Abstract
Introduction
The disease burden of bladder cancer is increasing worldwide; therefore, to deal with this situation, many studies on bladder cancer have been carried out extensively. Among these studies, the risk factors studies may provide a possible way to reduce the incidence of bladder cancer. Meta-analyses and original researches have confirmed that smoking is a risk factor of bladder cancer. However, the specific dose–response relationship between smoking and bladder cancer risk was still unclear. This meta-analysis addresses this research gap by summarizing the accumulated evidences, quantitatively.
Methods
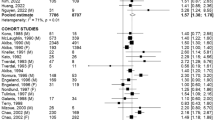
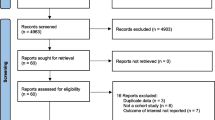
Relevant studies were obtained by searching PubMed, Embase and Web of Science database since inception until August 10, 2021, without restrictions. To obtain more comprehensive data, reference lists of identified articles were also browsed. Studies that reported risk estimates (relative risks (RR) or odds ratio (OR)) with 95% confidence intervals (CIs) focusing on the association between cigarette smoking and risk of bladder cancer were included in a dose–response meta-analysis.
Results
A non-linear dose–response relationship was confirmed between cigarette smoking and risk of bladder cancer on the basis of 8 cohorts and 44 case–control studies. The summary relative risk of developing bladder cancer for 1 more cigarettes/day (7 cohorts and 24 case–control studies) was 1.039 (95% CI 1.038–1.040, I2 = 0%), for 1 more pack-year (3 cohorts and 21 case–control studies) was 1.017(95% CI 1.016–1.019, I2 = 0%) and for 1 more year of exposure (16 case–control studies) was 1.021 (95% CI 1.020–1.023, I2 = 0%).
Conclusion
A positive non-linear dose–response relationship is confirmed between all smoking intensity, pack-years of smoking, smoking duration(years) and the risk of bladder cancer, but the plateau only occurred when smoking intensity reached 20 cigarettes/day. Further studies should report more detailed results, including those for subtypes of gender, age, region and be stratified by other risk factors to rule out residual confounding.







Similar content being viewed by others
References
Teoh JY, Huang J, Ko WY, Lok V, Choi P, Ng CF et al (2020) Global trends of bladder cancer incidence and mortality, and their associations with tobacco use and gross domestic product per capita. Eur Urol 78(6):893–906. https://doi.org/10.1016/j.eururo.2020.09.006
Siegel RL, Miller KD, Jemal A (2016) Cancer statistics, 2016. CA 66(1):7–30. https://doi.org/10.3322/caac.21332
Hartge P, Harvey EB, Linehan WM, Silverman DT, Sullivan JW, Hoover RN et al (1990) Unexplained excess risk of bladder cancer in men. J Natl Cancer Inst 82(20):1636–1640. https://doi.org/10.1093/jnci/82.20.1636
Vineis P, Frea B, Uberti E, Ghisetti V, Terracini B (1983) Bladder cancer and cigarette smoking in males: a case–control study. 69(1):17–22
Laaksonen MA, MacInnis RJ, Canfell K, Giles GG, Hull P, Shaw JE et al (2020) The future burden of kidney and bladder cancers preventable by behavior modification in Australia: a pooled cohort study. Int J Cancer 146(3):874–883. https://doi.org/10.1002/ijc.32420
Lao T, Gu W, Huang Q (2008) A meta-analysis on XRCC1 R399Q and R194W polymorphisms, smoking and bladder cancer risk. Mutagenesis 23(6):523–532. https://doi.org/10.1093/mutage/gen046
Wang M, Gu D, Zhang Z, Zhou J, Zhang Z (2009) XPD polymorphisms, cigarette smoking, and bladder cancer risk: a meta-analysis. J Toxicol Environ Health A 72(11–12):698–705. https://doi.org/10.1080/15287390902841029
