Abstract
Background
There is limited understanding of aetiological factors of and treatment options for restless leg syndrome (RLS) in patients with chronic kidney disease (CKD). This study aimed to estimate the prevalence of RLS in CKD patients and identify factors that may contribute to RLS.
Methods
A questionnaire-based cross-sectional study of patients with CKD stage 4 (CKD 4), pre-dialysis stage 5 (CKD-5ND) and haemodialysis-dependent stage 5 (CKD-5D) was conducted. Eligible patients were enrolled from the local dialysis units and renal clinics. The International RLS Study Group rating scale was used to establish the diagnosis of RLS and quantify its severity.
Results
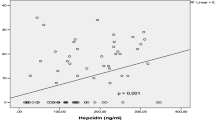
212 patients with CKD 4 (n = 92), CKD-5ND (n = 14) and CKD-5D (n = 106) were included. The overall prevalence of RLS was 32.1%. Women had a significantly higher odds of having RLS despite adjustment for age, diabetes, cardiovascular disease and whether patients were on dialysis (odds ratio 2.8 [95% confidence intervals 1.5–5.2]). In pre-dialysis groups, patients with RLS had significantly higher serum ferritin (323.9 [SD 338.1] vs 177.5 [SD 178.5] µg/L, p = 0.020) compared to non-RLS patients. In dialysis patients (CKD-5D), those with RLS had significantly higher total white cell (8.0 [SD 3.5] vs 6.8 [SD 1.9] × 109/L, p = 0.026) and neutrophil (6.4 [SD 3.9] vs 4.6 [SD1.7] × 109/L, p = 0.002) counts compared to patients without RLS.
Conclusion
RLS remains a significant problem in patients with CKD and may be related to underlying inflammation. Targeting this pathway may be useful. Prevalence of RLS, diagnosed using validated measures, is higher than previous reports.
Trial registration
N/A (the current study is not a trial).




Similar content being viewed by others
Availability of data and material
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BMI:
-
Body mass index
- BP:
-
Blood pressure
- CI:
-
Confidence interval
- CKD:
-
Chronic kidney disease
- CKD-EPI:
-
Chronic Kidney Disease Epidemiology Collaboration
- CKD-5ND:
-
Chronic Kidney Disease stage 5 non-dialysis-dependent
- CKD-5D:
-
Chronic Kidney Disease stage 5 dialysis-dependent
- CVD:
-
Cardiovascular disease
- DM:
-
Diabetes mellitus
- HD:
-
Haemodialysis/haemodiafiltration
- IQR:
-
Interquartile range
- IRLSSG:
-
International Restless Legs Syndrome Study Group
- NICE:
-
National Institute of Health and Care Excellence
- RLS:
-
Restless leg syndrome
- SD:
-
Standard deviation
- UK:
-
United Kingdom
- USA:
-
United States of America
References
Allen RP, Picchietti D, