Abstract
Objectives
The objective of this investigation was to assess the correlation between the mandible and cervical vertebrae bone marrow apparent diffusion coefficient (ADC), obtained by diffusion-weighted magnetic resonance imaging (DWI), with age; to verify the correlation between ADC values from the mandible and the cervical vertebrae; to describe and assess the differences between ADC values obtained from DWI examinations of distinct mandible areas as well as cervical vertebrae.
Methods
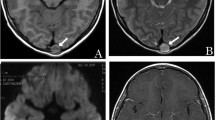
Thirty imaging examinations with DWI for that included the mandible and C1, C2, C3, and C4 vertebrae in the same examination were included. ADC values were collected from 7 distinct areas in the mandible and the cervical vertebrae. Differences between ADC values and non-parametric correlations were performed.
Results
A total of 270 regions were assessed. No significant difference was found between ADC values of all areas tested. An inverse correlation was found between C2, C3, and C4 vertebrae ADC values and age.
The significant correlation of anatomic area ADC values and age were presented as graphics to verify if the linear trend of ADC values and age are in accordance with the literature
Conclusions
The mandible area that most correlates with the cervical vertebrae, using ADC values, is the posterior trabecular area, below the inferior molars. Also, C2, C3, and C4 vertebrae ADC values inversely correlate with age, which demonstrates the bone qualitative changes in bone composition. ADC values may be useful for the qualitative assessment of bone quality to screen patients at osteoporosis risk.





Similar content being viewed by others
References
Travlos GS. Normal structure, function, and histology of the bone marrow. Toxicol Pathol. 2006;34(5):548–65. https://doi.org/10.1080/01926230600939856.
Ambrosi TH, Schulz TJ. The emerging role of bone marrow adipose tissue in bone health and dysfunction. J Mol Med (Berl). 2017;95(12):1291–301. https://doi.org/10.1007/s00109-017-1604-7.
Vande Berg BC, Malghem J, Lecouvet FE, Maldague B. Magnetic resonance imaging of normal bone marrow. Eur Radiol. 1998;8(8):1327–34. https://doi.org/10.1007/s003300050547.
Justesen J, Stenderup K, Ebbesen EN, Mosekilde L, Steiniche T, Kassem M. Adipocyte tissue volume in bone marrow is increased with aging and in patients with osteoporosis. Biogerontology. 2001;2(3):165–71. https://doi.org/10.1023/a:1011513223894.
Fazeli PK, Horowitz MC, MacDougald OA, Scheller EL, Rodeheffer MS, Rosen CJ, et al. Marrow fat and bone–new perspectives. J Clin Endocrinol Metab. 2013;98(3):935–45. https://doi.org/10.1210/jc.2012-3634.
Paccou J, Penel G, Chauveau C, Cortet B, Hardouin P. Marrow adiposity and bone: review of clinical implications. Bone. 2019;118:8–15. https://doi.org/10.1016/j.bone.2018.02.008.
Choi I, Munhoz L, Arita ES. Assessment of osteoporotic alterations in Brazilian postmenopausal women: a retrospective study. J Clin Dental Res. 2018;12(5):ZC34–7. https://doi.org/10.7860/JCDR/2018/34529.11566.
Fathi Kazerooni A, Pozo JM, McCloskey EV, Saligheh Rad H, Frangi AF. Diffusion MRI for assessment of bone quality; a review of findings in healthy aging and osteoporosis. J Magn Reson Imaging. 2019. https://doi.org/10.1002/jmri.26973.
Griffith JF, Genant HK. New advances in imaging osteoporosis and its complications. Endocrine. 2012;42(1):39–51. https://doi.org/10.1007/s12020-012-9691-2.
Munhoz L, Ramos EADA, Im DC, Hisatomi M, Yanagi Y, Asaumi J, et al. Application of diffusion-weighted magnetic resonance imaging in the diagnosis of salivary gland diseases: a systematic review. Oral Surg Oral Med Oral Pathol Oral Radiol. 2019. https://doi.org/10.1016/j.oooo.2019.02.020.
Munhoz L, Abdala Júnior R, Abdala R, Arita ES. Diffusion-weighted magnetic resonance imaging of the paranasal sinuses: a systematic review. Oral Surg Oral Med Oral Pathol Oral Radiol. 2018. https://doi.org/10.1016/j.oooo.2018.07.004.
Filograna L, Magarelli N, Cellini F, Manfrida S, Leone A, Colosimo C, et al. Diffusion weighted imaging (DWI) and apparent diffusion coefficient (ADC) values for detection of malignant vertebral bone marrow lesions. Eur Rev Med Pharmacol Sci. 2018;22(3):590–7. https://doi.org/10.26355/eurrev_201802_14273.
Munhoz L, Abdala Júnior R, Arita ES. The value of the apparent diffusion coefficient calculated from diffusion-weighted magnetic resonance imaging scans in the differentiation of maxillary sinus inflammatory diseases. Oral Surg Oral Med Oral Pathol Oral Radiol. 2018. https://doi.org/10.1016/j.oooo.2018.11.013.
Munhoz L, Abdala Júnior R, Abdala R, Asaumi J, Arita ES. Diffusion-weighted magnetic resonance imaging in maxillary sinuses inflammatory diseases: report of three cases and literature review. J Oral Maxillofac Res. 2018;9(2):e4. https://doi.org/10.5037/jomr.2018.9204.
Goodsitt MM, Hoover P, Veldee MS, Hsueh SL. The composition of bone marrow for a dual-energy quantitative computed tomography technique. A cadaver and computer simulation study. Invest Radiol. 1994;29(7):695–704. https://doi.org/10.1097/00004424-199407000-00006.
Chen WT, Shih TT, Chen RC, Lo HY, Chou CT, Lee JM, et al. Blood perfusion of vertebral lesions evaluated with gadolinium-enhanced dynamic MRI: in comparison with compression fracture and metastasis. J Magn Reson Imaging. 2002;15(3):308–14. https://doi.org/10.1002/jmri.10063.
Capuani S, Manenti G, Iundusi R, Tarantino U. Focus on diffusion MR investigations of musculoskeletal tissue to improve osteoporosis diagnosis: a brief practical review. Biomed Res Int. 2015;2015:948610. https://doi.org/10.1155/2015/948610.
Munhoz L, Aoki EM, Cortes ARG, de Freitas CF, Arita ES. Osteoporotic alterations in a group of different ethnicity Brazilian postmenopausal women: an observational study. Gerodontology. 2018. https://doi.org/10.1111/ger.12322.
Munhoz L, Cortes AR, Arita ES. Assessment of osteoporotic alterations in type 2 diabetes: a retrospective study. Dentomaxillofac Radiol. 2017. https://doi.org/10.1259/dmfr.20160414.
Colantonio DF, Saxena SK, Vanier A, Rodkey D, Tintle S, Wagner SC. Cervical spine computed tomography Hounsfield units accurately predict low bone mineral density of the femoral neck. Clin Spine Surg. 2019. https://doi.org/10.1097/BSD.0000000000000879.
Cheade MCC, Munhoz L, Arita ES, Watanabe PCA. Opportunistic screening for osteoporosis correlating the bone densities of jaws with multislice computed tomography for cervical vertebrae. Clin Lab Res Dent. 2019. https://doi.org/10.11606/issn.2357-8041.clrd.2019.155263.
Barngkgei I, Joury E, Jawad A. An innovative approach in osteoporosis opportunistic screening by the dental practitioner: the use of cervical vertebrae and cone beam computed tomography with its viewer program. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;120(5):651–9. https://doi.org/10.1016/j.oooo.2015.08.008.
Schreiber JJ, Anderson PA, Rosas HG, Buchholz AL, Au AG. Hounsfield units for assessing bone mineral density and strength: a tool for osteoporosis management. J Bone Joint Surg Am. 2011;93(11):1057–63. https://doi.org/10.2106/JBJS.J.00160.
Wagner SC, Dworak TC, Grimm PD, Balazs GC, Tintle SM. Measurement of distal ulnar Hounsfield units accurately predicts bone mineral density of the forearm. J Bone Joint Surg Am. 2017;99(8):e38. https://doi.org/10.2106/JBJS.15.01244.
Wagner SC, Formby PM, Helgeson MD, Kang DG. Diagnosing the undiagnosed: osteoporosis in patients undergoing lumbar fusion. Spine. 2016;41(21):E1279–83. https://doi.org/10.1097/BRS.0000000000001612.
Formby PM, Kang DG, Helgeson MD, Wagner SC. Clinical and radiographic outcomes of transforaminal lumbar interbody fusion in patients with osteoporosis. Global Spine J. 2016;6(7):660–4. https://doi.org/10.1055/s-0036-1578804.
Klemetti E, Kolmakov S, Kröger H. Pantomography in assessment of the osteoporosis risk group. Scand J Dent Res. 1994;102(1):68–72.
Estrugo-Devesa A, Segura-Egea J, García-Vicente L, Schemel-Suárez M, Blanco-Carrrión Á, Jané-Salas E, et al. Correlation between mandibular bone density and skeletal bone density in a Catalonian postmenopausal population. Oral Surg Oral Med Oral Pathol Oral Radiol. 2018;125(5):495–502. https://doi.org/10.1016/j.oooo.2017.10.003.
Padhani AR, Koh DM, Collins DJ. Whole-body diffusion-weighted MR imaging in cancer: current status and research directions. Radiology. 2011;261(3):700–18. https://doi.org/10.1148/radiol.11110474.
Agrawal K, Agarwal Y, Chopra RK, Batra A, Chandra R, Thukral BB. Evaluation of MR spectroscopy and diffusion-weighted MRI in postmenopausal bone strength. Cureus. 2015;7(9):e327. https://doi.org/10.7759/cureus.327.