van Osch FH, Jochems SH, van Schooten FJ, Bryan RT, Zeegers MP (2016) Quantified relations between exposure to tobacco smoking and bladder cancer risk: a meta-analysis of 89 observational studies. Int J Epidemiol 45(3):857–870. https://doi.org/10.1093/ije/dyw044
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ (Clin Res Ed) 339:b2535. https://doi.org/10.1136/bmj.b2535
Peterson J, Welch V, Losos M, Tugwell PJOOHRI (2011) The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses, vol 2, Issue 1. Ottawa Hospital Research Institute, Ottawa, pp 1–12
Greenland S, Longnecker MP (1992) Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol 135(11):1301–1309. https://doi.org/10.1093/oxfordjournals.aje.a116237
Orsini N, Bellocco R, Greenland S (2006) Generalized least squares for trend estimation of summarized dose–response data. Stata J 6(6):40–57
Dersimonian R, Nan L (1986) Meta-analysis in clinical trials. Control Clin Trials 7(3):177
Higgins JPT, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–58
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ (Clin Res Ed) 315(7109):629–634. https://doi.org/10.1136/bmj.315.7109.629
Alberg AJ, Kouzis A, Genkinger JM, Gallicchio L, Burke AE, Hoffman SC et al (2007) A prospective cohort study of bladder cancer risk in relation to active cigarette smoking and household exposure to secondhand cigarette smoke. Am J Epidemiol 165(6):660–666. https://doi.org/10.1093/aje/kwk047
Welty CJ, Wright JL, Hotaling JM, Bhatti P, Porter MP, White E (2014) Persistence of urothelial carcinoma of the bladder risk among former smokers: results from a contemporary, prospective cohort study. Urol Oncol 32(1):25. https://doi.org/10.1016/j.urolonc.2012.09.001
Sun CL, Yuan JM, Wang XL, Gao YT, Ross RK, Yu MC (2004) Dietary soy and increased risk of bladder cancer: a prospective cohort study of men in Shanghai. China Int J Cancer 112(2):319–323. https://doi.org/10.1002/ijc.20384
Inoue-Choi M, Hartge P, Liao LM, Caporaso N, Freedman ND (2018) Association between long-term low-intensity cigarette smoking and incidence of smoking-related cancer in the national institutes of health-AARP cohort. Int J Cancer 142(2):271–280. https://doi.org/10.1002/ijc.31059
Freedman ND, Abnet CC, Caporaso NE, Fraumeni JF, Murphy G, Hartge P et al (2016) Impact of changing US cigarette smoking patterns on incident cancer: risks of 20 smoking-related cancers among the women and men of the NIH-AARP cohort. Int J Epidemiol 45(3):846–856. https://doi.org/10.1093/ije/dyv175
Dugue PA, Brinkman MT, Hodge AM, Bassett JK, Bolton D, Longano A et al (2018) Dietary intake of nutrients involved in one-carbon metabolism and risk of urothelial cell carcinoma: a prospective cohort study. Int J Cancer 143(2):298–306. https://doi.org/10.1002/ijc.31319
Krabbe LM, Svatek RS, Shariat SF, Messing EM, Lotan Y (2014) Bladder cancer risk: use of PLCO and NLST to identify a suitable screening cohort. J Clin Oncol 32(15):65.e19–65.e25
Andreotti G, Karami S, Pfeiffer RM, Hurwitz L, Liao LM, Weinstein SJ et al (2014) LINE1 methylation levels associated with increased bladder cancer risk in pre-diagnostic blood DNA among US (PLCO) and European (ATBC) cohort study participants. Epigenetics 9(3):404–415. https://doi.org/10.4161/epi.27386
Band PR, Le ND, MacArthur AC, Fang R, Gallagher RP (2005) Identification of occupational cancer risks in british columbia: a population-based case–control study of 1129 cases of bladder cancer. J Occup Environ Med 47(8):854–858. https://doi.org/10.1097/01.jom.0000169094.77036.1d
Barbone F, Franceschi S, Talamini R, Bidoli E, La Vecchia C (1994) Occupation and bladder cancer in Pordenone (North-East Italy): a case–control study. Int J Epidemiol 23(1):58–65
