Abstract
Purpose
Commonly used comorbidity indices include the Charlson Comorbidity Index (CCI), Elixhauser/Van Walraven Index (VWI), and modified frailty index (mFI). This study evaluates whether these indices predict postoperative readmissions and complications after inflatable penile prosthesis (IPP) and artificial urinary sphincter (AUS) placement.
Methods
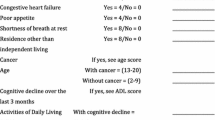
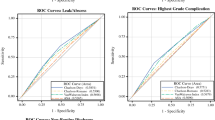
We identified adult males who underwent IPP or AUS placement using the State Inpatient and State Ambulatory Surgery and Services Databases for Florida (2010–2015) and California (2010–2011). CCI, VWI, and mFI scores were calculated for each patient. We extracted 30-day emergency department services, 30-day readmissions, 90-day device complications (e.g., removal, replacement, or infection), and 90-day postoperative complications (excluding device complications). Receiver-operating characteristic curves were constructed and areas under the curve (AUC) were compared between the indices using the VWI as the reference model. We considered an AUC < 0.7 to represent poor predictive power.
Results
We identified 4242 IPP and 1190 AUS patients. All three indices had AUCs and 95% confidence intervals less than 0.70 for all outcomes following IPP and AUS placement making these indices poor predictors for postoperative outcomes. There were no significant differences in predicting 90-day postoperative complications between the VWI (AUC = 0.59, 95% CI [0.54–0.63]), CCI (AUC = 0.59, 95% CI [0.54–0.63], p = 0.99), and mFI (AUC = 0.60, 95% CI [0.55–0.66], p = 0.53) for IPPs and VWI (AUC = 0.54, 95% CI [0.47–0.61]), CCI (AUC = 0.50, 95% CI [0.43–0.57], p = 0.30), and mFI (AUC = 0.52, 95% CI [0.43–0.60], p = 0.56) for AUS placements.
Conclusion
All three comorbidity indices were poor predictors of readmissions and complications following urologic prosthetic surgeries. A better comorbidity index is needed for risk-stratification of patients undergoing these surgeries.


Similar content being viewed by others
Data availability
Data analyzed for this project can be obtained from Healthcare Cost and Utilization Project (HCUP) databases located on the Agency for Healthcare Research and Quality website.
References
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383. https://doi.org/10.1016/0021-9681(87)90171-8
van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ (2009) A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care 47(6):626–633. https://doi.org/10.1097/MLR.0b013e31819432e5
Elixhauser A, Steiner C, Harris DR, Coffey RM (1998) Comorbidity measures for use with administrative data. Med Care 36(1):8–27. https://doi.org/10.1097/00005650-199801000-00004
Koohestani D, Chobrutskiy BI, Janjua H, Velanovich V (2022) The accumulating deficits model for postoperative mortality and readmissions: comparison of four methods over multiple calendar year cohorts. Ann Surg 276(2):293–297. https://doi.org/10.1097/sla.0000000000004421
McFerrin C, Raza SJ, May A, Davaro F, Siddiqui S, Hamilton Z (2019) Charlson comorbidity score is associated with readmission to the index operative hospital after radical cystectomy and correlates with 90-day mortality risk. Int Urol Nephrol 51(10):1755–1762. https://doi.org/10.1007/s11255-019-02247-6
Voskuijl T, Hageman M, Ring D (2014) Higher Charlson Comorbidity Index Scores are associated with readmission after orthopaedic surgery. Clin Orthop Relat Res 472(5):1638–1644. https://doi.org/10.1007/s11999-013-3394-8