He J, Fang H, Na LX. Vertebral bone marrow diffusivity in normal adults with varying bone densities at 3T diffusion-weighted imaging. Acta Radiol. 2018;59(1):89–96. https://doi.org/10.1177/0284185117704235.
Momeni M, Asadzadeh M, Mowla K, Hanafi MG, Gharibvand MM, Sahraeizadeh A. Sensitivity and specificity assessment of DWI and ADC for the diagnosis of osteoporosis in postmenopausal patients. Radiol Med. 2020;125(1):68–74. https://doi.org/10.1007/s11547-019-01080-2.
Pernow Y, Hauge EM, Linder K, Dahl E, Sääf M. Bone histomorphometry in male idiopathic osteoporosis. Calcif Tissue Int. 2009;84(6):430–8. https://doi.org/10.1007/s00223-009-9239-5.
Griffith JF, Yeung DK, Ahuja AT, Choy CW, Mei WY, Lam SS, et al. A study of bone marrow and subcutaneous fatty acid composition in subjects of varying bone mineral density. Bone. 2009;44(6):1092–6. https://doi.org/10.1016/j.bone.2009.02.022.
Kiebzak GM. Age-related bone changes. Exp Gerontol. 1991;26(2–3):171–87. https://doi.org/10.1016/0531-5565(91)90010-j.
Schellinger D, Lin CS, Lim J, Hatipoglu HG, Pezzullo JC, Singer AJ. Bone marrow fat and bone mineral density on proton MR spectroscopy and dual-energy X-ray absorptiometry: their ratio as a new indicator of bone weakening. AJR Am J Roentgenol. 2004;183(6):1761–5. https://doi.org/10.2214/ajr.183.6.01831761.
Hatipoglu HG, Selvi A, Ciliz D, Yuksel E. Quantitative and diffusion MR imaging as a new method to assess osteoporosis. AJNR Am J Neuroradiol. 2007;28(10):1934–7. https://doi.org/10.3174/ajnr.A0704.
Yeung DK, Wong SY, Griffith JF, Lau EM. Bone marrow diffusion in osteoporosis: evaluation with quantitative MR diffusion imaging. J Magn Reson Imaging. 2004;19(2):222–8. https://doi.org/10.1002/jmri.10453.
Griffith JF, Yeung DK, Antonio GE, Wong SY, Kwok TC, Woo J, et al. Vertebral marrow fat content and diffusion and perfusion indexes in women with varying bone density: MR evaluation. Radiology. 2006;241(3):831–8. https://doi.org/10.1148/radiol.2413051858.
Tang GY, Lv ZW, Tang RB, Liu Y, Peng YF, Li W, et al. Evaluation of MR spectroscopy and diffusion-weighted MRI in detecting bone marrow changes in postmenopausal women with osteoporosis. Clin Radiol. 2010;65(5):377–81. https://doi.org/10.1016/j.crad.2009.12.011.
Coutel X, Olejnik C, Marchandise P, Delattre J, Béhal H, Kerckhofs G, et al. A novel microCT method for bone and marrow adipose tissue alignment identifies key differences between mandible and tibia in rats. Calcif Tissue Int. 2018;103(2):189–97. https://doi.org/10.1007/s00223-018-0397-1.
Lanske B, Rosen C. Bone marrow adipose tissue: the first 40 years. J Bone Miner Res. 2017;32(6):1153–6. https://doi.org/10.1002/jbmr.3140.
Mavropoulos A, Odman A, Ammann P, Kiliaridis S. Rehabilitation of masticatory function improves the alveolar bone architecture of the mandible in adult rats. Bone. 2010;47(3):687–92. https://doi.org/10.1016/j.bone.2010.06.025.
Allen MR. The effects of bisphosphonates on jaw bone remodeling, tissue properties, and extraction healing. Odontology. 2011;99(1):8–17. https://doi.org/10.1007/s10266-010-0153-0.
Blake GM, Fogelman I. How important are BMD accuracy errors for the clinical interpretation of DXA scans? J Bone Miner Res. 2008;23(4):457–62. https://doi.org/10.1359/jbmr.071119.
Zhang L, Wang Q, Wu X, Zhao A, Feng J, Zhang H, et al. Baseline bone marrow ADC value of diffusion-weighted MRI: a potential independent predictor for progression and death in patients with newly diagnosed multiple myeloma. Eur Radiol. 2021;31(4):1843–52. https://doi.org/10.1007/s00330-020-07295-6.
Funding
No funding was available for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Luciana Munhoz, Isabela Choi, Reinaldo Abdala Junior and Emiko Saito Arita declare no conflict of interest.
Ethics approval
Ethics committee approval was obtained for this study (number 2.441.500), and the guidelines of the Helsinki Declaration were followed in this investigation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Munhoz, L., Abdala Júnior, R., Choi, I.G.G. et al. Diffusion-weighted magnetic resonance imaging of mandibular bone marrow: do apparent diffusion coefficient values of the cervical vertebrae and mandible correlate with age?. Oral Radiol 38, 72–79 (2022). https://doi.org/10.1007/s11282-021-00528-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11282-021-00528-4