Baris D, Karagas MR, Verrill C, Johnson A, Andrew AS, Marsit CJ et al (2009) A case–control study of smoking and bladder cancer risk: emergent patterns over time. J Natl Cancer Inst 101(22):1553–1561. https://doi.org/10.1093/jnci/djp361
Boada LD, Henriquez-Hernandez LA, Navarro P, Zumbado M, Almeida-Gonzalez M, Camacho M et al (2015) Exposure to polycyclic aromatic hydrocarbons (PAHs) and bladder cancer: evaluation from a gene-environment perspective in a hospital-based case-control study in the Canary Islands (Spain). Int J Occup Environ Health 21(1):23–30. https://doi.org/10.1179/2049396714Y.0000000085
Bozdogan ST, Erol B, Dursun A, Bozdogan G, Donmez I, Mungan NA et al (2015) The IL-1RN and IL-4 gene polymorphisms are potential genetic markers of susceptibility to bladder cancer: a case–control study. World J Urol 33(3):389–395. https://doi.org/10.1007/s00345-014-1323-4
Brinkman MT, Buntinx F, Kellen E, Dagnelie PC, Van Dongen M, Muls E et al (2011) Dietary intake of micronutrients and the risk of developing bladder cancer: results from the Belgian case–control study on bladder cancer risk. Cancer Causes Control 22(3):469–478. https://doi.org/10.1007/s10552-010-9718-z
Burch JD, Rohan TE, Howe GR, Risch HA, Hill GB, Steele R et al (1989) Risk of bladder cancer by source and type of tobacco exposure: a case-control study. Int J Cancer 44(4):622–628
Chu HY, Ma L, Wang ML, Shi DN, Qin C, Yuan L et al (2012) The polymorphisms of IL-4, IL-4R and IL-13 genes and bladder cancer risk in a Chinese population: a case–control study. Mol Biol Rep 39(5):5349–5357. https://doi.org/10.1007/s11033-011-1334-9
Clavel J, Cordier S, Boccon-Gibod L, Hemon D (1989) Tobacco and bladder cancer in males: increased risk for inhalers and smokers of black tobacco. Int J Cancer 44(4):605–610. https://doi.org/10.1002/ijc.2910440408
Colt JS, Baris D, Stewart P, Schned AR, Heaney JA, Mott LA et al (2004) Occupation and bladder cancer risk in a population-based case–control study in New Hampshire. Cancer Causes Control 15(8):759–769. https://doi.org/10.1023/B:CACO.0000043426.28741.a2
Cordier S, Clavel J, Limasset JC, Boccon-Gibod L, Le Moual N, Mandereau L et al (1993) Occupational risks of bladder cancer in France: a multicentre case–control study. Int J Epidemiol 22(3):403–411
Covolo L, Placidi D, Gelatti U, Carta A, Di Carlo AS, Lodetti P et al (2008) Bladder cancer, GSTs, NAT1, NAT2, SULT1A1, XRCC1, XRCC3, XPD genetic polymorphisms and coffee consumption: a case–control study. Eur J Epidemiol 23(5):355–362. https://doi.org/10.1007/s10654-008-9238-2
Dai QS, He HC, Cai C, Chen JH, Han ZD, Qin GQ et al (2011) Multicenter case–control study of the relationship between smoking and bladder cancer in China. Natl Med J China 91(34):2407–2410. https://doi.org/10.3760/cma.j.issn.0376-2491.2011.34.008
De Stefani E, Correa P, Fierro L, Fontham E, Chen V, Zavala D (1991) Black tobacco, maté, and bladder cancer. A case-control study from uruguay. Cancer 67(2):536–540. https://doi.org/10.1002/1097-0142(19910115)67:2%3c536::aid-cncr2820670236%3e3.0.co;2-8
Fortuny J, Kogevinas M, Chang-Claude J, Gonzalez CA, Hours M, Jockel KH et al (1999) Tobacco, occupation and non-transitional-cell carcinoma of the bladder: an international case–control study. Int J Cancer 80(1):44–46. https://doi.org/10.1002/(SICI)1097-0215(19990105)80:1%3c44::AID-IJC9%3e3.0.CO;2-8
Freedman DM, Cantor KP, Lee NL, Chen LS, Lei HH, Ruhl CE et al (1997) Bladder cancer and drinking water: a population-based case–control study in washington county, maryland (United States). Cancer Causes Control 8(5):738–744. https://doi.org/10.1023/A:1018431421567
