Abstract
Background
Poor sleep quality is prevalent and is associated with cognitive decline, impaired health, and reduced quality of life. There is a lack of studies about sleep quality and its potential risk factors among rural adults aged 45 years or above under rapid urbanization in China.
Methods
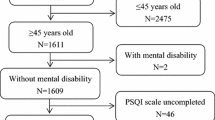
In a cross-sectional survey conducted in Deqing County, China in 2015, we included 1584 adults 45+ years of age. Sleep quality was measured by using the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI). Poor sleep quality was defined by a CPSQI global score > 5. Other data collected included sociodemographic and lifestyle factors as well as physical health. Logistic regression model was applied to assess factors influencing sleep quality by calculating crude odds ratio (cOR), adjusted OR (aOR), and their 95% confident intervals (CI).
Results
Of 1584 subjects, more than half were female with an average age of 58.9 ± 8.1 years. Their night sleep duration was 7.7 ± 1.2 h, sleep latency was 31.9 ± 32.0 min, and 17% of them could not fall asleep within half hour, averagely. The mean score of CPSQI was 4.4 ± 2.7. The prevalence of poor sleep quality was 27.7% (95% CI = 25.4–29.7%) overall, and there existed a significant sex difference—30.6% (95% CI = 27.7–33.7%) for women and 24.0% (95% CI = 20.9–27.2%) for men. Five domains of the CPSQI except for sleep efficiency and use of sleeping medication also showed a sex difference (p < 0.05). Logistic regression analysis indicated that unmarried status (aOR = 1.51, 95% CI = 1.03–2.22), lower monthly individual income (aOR = 2.09, 95% CI = 1.49–2.94), and chronic diseases (aOR = 1.95, 95% CI = 1.51–2.51) were significantly related to poor sleep quality.
Conclusions
Sleep problems were prevalent among the rural Chinese adults aged 45+ years. People who were unmarried or had low personal income or any chronic diseases were more likely to have poor sleep quality.
Similar content being viewed by others
References
Wong WS, Fielding R (2011) Prevalence of insomnia among Chinese adults in Hong Kong: a population-based study. J Sleep Res 20(1 Pt 1):117–126
Bawden FC, Oliveira CA, Caramelli P (2011) Impact of obstructive sleep apnea on cognitive performance. Arq Neuropsiquiatr 69(4):585–589
Li J, Yao YS, Dong Q, Dong YH, Liu JJ, Yang LS, Huang F (2013) Characterization and factors associated with sleep quality among rural elderly in China. Arch Gerontol Geriatr 56(1):237–243
Luo J, Zhu G, Zhao Q, Guo Q, Meng H, Hong Z, Ding D (2013a) Prevalence and risk factors of poor sleep quality among Chinese elderly in an urban community: results from the shanghai aging study. PLoS One 8(11):e81261
Manjavong M, Limpawattana P, Mairiang P, Anutrakulchai S (2016) Prevalence of insomnia and related impact[J]. Int J Psychiatry Med 51(6):544–553
Miao J, Wu X (2016) Urbanization socioeconomic status and health disparity in China. Health Place 42:87–95
Statistical Communiqué of China on 2015 National Economic and Social Development [EB/OL]. [2018/4/22]. http://www.stats.gov.cn/tjsj/zxfb/201602/t20160229_1323991.html
Yang XJ (2013) China’s rapid urbanization. Science 342(6156):310
Yu J, Li J, Cuijpers P, Wu S, Wu Z (2012) Prevalence and correlates of depressive symptoms in Chinese older adults: a population-based study. Int J Geriatr Psychiatry 27(3):305–312
Luo C, Zhang J, Pan J (2013b) One-year course and effects of insomnia in rural Chinese adolescents. Sleep 36(3):377–384
Buysse DJ, Reynolds CR, Monk TH et al (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28(2):193–213
Haseli-Mashhadi N, Pan A, Ye X et al (2009) Self-rated health in middle-aged and elderly Chinese: distribution, determinants and associations with cardio-metabolic risk factors. BMC Public Health 9:368
Zhang HS, Li Y, Mo HY, Qiu DX, Zhao J, Luo JL, Lin WQ, Wang JJ, Wang PX (2017) A community-based cross-sectional study of sleep quality in middle-aged and older adults. Qual Life Res 26(4):923–933
Poland RE, Rao U, Lutchmansingh P, McCracken JT, Lesser IM, Edwards C, Ott GE, Lin KM (1999) REM sleep in depression is influenced by ethnicity. Psychiatry Res 88(2):95–105
