Abstract
Purpose
In recent years, increasing evidence has shown that sodium-glucose cotransporter 2 inhibitors (SGLT2i) drugs have potential renoprotective effects in patients with diabetes mellitus (DM). However, the renal protective effect of SGLT2i in non-diabetic nephropathy patients has not been extensively demonstrated. In this systematic review and meta-analysis, we aimed to evaluate the renal protective effect and safety of SGLT2i in non-diabetic nephropathy patients.
Methods
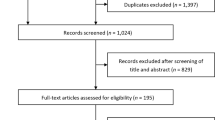
we searched for relevant clinically randomised controlled trials and analyzed the effects of SGLT2i on estimated glomerular filtration rate (eGFR), urinary albumin/creatinine ratio (UACR), and systolic blood pressure (SBP) and the incidence of adverse events in patients with non-diabetic nephropathy.
Results
We collated and analysed clinical data from six groups of patients with nondiabetic nephropathy. It was found that the SGLT2i significantly delayed the decline in eGFR [MD = 1.35 ml/min/1.73 m2, 95% CI 0.84, 1.86), P < 0.0001]. Furthermore, the SGLT2i significantly reduced UACR [MD = − 24.47% l, 95% CI (− 38.9, −10.04), P = 0.0009], and showed a greater decrease in SBP [MD = − 4.13 mmHg, 95% CI (− 7.49, − 0.77), P = 0.02]. There was no significant difference in the incidence of adverse reactions between dapagliflozin/empagliflozin and the control group [OR = 1.14, 95% CI (0.88, 1.47), P = 0.33].
Conclusion
This study shows that SGLT2i help to delay the progression of non-diabetic kidney disease. Therefore, SGLT2i may contribute to the general treatment of nondiabetic nephropathy.




Similar content being viewed by others
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Ferrannini E (2017) Sodium-glucose co-transporters and their inhibition: clinical physiology. Cell Metab 26(1):27–38. https://doi.org/10.1016/j.cmet.2017.04.011
Wanner C, Inzucchi SE, Lachin JM, Fitchett D, von Eynatten M, Mattheus M, Johansen OE, Woerle HJ, Broedl UC, Zinman B (2016) Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med 375(4):323–334. https://doi.org/10.1056/NEJMoa1515920
Perkovic V, Jardine MJ, Neal B, Bompoint S, Heerspink HJL, Charytan DM, Edwards R, Agarwal R, Bakris G, Bull S, Cannon CP, Capuano G, Chu PL, de Zeeuw D, Greene T, Levin A, Pollock C, Wheeler DC, Yavin Y, Zhang H, Zinman B, Meininger G, Brenner BM, Mahaffey KW (2019) Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med 380(24):2295–2306. https://doi.org/10.1056/NEJMoa1811744
Cooper ME, Inzucchi SE, Zinman B, Hantel S, von Eynatten M, Wanner C, Koitka-Weber A (2019) Glucose control and the effect of empagliflozin on kidney outcomes in type 2 diabetes: an analysis from the EMPA-REG OUTCOME trial. Am J Kidney Dis 74(5):713–715. https://doi.org/10.1053/j.ajkd.2019.03.432
Tamura K, Wakui H, Azushima K, Uneda K, Umemura S (2016) Circadian blood pressure rhythm as a possible key target of SGLT2 inhibitors used for the treatment of Type 2 diabetes. Hypert res 39(6):396–398. https://doi.org/10.1038/hr.2016.1
Heerspink HJL, Kosiborod M, Inzucchi SE, Cherney DZI (2018) Renoprotective effects of sodium-glucose cotransporter-2 inhibitors. Kidney Int 94(1):26–39. https://doi.org/10.1016/j.kint.2017.12.027
Vlasschaert C, Sidhu B, Silver SA (2021) Sodium/glucose cotransporter 2 inhibitors in chronic kidney disease and heart failure: ready for prime time in patients without diabetes. Curr Opin Nephrol Hypertens 30(3):361–368. https://doi.org/10.1097/mnh.0000000000000703
Teo YH, Teo YN, Syn NL, Kow CS, Yoong CSY, Tan BYQ, Yeo TC, Lee CH, Lin W, Sia CH (2021) Effects of sodium/glucose Cotransporter 2 (SGLT2) inhibitors on cardiovascular and metabolic outcomes in patients without diabetes mellitus: a systematic review and meta-analysis of randomized-controlled trials. J Amer Heart Assoc. 10(5):019463. https://doi.org/10.1161/jaha.120.019463
Cherney DZI, Dekkers CCJ, Barbour SJ, Cattran D, Abdul Gafor AH, Greasley PJ, Laverman GD, Lim SK, Di Tanna GL, Reich HN, Vervloet MG, Wong MG, Gansevoort RT, Heerspink HJL (2020) Effects of the SGLT2 inhibitor dapagliflozin on proteinuria in non-diabetic patients with chronic kidney disease (DIAMOND): a randomised, double-blind, crossover trial. Lancet Diabetes Endocrinol 8(7):582–593. https://doi.org/10.1016/s2213-8587(20)30162-5
Heerspink HJL, Stefansson BV, Chertow GM, Correa-Rotter R, Greene T, Hou FF, Lindberg M, McMurray J, Rossing P, Toto R, Langkilde AM, Wheeler DC (2020) Rationale and protocol of the dapagliflozin and prevention of adverse outcomes in chronic kidney disease (DAPA-CKD) randomized controlled trial. Nephrol dial transplant 35(2):274–282. https://doi.org/10.1093/ndt/gfz290
Antlanger M, Domenig O, Kaltenecker CC, Kovarik JJ, Rathkolb V, Müller MM, Schwaiger E, Hecking M, Poglitsch M, Säemann MD, Kopecky C (2022) Combined sodium glucose co-transporter-2 inhibitor and angiotensin-converting enzyme inhibition upregulates the renin-angiotensin system in chronic kidney disease with type 2 diabetes: Results of a randomized, double-blind, placebo-controlled exploratory trial. Diabetes Obes Metab 24(5):816–826. https://doi.org/10.1111/dom.14639
Herrington WG, Staplin N, Wanner C, Green JB, Hauske SJ, Emberson JR, Preiss D, Judge P, Mayne KJ, Ng SYA, Sammons E, Zhu D, Hill M, Stevens W, Wallendszus K, Brenner S, Cheung AK, Liu ZH, Li J, Hooi LS, Liu W, Kadowaki T, Nangaku M, Levin A, Cherney D, Maggioni AP, Pontremoli R, Deo R, Goto S, Rossello X, Tuttle KR (2023) Empagliflozin in patients with chronic kidney disease. N Engl J Med 388(2):117–127. https://doi.org/10.1056/NEJMoa2204233
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Revista espanola de cardiologia (English ed) 74(9):790–799. https://doi.org/10.1016/j.rec.2021.07.010
Wheeler DC, Toto RD, Stefánsson BV, Jongs N, Chertow GM, Greene T, Hou FF, McMurray JJV, Pecoits-Filho R, Correa-Rotter R, Rossing P, Sjöström CD, Umanath K, Langkilde AM, Heerspink HJL (2021) A pre-specified analysis of the DAPA-CKD trial demonstrates the effects of dapagliflozin on major adverse kidney events in patients with IgA nephropathy. Kidney Int 100(1):215–224. https://doi.org/10.1016/j.kint.2021.03.033
Heerspink HJL, Jongs N, Chertow GM, Langkilde AM, McMurray JJV, Correa-Rotter R, Rossing P, Sjöström CD, Stefansson BV, Toto RD, Wheeler DC, Greene T (2021) Effect of dapagliflozin on the rate of decline in kidney function in patients with chronic kidney disease with and without type 2 diabetes: a prespecified analysis from the DAPA-CKD trial. Lancet Diabetes Endocrinol 9(11):743–754. https://doi.org/10.1016/s2213-8587(21)00242-4
Wheeler DC, Jongs N, Stefansson BV, Chertow GM, Greene T, Hou FF, Langkilde AM, McMurray JJV, Rossing P, Nowicki M, Wittmann I, Correa-Rotter R, Sjöström CD, Toto RD, Heerspink HJL (2022) Safety and efficacy of dapagliflozin in patients with focal segmental glomerulosclerosis: a prespecified analysis of the dapagliflozin and prevention of adverse outcomes in chronic kidney disease (DAPA-CKD) trial. Nephrol dialy transplant 37(9):1647–1656. https://doi.org/10.1093/ndt/gfab335