Gaertner RR, Trpeski L, Johnson KC (2004) A case–control study of occupational risk factors for bladder cancer in Canada. Cancer Causes Control 15(10):1007–1019. https://doi.org/10.1007/s10552-004-1448-7
Geoffroy-Perez A, Cordier S (2001) Fluid consumption and the risk of bladder cancer: results of a multicenter case–control study. Int J Cancer 93(6):880–887
Hartge P, Silverman D, Hoover R (1987) Changing cigarette habits and bladder cancer risk: a case–control study. J Natl Cancer Inst 78(6):1119–1125
Hemelt M, Hu Z, Zhong Z, Xie LP, Wong YC, Tam PC et al (2010) Fluid intake and the risk of bladder cancer: results from the South and East China case–control study on bladder cancer. Int J Cancer 127(3):638–645. https://doi.org/10.1002/ijc.25084
Hours M, Dananche B, Fevotte J, Bergeret A, Ayzac L, Cardis E et al (1994) Bladder cancer and occupational exposures. Scand J Work Environ Health 20(5):322–330. https://doi.org/10.5271/sjweh.1390
Jensen OM, Knudsen JB, McLaughlin JK, Sorensen BL (1988) The Copenhagen case–control study of renal pelvis and ureter cancer: role of smoking and occupational exposures. Int J Cancer 41(4):557–561
Jensen OM, Wahrendorf J, Blettner M, Knudsen JB, Sørensen BL (1987) The Copenhagen case–control study of bladder cancer: role of smoking in invasive and non-invasive bladder tumours. J Epidemiol Community Health 41(1):30–36. https://doi.org/10.1136/jech.41.1.30
Koivusalo M, Hakulinen T, Vartiainen T, Pukkala E, Jaakkola JJ, Tuomisto J (1998) Drinking water mutagenicity and urinary tract cancers: a population-based case–control study in Finland. Am J Epidemiol 148(7):704–712. https://doi.org/10.1093/aje/148.7.704
Kunze E, Chang-Claude J, Frentzel-Beyme R (1992) Life style and occupational risk factors for bladder cancer in Germany: a case–control study. Cancer 69(7):1776–1790
Liang D, Lin J, Grossman HB, Ma J, Wei B, Dinney CP et al (2008) Plasma vitamins E and A and risk of bladder cancer: a case–control analysis. Cancer Causes Control 19(9):981–992. https://doi.org/10.1007/s10552-008-9165-2
López-Abente G, González CA, Errezola M, Escolar A, Izarzugaza I, Nebot M et al (1991) Tobacco smoke inhalation pattern, tobacco type, and bladder cancer in Spain. Am J Epidemiol 134(8):830–839. https://doi.org/10.1093/oxfordjournals.aje.a116158
Ma L, Chu HY, Wang ML, Shi DN, Zhong DY, Li P et al (2012) hOGG1 Ser326Cys polymorphism is associated with risk of bladder cancer in a Chinese population: a case-control study. Cancer Sci 103(7):1215–1220. https://doi.org/10.1111/j.1349-7006.2012.02290.x
Meliker JR, Slotnick MJ, AvRuskin GA, Schottenfeld D, Jacquez GM, Wilson ML et al (2010) Lifetime exposure to arsenic in drinking water and bladder cancer: a population-based case–control study in Michigan, USA. Cancer Causes Control 21(5):745–757. https://doi.org/10.1007/s10552-010-9503-z
Momas I, Daures JP, Festy B, Bontoux J, Gremy F (1994) Bladder cancer and black tobacco cigarette smoking. Some results from a French case–control study. Eur J Epidemiol 10(5):599–604
Pesch B, Gawrych K, Rabstein S, Weiss T, Casjens S, Rihs HP et al (2013) N-acetyltransferase 2 phenotype, occupation, and bladder cancer risk: results from the EPIC cohort. Cancer Epidemiol Biomark Prev 22(11):2055–2065. https://doi.org/10.1158/1055-9965.EPI-13-0119-T
Porru S, Pavanello S, Carta A, Arici C, Simeone C, Izzotti A et al (2014) Complex relationships between occupation, environment, DNA adducts, genetic polymorphisms and bladder cancer in a case-control study using a structural equation modeling. PLoS One. https://doi.org/10.1371/journal.pone.0094566
Rebelakos A, Trichopoulos D, Tzonou A, Zavitsanos X, Velonakis E, Trichopoulos A (1985) Tobacco smoking, coffee drinking, and occupation as risk factors for bladder cancer in Greece. J Natl Cancer Inst 75(3):455–461
