors of obstructive sleep apnea syndrome in a population of upper Egypt. Eur Respir J 36: Suppl. 54, XXXs
Javaheri S, Caref EB, Chen E, Tong KB, Abraham WT (2011) Sleep apnea testing and outcomes in a large cohort of Medicare beneficiaries with newly diagnosed heart failure. Am J Respir Crit Care Med 183(4):539–546
World Health Organization. Division of Mental Health (1996) WHOQOL-BREF: introduction, administration, scoring and generic version of the assessment: field trial version, December 1996. World Health Organization, Geneva
Iber C, Ancoli-Israel S, Chesson AL Jr, Quan SF (2007) The AASMmanual for the scoring of sleep and associated events: rules, terminology and technical specifications, 1st edn. American Academy of Sleep Medicine, Westchester, IL
Yousif M, El-Helbawy R (2013) A six-year sleep lab experience in an Egyptian University hospital. Egyptian Journal of Chest Diseases and Tuberculosis 62:717–722
Peppard PE, Hage EW (2018) The last 25 years of obstructive sleep apnea epidemiology—and the next 25? Am J Respir Crit Care Med 197(3):310–312
Schwab RJ, Pasirstein M, Kaplan L, Pierson R, Mackley A, Hachadoorian R, Arens R, Maislin G, Pack AI (2006) Family aggregation of upper airway soft tissue structures in normal subjects and patients with sleep apnea. Am J Respir Crit Care Med 173:453–463
Basoglu OK, Tasbakan MS (2018) Gender differences in clinical and polysomnographic features of obstructive sleep apnea: a clinical study of 2827 patients. Sleep Breath 22(1):241–249
Vgontzas AN, Tan TL, Bixler EO, Martin LF, Shubert D, Kales A (1994) Sleep apnea and sleep disruption in obese patients. Arch Intern Med 154(15):1705–1711
Peppard PE, Young T, Palta M, Dempsey J, Skatrud J (2000) Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA 284:3015–3021
Garvey WT, Mechanick JI, Brett EM, Garber AJ, Hurley DL, Jastreboff AM et al (2016) American Association of Clinical Endocrinologists and American College of Endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Endocr Pract 3:1–203
Lavie P, Herer P, Hoffstein V (2000) Obstructive sleep apnoea syndrome as a risk factor for hypertension: population study. BMJ 320(7233):479–482
Shahar E, Whitney CW, Redline S, Lee ET, Newman AB, Nieto FJ et al (2001) Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med 163:19–25
Hla KM, Young T, Hagen EW, Stein JH, Finn LA, Nieto FJ, Peppard PE (2015) Coronary heart disease incidence in sleep disordered breathing: the Wisconsin Sleep Cohort Study. Sleep 38(5):677–684
Sanchez-de-la-Torre A, Soler X, Barbe F et al (2018) Cardiac troponin values in patients with acute coronary syndrome and sleep apnea. Chest 153(2):329–338
Mehra R, Benjamin EJ, Shahar E, Gottlieb DJ, Nawabit R, Kirchner HL et al (2006) Association of nocturnal arrhythmias with sleep-disordered breathing: the Sleep Heart Health Study. Am J Respir Crit Care Med 173:910–916
Gami AS, Olson EJ, Shen WK, Wright RS, Ballman KV, Hodge DO, Herges RM, Howard DE, Somers VK (2013) Obstructive sleep apnea and the risk of sudden cardiac death. J Am Coll Cardiol 62(7):610–616
Kent BD, Grote L, Ryan S, Pépin JL, Bonsignore MR, Tkacova R, Saaresranta T, Verbraecken J, Lévy P, Hedner J, McNicholas WT (2014) Diabetes mellitus prevalence and control in sleep-disordered breathing: the European Sleep Apnea Cohort (ESADA) study. Chest 146(4):982–990
Celen YT, Hedner J, Carlson J, Peker Y (2010) Impact of gender on incident diabetes mellitus in obstructive sleep apnea: a 16-year follow-up. J Clin Sleep Med 6(3):244–250
Rotenberg BW, Murariu D, Pang KP (2016) Trends in CPAP adherence over twenty years of data collection: a flattened curve. Rotenberg et al. J Otolaryngol Head Neck Surg 45:43
Frost & Sullivan (2016) Hidden health crisis costing America billions. Underdiagnosing and undertreating obstructive sleep apnea draining healthcare system. Darien, IL: American Academy of Sleep Medicine. Available from: http://www.aasmnet.org/sleep-apnea-economic-impact.aspx
Wallace DM, Williams NJ, Sawyer AM, Jean-Louis G, Aloia MS, Vieira DL, Wohlgemuth WK (2018) Adherence to positive airway pressure treatment among minority populations in the US: a scoping review. Sleep Med Rev 38:56–69
May AM, Gharibeh T, Wang L, Hurley A, Walia H, Strohl KP (2018) CPAP adherence predictors in a randomized trial of moderate-to-severe OSA enriched with women and minorities. CHEST 154(3):567–578
Balakrishnan K, James KT, Weaver EM (2016) Predicting CPAP use and treatment outcomes using composite indices of sleep apnea severity. J Clin Sleep Med 12(6):849–854
Jacobsen AR, Eriksen F, Hansen RW, Erlandsen M, Thorup L, Damgård MB, Kirkegaard MG, Hansen KW (2017) Determinants for adherence to continuous positive airway pressure therapy in obstructive sleep apnea. PLoS One 12(12):e0189614
Walter RJ, Hagedorn SI, Lettieri CJ (2017) Impact of diagnosing and treating obstructive sleep apnea on healthcare utilization. Sleep Med 38:73–77
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sweed, R.A., Hassan, S., ElWahab, N.H.A. et al. Comorbidities associated with obstructive sleep apnea: a retrospective Egyptian study on 244 patients. Sleep Breath 23, 1079–1085 (2019). https://doi.org/10.1007/s11325-019-01783-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-019-01783-w