Coyan GN, Chin H, Shah A, Miguelino AM, Wang Y, Kilic A, Sultan I, Sciortino CM, Chu D (2022) Charlson comorbidity index is associated with longer-term mortality and re-admissions following coronary artery bypass grafting. J Surg Res 275:300–307. https://doi.org/10.1016/j.jss.2022.02.012
Varady NH, Gillinov SM, Yeung CM, Rudisill SS, Chen AF (2021) The Charlson and Elixhauser Scores outperform the american society of anesthesiologists score in assessing 1-year mortality risk after hip fracture surgery. Clin Orthop Relat Res 479(9):1970–1979. https://doi.org/10.1097/corr.0000000000001772
Hinton ZW, Fletcher AN, Ryan SP, Wu CJ, Bolognesi MP, Seyler TM (2021) Body Mass Index, American Society of Anesthesiologists Score, and Elixhauser comorbidity index predict cost and delay of care during total knee arthroplasty. J Arthroplasty 36(5):1621–1625. https://doi.org/10.1016/j.arth.2020.12.016
Rios-Diaz AJ, Zheng R, Thibault DP, Crispo JAG, Willis AW, Willis AI (2019) Understanding nationwide readmissions after thyroid surgery. Surgery 165(2):423–430. https://doi.org/10.1016/j.surg.2018.09.007
Traven SA, McGurk KM, Reeves RA, Walton ZJ, Woolf SK, Slone HS (2019) Modified frailty index predicts medical complications, length of stay, readmission, and mortality following total shoulder arthroplasty. J Shoulder Elbow Surg 28(10):1854–1860. https://doi.org/10.1016/j.jse.2019.03.009
McChesney SL, Canter DJ, Monlezun DJ, Green H, Margolin DA (2020) Modified Frailty Index predicts postoperative outcomes in patients undergoing radical pelvic surgery. Am Surg 86(2):95–103
Al-Khamis A, Warner C, Park J, Marecik S, Davis N, Mellgren A, Nordenstam J, Kochar K (2019) Modified frailty index predicts early outcomes after colorectal surgery: an ACS-NSQIP study. Colorectal Dis 21(10):1192–1205. https://doi.org/10.1111/codi.14725
Medendorp AR, Anger JT, Jin C, Amin KA, Hampson LA, Lee UJ, Suskind AM (2019) The impact of frailty on artificial urinary sphincter placement and removal procedures. Urology 129:210–216. https://doi.org/10.1016/j.urology.2019.04.015
Inouye BM, Sexton SJ, Boysen WR, Kowalik U, Truong T, Kuchibhatla M, Peterson AC (2021) Increasing comorbidity and frailty is not associated with early postoperative complications among men undergoing artificial urinary sphincter or sling implantation: a real-world application of NSQIP® data to reconstructive urology. Urology Practice 8(2):264–269. https://doi.org/10.1097/UPJ.0000000000000199
Beilan J, Strakosha R, Palacios DA, Rosser CJ (2014) The Postoperative Morbidity Index: a quantitative weighing of postoperative complications applied to urological procedures. BMC Urol 14:1. https://doi.org/10.1186/1471-2490-14-1
Chung E, Van CT, Wilson I, Cartmill RA (2013) Penile prosthesis implantation for the treatment for male erectile dysfunction: clinical outcomes and lessons learnt after 955 procedures. World J Urol 31(3):591–595. https://doi.org/10.1007/s00345-012-0859-4
Alwaal A, Harris CR, Awad MA, Allen IE, Breyer BN (2016) Comparison of complication rates related to male urethral slings and artificial urinary sphincters for urinary incontinence: national multi-institutional analysis of ACS-NSQIP database. Int Urol Nephrol 48(10):1571–1576. https://doi.org/10.1007/s11255-016-1347-3
Quality AfHRa Introduction to the HCUP State Inpatient Databases (SID). https://www.hcup-us.ahrq.gov/db/state/siddist/SID_Introduction.jsp. Accessed Feb 11 2023
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA (2005) Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 43(11):1130–1139. https://doi.org/10.1097/01.mlr.0000182534.19832.83
Mitnitski AB, Mogilner AJ, Rockwood K (2001) Accumulation of deficits as a proxy measure of aging. Sci World J 1:323–336. https://doi.org/10.1100/tsw.2001.58