Shivappa N, Hebert JR, Rosato V, Rossi M, Libra M, Montella M et al (2017) Dietary inflammatory index and risk of bladder cancer in a large Italian case–control study. Urology 100:84–89. https://doi.org/10.1016/j.urology.2016.09.026
Sorahan T, Lancashire RJ, Sole G (1994) Urothelial cancer and cigarette-smoking—findings from a regional case–controlled study. Br J Urol 74(6):753–756. https://doi.org/10.1111/j.1464-410X.1994.tb07120.x
Stern MC, Van Den Berg D, Yuan JM, Conti DV, Gago-Dominguez M, Pike MC et al (2009) Sequence variant on 3q28 and urinary bladder cancer risk: findings from the Los Angeles-Shanghai bladder case–control study. Cancer Epidemiol Biomark Prev 18(11):3057–3061. https://doi.org/10.1158/1055-9965.EPI-09-0492
Wakai K, Takashi M, Okamura K, Yuba H, Suzuki K, Murase T et al (2000) Foods and nutrients in relation to bladder cancer risk: a case–control study in Aichi prefecture. Central Jpn Nutr Cancer 38(1):13–22. https://doi.org/10.1207/s15327914nc381_3
Wallace K, Kelsey KT, Schned A, Morris JS, Andrew AS, Karagas MR (2009) Selenium and risk of bladder cancer: a population-based case–control study. Cancer Prev Res 2(1):70–73. https://doi.org/10.1158/1940-6207.CAPR-08-0046
Wu CC, Huang YK, Huang CY, Shiue HS, Pu YS, Su CT et al (2018) Polymorphisms of TNF-alpha-308 G/A and IL-8–251 T/A genes associated with urothelial carcinoma: a case–control study. BioMed Res Int. https://doi.org/10.1155/2018/3148137
Yu Y, Hu J, Wang PP, Zou Y, Qi Y, Zhao P et al (1997) Risk factors for bladder cancer: a case–control study in Northeast China. Eur J Cancer Prev 6(4):363–369. https://doi.org/10.1097/00008469-199708000-00008
Zaitsu M, Nakamura F, Toyokawa S, Tonooka A, Takeuchi T, Homma Y et al (2016) Risk of alcohol consumption in bladder cancer: case–control study from a nationwide inpatient database in Japan. Tohoku J Exp Med 239(1):9–15. https://doi.org/10.1620/tjem.239.9
Zheng YL, Amr S, Saleh DA, Dash C, Ezzat S, Mikhail NN et al (2012) Urinary bladder cancer risk factors in Egypt: a multicenter case–control study. Cancer Epidemiol Biomark Prev 21(3):537–546. https://doi.org/10.1158/1055-9965.EPI-11-0589
Benowitz NL, Perez-Stable EJ, Herrera B, Jacob P 3rd (2002) Slower metabolism and reduced intake of nicotine from cigarette smoking in Chinese-Americans. J Natl Cancer Inst 94(2):108–115. https://doi.org/10.1093/jnci/94.2.108
Geng H, Zhao L, Liang Z, Zhang Z, Xie D, Bi L et al (2017) Cigarette smoke extract-induced proliferation of normal human urothelial cells via the MAPK/AP-1 pathway. Oncol Lett 13(1):469–475. https://doi.org/10.3892/ol.2016.5407
Yuge K, Kikuchi E, Hagiwara M, Yasumizu Y, Tanaka N, Kosaka T et al (2015) Nicotine induces tumor growth and chemoresistance through activation of the PI3K/Akt/mTOR pathway in bladder cancer. Mol Cancer Ther 14(9):2112–2120. https://doi.org/10.1158/1535-7163.mct-15-0140
Lee HW, Wang HT, Weng MW, Chin C, Huang W, Lepor H et al (2015) Cigarette side-stream smoke lung and bladder carcinogenesis: inducing mutagenic acrolein-DNA adducts, inhibiting DNA repair and enhancing anchorage-independent-growth cell transformation. Oncotarget 6(32):33226–33236. https://doi.org/10.18632/oncotarget.5429
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest between authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhao, X., Wang, y. & Liang, C. Cigarette smoking and risk of bladder cancer: a dose–response meta-analysis. Int Urol Nephrol 54, 1169–1185 (2022). https://doi.org/10.1007/s11255-022-03173-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-022-03173-w