Abstract
Purpose
To compare the outcomes of mini-percutaneous nephrolithotomy (mPCNL) and retrograde intrarenal surgery (RIRS) in patients with renal stones sizing 2–3 cm.
Methods
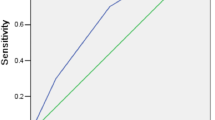
A total of 566 patients from 6 institutions who underwent mPCNL (n = 440) and RIRS (n = 126) procedures were enrolled in our study. The retrospective patient cohort was reviewed and compared. Binary logistic regression analysis was performed to determine factors predicting success in the RIRS group.
Results
The stone-free rates were 91.1 and 77% for the mPCNL and RIRS groups, respectively (p < 0.001). The auxiliary procedure rates were 4.5 and 39.7% in the mPCNL and RIRS groups, respectively (p < 0.001). Mean values of hemoglobin decrease, fluoroscopy time, and hospitalization time were significantly higher in the mPCNL group (p < 0.001). While the Clavien grade 1–2 complication rates were 10.9 and 34.1% (p < 0.001) in two groups, these values were 2.7 and 1.6% (p = 0.539), respectively, for Clavien grade 3–4 complication rates. Although three patients in the mPCNL group received blood transfusions, none of the patients in the RIRS groups were transfused. The stone location and stone density parameters were found to be the independent predictive factors for RIRS success.
Conclusions
mPCNL provided a higher stone-free rate, less need for the auxiliary procedure, and lower complication rates compared to RIRS in patients with 2–3 cm stones. Blood loss, radiation exposure, and a hospital stay of mPCNL can be significantly reduced with the RIRS technique in selected patients.
Similar content being viewed by others
Data availability
All datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
European Association of Urology. Urolithiasis 2021 [Available from: http://uroweb.org/guideline/urolithiasis/.
Ganpule AP, Bhattu AS, Desai M (2015) PCNL in the twenty-first century: role of Microperc, Miniperc, and Ultraminiperc. World J Urol 33(2):235–240
Sakr A, Salem E, Kamel M et al (2017) Minimally invasive percutaneous nephrolithotomy vs. standard PCNL for management of renal stones in the flank-free modified supine position: single-center experience. Urolithiasis 45(6):585–589
Li Y, He Q, Bao J et al (2020) Forecast and guiding role of using hounsfield unit in retrograde intrarenal surgery for the treatment of renal stone of 2–3 cm: a single center prospective study. Res Square. https://doi.org/10.21203/rs.3.rs-59924/v1
Zeng G, Zhu W, Li J et al (2015) The comparison of minimally invasive percutaneous nephrolithotomy and retrograde intrarenal surgery for stones larger than 2 cm in patients with a solitary kidney: a matched-pair analysis. World J Urol 33(8):1159–1164
El Shazly A, Taleb A, Ahmed A et al (2020) Mini-percutaneous nephrolithotomy (MPCNL) VS. Flexible ureterorenoscopy (RIRS) for renal stones> 2cm. Benha J Appl Sci 5((4 part (2))):1–5
Zhao Z, Sun H, Zeng T et al (2020) An easy risk stratification to recommend the optimal patients with 2–3 cm kidney stones to receive retrograde intrarenal surgery or mini-percutaneous nephrolithotomy. Urolithiasis 48(2):167–173
Erkoc M, Bozkurt M (2021) Comparison of mini-percutaneous nephrolithotomy and retrograde intrarenal surgery for renal pelvic stones of 2–3 cm. J Laparoendosc Adv Surg Tech 31(6):605–609
Zeng G, Cai C, Duan X et al (2021) Mini percutaneous nephrolithotomy is a noninferior modality to standard percutaneous nephrolithotomy for the management of 20–40 mm renal calculi: a multicenter randomized controlled trial. Eur Urol 79(1):114–121
Niwa N, Matsumoto K, Ohigashi T et al (2019) Clinical outcomes of retrograde intrarenal surgery as a primary treatment for staghorn calculi: a single-center experience. Clin Med Insights: Urol 12:1179561119854772
Sanguedolce F, Bozzini G, Chew B et al (2017) The evolving role of retrograde intrarenal surgery in the treatment of urolithiasis. Eur Urol Focus 3(1):46–55
Jiao B, Luo Z, Xu X et al (2019) Minimally invasive percutaneous nephrolithotomy versus retrograde intrarenal surgery in surgical management of upper urinary stones-A systematic review with meta-analysis. Int J Surg 71:1–11
