Abstract
Purpose
The NoSAS score was developed to identify subjects at high risk of sleep-disordered breathing (SDB). We aimed to validate the NoSAS score in a multiethnic Asian cohort and compare its performance to the STOP-Bang and Berlin questionnaires.
Methods
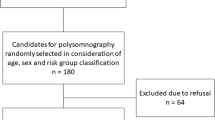
A sample of 242 subjects selected from a population-based cohort in Singapore completed home-based sleep testing with an Embletta device (type 3 monitor). All subjects were given the STOP-Bang and Berlin questionnaires for self-administration prior to the sleep study. The NoSAS score was subsequently calculated based on available demographic data and Berlin questionnaire responses.
Results
The prevalence of severe SDB, defined as an apnea-hypopnea index cutoff of ≥30 events/h, was 10.7%. The number of subjects who were classified as high risk by the NoSAS score and STOP-Bang and Berlin questionnaires were 76 (31.4%), 89 (36.8%), and 79 (32.6%), respectively. The sensitivity, specificity, and negative and positive predictive values of the NoSAS score to predict severe SDB were 69.2, 73.1, 95.2, and 23.7%, respectively. The STOP-Bang and Berlin questionnaires performed similarly to the NoSAS score, with area under the curve (AUC) values of all three questionnaires clustered around 0.682–0.748. Compared to the STOP-Bang (94.8%) and Berlin questionnaires (96.3%), the NoSAS score (95.2%) had equally high negative predictive value in ruling out severe SDB.
Conclusions
The NoSAS score performed similarly to the STOP-Bang and Berlin questionnaires in a multiethnic Asian cohort. All three questionnaires had high negative predictive values in ruling out severe SDB and may have utility as screening tools.
Similar content being viewed by others
Abbreviations
- SDB:
-
Sleep-disordered breathing
- AHI:
-
Apnea-hypopnea index
- AASM,:
-
American Academy of Sleep Medicine
- PSG:
-
Polysomnography
- BMI:
-
Body mass index
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
- AUC:
-
Area under the curve
- PSQI:
-
Pittsburg Sleep Quality Index
- SpO2 :
-
Oxygen saturation as measured by pulse oximetry.
References
Heinzer R, Vat S, Marques-Vidal P, Marti-Soler H, Andries D, Tobback N, Mooser V, Preisig M, Malhotra A, Waeber G, Vollenweider P, Tafti M, Haba-Rubio J (2015) Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. The Lancet Respiratory medicine 3(4):310–318. doi:10.1016/s2213-2600(15)00043-0
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM (2013) Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 177(9):1006–1014. doi:10.1093/aje/kws342
Chen X, Wang R, Zee P, Lutsey PL, Javaheri S, Alcantara C, Jackson CL, Williams MA, Redline S (2015) Racial/ethnic differences in sleep disturbances: the multi-ethnic study of atherosclerosis (MESA). Sleep 38(6):877–888. doi:10.5665/sleep.4732
Redline S, Sotres-Alvarez D, Loredo J, Hall M, Patel SR, Ramos A, Shah N, Ries A, Arens R, Barnhart J, Youngblood M, Zee P, Daviglus ML (2014) Sleep-disordered breathing in Hispanic/Latino individuals of diverse backgrounds. The Hispanic community health study/study of Latinos. Am J Respir Crit Care Med 189(3):335–344. doi:10.1164/rccm.201309-1735OC
Watson NF (2016) Health care savings: the economic value of diagnostic and therapeutic care for obstructive sleep apnea. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine 12(8):1075–1077. doi:10.5664/jcsm.6034
Flemons WW, Douglas NJ, Kuna ST, Rodenstein DO, Wheatley J (2004) Access to diagnosis and treatment of patients with suspected sleep apnea. Am J Respir Crit Care Med 169(6):668–672. doi:10.1164/rccm.200308-1124PP
Qaseem A, Dallas P, Owens DK, Starkey M, Holty JE, Shekelle P (2014) Diagnosis of obstructive sleep apnea in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med 161(3):210–220. doi:10.7326/m12-3187
Chung F, Yegneswaran B, Liao P, Chung SA, Vairavanathan S, Islam S, Khajehdehi A, Shapiro CM (2008) STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology 108(5):812–821. doi:10.1097/ALN.0b013e31816d83e4
Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP (1999) Using the Berlin questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med 131(7):485–491
Marti-Soler H, Hirotsu C, Marques-Vidal P, Vollenweider P, Waeber G, Preisig M, Tafti M, Tufik SB, Bittencourt L, Tufik S, Haba-Rubio J, Heinzer R (2016) The NoSAS score for screening of sleep-disordered breathing: a derivation and validation study. The Lancet Respiratory medicine. doi:10.1016/s2213-2600(16)30075-3
Tan A, Cheung YY, Yin J, Lim WY, Tan LW, Lee CH (2016) Prevalence of sleep-disordered breathing in a multiethnic Asian population in Singapore: a community-based study. Respirology (Carlton, Vic) 21(5):943–950. doi:10.1111/resp.12747
Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK, Marcus CL, Mehra R, Parthasarathy S, Quan SF, Redline S, Strohl KP, Davidson Ward SL, Tangredi MM (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine 8(5):597–619. doi:10.5664/jcsm.2172
Lee RW, Vasudavan S, Hui DS, Prvan T, Petocz P, Darendeliler MA, Cistulli PA (2010) Differences in craniofacial structures and obesity in Caucasian and Chinese patients with obstructive sleep apnea. Sleep 33(8):1075–1080
Li KK, Kushida C, Powell NB, Riley RW, Guilleminault C (2000) Obstructive sleep apnea syndrome: a comparison between far-east Asian and white men. Laryngoscope 110(10 Pt 1):1689–1693. doi:10.1097/00005537-200010000-00022
Arnardottir ES, Bjornsdottir E, Olafsdottir KA, Benediktsdottir B, Gislason T (2016) Obstructive sleep apnoea in the general population: highly prevalent but minimal symptoms. The European respiratory journal 47(1):194–202. doi:10.1183/13993003.01148-2015
Bixler EO, Vgontzas AN, Gaines J, Fernandez-Mendoza J, Calhoun SL, Liao D (2016) Moderate sleep apnoea: a "silent" disorder, or not a disorder at all? The European respiratory journal 47(1):23–26. doi:10.1183/13993003.01955-2015
Vat S, Haba-Rubio J, Tafti M, Tobback N, Andries D, Heinzer R (2015) Scoring criteria for portable monitor recordings: a comparison of four hypopnoea definitions in a population-based cohort. Thorax 70(11):1047–1053. doi:10.1136/thoraxjnl-2014-205982
Acknowledgments
The authors thank the staff of Easmed Private Limited, for their assistance with the home-based sleep studies; Venesa Loh and Tan Ching Yee with the patient recruitment; and Glenn Rolden (RGPST) and Hafiz Firdaus Bin Abdul Haddy for the analysis of the sleep tracings.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by the FY2014 Health Services Research and Quality Improvement Grant of Ng Teng Fong General Hospital, Jurong Health Services.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study has been approved by the ethics committee of the participating hospital and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Tan, A., Hong, Y., Tan, L.W. et al. Validation of NoSAS score for screening of sleep-disordered breathing in a multiethnic Asian population. Sleep Breath 21, 1033–1038 (2017). https://doi.org/10.1007/s11325-016-1455-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-016-1455-4