Jean-Louis G, Magai CM, Cohen CI, Zizi F, von Gizycki H, DiPalma J, Casimir GJ (2001) Ethnic differences in self-reported sleep problems in older adults. Sleep 24(8):926–933
Hale L, Do DP (2007) Racial differences in self-reports of sleep duration in a population-based study. Sleep 30(9):1096–1103
Report on the work of the Deqing Government [EB/OL]. [2018/4/23]. http://www.deqing.gov.cn/art/2017/2/23/art_9378_289833.html
Fu CW, Chen Y, Wang F, Jiang QW (2012) Chronic diseases in adults living in rural communities of China: World Congress on Public Health World Health Organization
Tsai PS, Wang SY, Wang MY, Su CT, Yang TT, Huang CJ, Fang SC (2005) Psychometric evaluation of the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI) in primary insomnia and control subjects. Qual Life Res 14(8):1943–1952
WHO|Physical activity [EB/OL]. [2018/4/26].http://www.who.int/topics/physical_activity/en/
(2000) Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 894:1–253
Su TP, Huang SR, Chou P (2004) Prevalence and risk factors of insomnia in community-dwelling Chinese elderly: a Taiwanese urban area survey. Aust N Z J Psychiatry 38(9):706–713
Liu X, Liu L (2005) Sleep habits and insomnia in a sample of elderly persons in China. Sleep 28(12):1579–1587
Xiang YT, Ma X, Cai ZJ, Li SR, Xiang YQ, Guo HL, Hou YZ, Li ZB, Li ZJ, Tao YF, Dang WM, Wu XM, Deng J, Lai KYC, Ungvari GS (2008) The prevalence of insomnia, its sociodemographic and clinical correlates, and treatment in rural and urban regions of Beijing, China: a general population-based survey. Sleep 31(12):1655–1662
Roth T, Ancoli-Israel S (1999) Daytime consequences and correlates of insomnia in the United States: results of the 1991 National Sleep Foundation survey. II. Sleep 22(Suppl 2):S354–S358
Shochat T, Ancoli-Israel S (2017) Chapter 153—insomnia in older adults. In: Kryger A, Meir M, Roth T, Dement WC (eds) Principles and practice of sleep medicine, sixth edn. Elsevier, pp 1503–1509
Murphy F (2006) Loneliness: a challenge for nurses caring for older people. Nurs Older People 18(5):22–25
Breslau N, Roth T, Rosenthal L, Andreski P (1996) Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biol Psychiatry 39(6):411–418
Yeo BK, Perera IS, Kok LP, Tsoi WF (1996) Insomnia in the community. Singap Med J 37(3):282–284
Zhang B, Wing YK (2006) Sex differences in insomnia: a meta-analysis. Sleep 29(1):85–93
Lu CH, Wang PX, Lei YX, Luo ZC (2014) Influence of health-related quality of life on health service utilization in Chinese rural-to-urban female migrant workers. Health Qual Life Outcomes 12:121
Ohayon M (1996) Epidemiological study on insomnia in the general population. Sleep 19(3 Suppl):S7–S15
Tseng HC, Wang CJ, Cheng SH, Sun ZJ, Chen PS, Lee CT, Lin SH, Yang YK, Yang YC (2014) Tea-drinking habit among new university students: associated factors. Kaohsiung J Med Sci 30(2):98–103
Garaulet M, Ortega FB, Ruiz JR, Rey-López JP, Béghin L, Manios Y, Cuenca-García M, Plada M, Diethelm K, Kafatos A, Molnár D, al-Tahan J, Moreno LA (2011) Short sleep duration is associated with increased obesity markers in European adolescents: effect of physical activity and dietary habits. The HELENA study. Int J Obes 35(10):1308–1317
Zhejiang Statistical Yearbook 2014[R]. Beijing: Zhejiang Provincial Bureau of Statistics, 2014
Funding
National Natural Science Foundation of China and Shanghai Government provided financial support in the form of the National Natural Science Foundation of China (81473038), Shanghai 3-Year Public Health Action Plan (GWTD2015S04), and Shanghai Leading Academic Discipline Project of Public Health (15GWZK80101). The sponsor had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Review Board of the Fudan University School of Public Health and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Dong, X., Wang, Y., Chen, Y. et al. Poor sleep quality and influencing factors among rural adults in Deqing, China. Sleep Breath 22, 1213–1220 (2018). https://doi.org/10.1007/s11325-018-1685-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-018-1685-8