De S, Autorino R, Kim FJ et al (2015) Percutaneous nephrolithotomy versus retrograde intrarenal surgery: a systematic review and meta-analysis. Eur Urol 67(1):125–137
Abd El Hamed AM, Elmoghazy H, Aldahshoury M et al (2017) Single session vs two sessions of flexible ureterosopy (FURS) for dusting of renal pelvic stones 2–3 cm in diameter: does stone size or hardness play a role in number of sessions to be applied?”. Turk J Urol 43(2):158
Resorlu B, Unsal A, Gulec H et al (2012) A new scoring system for predicting stone-free rate after retrograde intrarenal surgery: the “resorlu-unsal stone score.” Urology 80(3):512–518
Forbes CM, Rebullar KA, Teichman JM (2018) Comparison of flexible ureteroscopy damage rates for lower pole renal stones by laser fiber type. Lasers Surg Med 50(8):798–801
Becker B, Gross AJ, Netsch C (2019) Ho: YaG laser lithotripsy: recent innovations. Curr Opin Urol 29(2):103–107
Elhilali MM, Badaan S, Ibrahim A et al (2017) Use of the Moses technology to improve holmium laser lithotripsy outcomes: a preclinical study. J Endourol 31(6):598–604
Petzold R, Miernik A, Suarez-Ibarrola R (2021) In vitro dusting performance of a new solid-state thulium laser compared to holmium laser lithotripsy. J Endourol 35(2):221–225
Cracco CM, Scoffone CM (2020) Endoscopic combined intrarenal surgery (ECIRS)-Tips and tricks to improve outcomes: a systematic review. Tur J Urol 46(Suppl 1):S46
Lee JW, Park J, Lee SB et al (2015) Mini-percutaneous nephrolithotomy vs retrograde intrarenal surgery for renal stones larger than 10 mm: a prospective randomized controlled trial. Urology 86(5):873–877
Pan J, Chen Q, Xue W et al (2013) RIRS versus mPCNL for single renal stone of 2–3 cm: clinical outcome and cost-effective analysis in Chinese medical setting. Urolithiasis 41(1):73–78
Hein S, Schoenthaler M, Wilhelm K et al (2017) Ultralow radiation exposure during flexible ureteroscopy in patients with nephrolithiasis—How far can we go? Urology 108:34–39
Peng Y, Xu B, Zhang W et al (2015) Retrograde intrarenal surgery for the treatment of renal stones: is fluoroscopy-free technique achievable? Urolithiasis 43(3):265–270
Cheng F, Yu W, Zhang X et al (2010) Minimally invasive tract in percutaneous nephrolithotomy for renal stones. J Endourol 24(10):1579–1582
ElSheemy MS, Elmarakbi AA, Hytham M et al (2019) Mini vs standard percutaneous nephrolithotomy for renal stones: a comparative study. Urolithiasis 47(2):207–214
Kim HY, Lee KW, Lee DS (2020) Critical causes in severe bleeding requiring angioembolization after percutaneous nephrolithotomy. BMC Urol 20(1):1–7
Suh LK, Rothberg MB, Landman J et al (2010) Intrarenal pressures generated during deployment of various antiretropulsion devices in an ex vivo porcine model. J Endourol 24(7):1165–1168
Funding
No funding.
Author information
Authors and Affiliations
Contributions
MA: Ibis protocol/project development, data collection or management, data analysis, manuscript writing/editing; MB: data collection or management, data analysis, manuscript writing/editing; MIG: manuscript writing/editing; YY: data collection or management, manuscript writing/editing; MAK: manuscript writing/editing; AB: protocol/project development, manuscript writing/editing; SV: data collection or management, data analysis; ST: data collection or management, data analysis; TT: manuscript writing/editing; MCK: protocol/project development, data collection or management; MGS: data collection or management; RE: data collection or management, data analysis; SG: manuscript writing/editing; KS: protocol/project development, manuscript writing/editing. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no potential or financial conflicts of interest to declare.
Ethics approval
The study was approved by the Ankara University Faculty of Medicine Ethics Committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ibis, M.A., Gokce, M.I., Babayigit, M. et al. Could retrograde intrarenal surgery be a safe and effective alternative to mini-percutaneous nephrolithotomy ın the management of relatively large (20–30 mm) stones? A critical evaluation. Int Urol Nephrol 54, 2141–2148 (2022). https://doi.org/10.1007/s11255-022-03255-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-022-03255-9