Design, recruitment, and baseline characteristics of the EMPA-KIDNEY trial (2022). Nephrology, dialysis, transplantation 37 (7):1317–1329. Doi: https://doi.org/10.1093/ndt/gfac040
McGuire DK, Shih WJ, Cosentino F, Charbonnel B, Cherney DZI, Dagogo-Jack S, Pratley R, Greenberg M, Wang S, Huyck S, Gantz I, Terra SG, Masiukiewicz U, Cannon CP (2021) Association of SGLT2 Inhibitors With Cardiovascular and Kidney Outcomes in Patients With Type 2 Diabetes: A Meta-analysis. JAMA cardiology 6(2):148–158. https://doi.org/10.1001/jamacardio.2020.4511
Arnott C, Li Q, Kang A, Neuen BL, Bompoint S, Lam CSP, Rodgers A, Mahaffey KW, Cannon CP, Perkovic V, Jardine MJ, Neal B (2020) Sodium-glucose cotransporter 2 inhibition for the prevention of cardiovascular events in patients with type 2 diabetes mellitus: a systematic review and meta-analysis. J Amer Heart Assoc 9(3):014908. https://doi.org/10.1161/jaha.119.014908
Zelniker TA, Wiviott SD, Raz I, Im K, Goodrich EL, Bonaca MP, Mosenzon O, Kato ET, Cahn A, Furtado RHM, Bhatt DL, Leiter LA, McGuire DK, Wilding JPH, Sabatine MS (2019) SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet (London, England) 393(10166):31–39. https://doi.org/10.1016/s0140-6736(18)32590-x
Li LF, Ding LL, Zhan ZL, Qiu M (2021) Meta-analysis on the safety and cardiorenal efficacy of SGLT2 inhibitors in patients without T2DM. Front cardiovasc med. 8:690529. https://doi.org/10.3389/fcvm.2021.690529
Zelniker TA, Braunwald E (2020) Mechanisms of cardiorenal effects of sodium-glucose cotransporter 2 inhibitors: JACC state-of-the-art review. J Am Coll Cardiol 75(4):422–434. https://doi.org/10.1016/j.jacc.2019.11.031
Zhang Y, He D, Zhang W, Xing Y, Guo Y, Wang F, Jia J, Yan T, Liu Y, Lin S (2020) ACE inhibitor benefit to kidney and cardiovascular outcomes for patients with non-dialysis chronic kidney disease stages 3–5: A network meta-analysis of randomised clinical trials. Drugs 80(8):797–811. https://doi.org/10.1007/s40265-020-01290-3
Cheung AK, Rahman M, Reboussin DM, Craven TE, Greene T, Kimmel PL, Cushman WC, Hawfield AT, Johnson KC, Lewis CE, Oparil S, Rocco MV, Sink KM, Whelton PK, Wright JT Jr, Basile J, Beddhu S, Bhatt U, Chang TI, Chertow GM, Chonchol M, Freedman BI, Haley W, Ix JH, Katz LA, Killeen AA, Papademetriou V, Ricardo AC, Servilla K, Wall B, Wolfgram D, Yee J (2017) Effects of intensive BP control in CKD. J Am Soc Nephrol 28(9):2812–2823. https://doi.org/10.1681/asn.2017020148
De Nicola L, Gabbai FB, Garofalo C, Conte G, Minutolo R (2020) Nephroprotection by SGLT2 inhibition: back to the future? J clin med. https://doi.org/10.3390/jcm9072243
Funding
Hubei Provincial Department of Education Natural Science Research Project Fund, B2017024, Ping Zhu, Yichang Medical and Health Research Project Fund, A20-2-002, Ping Zhu.
Author information
Authors and Affiliations
Contributions
PZ and CM design. CM, XL, WL, YL, and FS conduct/data collection. CM and XL analysis. PZ and CM writing the manuscript. All authors contributed to the article and approved the submitted version.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ma, C., Li, X., Li, W. et al. The efficacy and safety of SGLT2 inhibitors in patients with non-diabetic chronic kidney disease: a systematic review and meta-analysis. Int Urol Nephrol 55, 3167–3174 (2023). https://doi.org/10.1007/s11255-023-03586-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03586-1