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44(3):837–845
Jiang R, Wolf S, Alkazemi MH, Pomann GM, Purves JT, Wiener JS, Routh JC (2018) The evaluation of three comorbidity indices in predicting postoperative complications and readmissions in pediatric urology. J Pediatr Urol 14(3):244.e241-244.e247. https://doi.org/10.1016/j.jpurol.2017.12.019
Bielza R, Balaguer C, Zambrana F, Arias E, Thuissard IJ, Lung A, Oñoro C, Pérez P, Andreu-Vázquez C, Neira M, Anguita N, Sáez C, de la Puente EMF (2022) Accuracy, feasibility and predictive ability of different frailty instruments in an acute geriatric setting. Eur Geriatr Med 13(4):827–835. https://doi.org/10.1007/s41999-022-00645-1
Mandrekar JN (2010) Receiver operating characteristic curve in diagnostic test assessment. J Thorac Oncol 5(9):1315–1316. https://doi.org/10.1097/JTO.0b013e3181ec173d
Zhang F, Chiu Y, Ensor J, Mohamed MO, Peat G, Mamas MA (2022) Elixhauser outperformed Charlson comorbidity index in prognostic value after ACS: insights from a national registry. J Clin Epidemiol 141:26–35. https://doi.org/10.1016/j.jclinepi.2021.08.025
Ondeck NT, Bohl DD, Bovonratwet P, McLynn RP, Cui JJ, Grauer JN (2018) Discriminative ability of Elixhauser’s comorbidity measure is superior to other comorbidity scores for inpatient adverse outcomes after total hip arthroplasty. J Arthroplasty 33(1):250–257. https://doi.org/10.1016/j.arth.2017.08.032
Austin SR, Wong YN, Uzzo RG, Beck JR, Egleston BL (2015) Why summary comorbidity measures such as the Charlson Comorbidity Index and Elixhauser Score Work. Med Care 53(9):e65-72. https://doi.org/10.1097/MLR.0b013e318297429c
Huynh MJ, Wang Y, Joshi M, Krasnow R, Yu AX, Mossanen M, Chung BI, Chang SL (2021) Patient factors predict complications after partial nephrectomy: validation and calibration of the Preoperative Risk Evaluation for Partial Nephrectomy (PREP) score. BJU Int 127(3):369–374. https://doi.org/10.1111/bju.15240
Dell’Oglio P, Tian Z, Leyh-Bannurah SR, Larcher A, Mazzone E, Moschini M, Trudeau V, Stabile A, Gallina A, Suardi N, Capitanio U, Mottrie A, Briganti A, Montorsi F, Rochefort CM, Karakiewicz PI (2019) Development of a new comorbidity assessment tool for specific prediction of perioperative mortality in contemporary patients treated with radical cystectomy. Ann Surg Oncol 26(6):1942–1949. https://doi.org/10.1245/s10434-019-07313-y
Funding
This study was supported by grant funding from the Capital Region Medical Research Institute (CRMRI). The CRMRI was not involved with the study design, research, analysis, data collection, interpretation of data, reviewing, or approval of the publication.
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study conception and design. Material preparation, data collection, and data analysis were performed by MKT, NM, PJF, CW, and BMI. The first draft of the manuscript was written by MKT, and all the authors commented on previous versions of the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical statement
This study was deemed exempt from Institutional Review Board review.
Ethical approval
This study uses the State Inpatient and State Ambulatory Surgery and Services Databases which only contains de-identified data. This study was deemed exempt from Institutional Review Board review.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tram, M.K., Moring, N., Feustel, P.J. et al. An evaluation of three validated comorbidity indices to predict short-term postoperative outcomes after prosthetic urologic surgery. Int Urol Nephrol 56, 847–854 (2024). https://doi.org/10.1007/s11255-023-03842-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03842-4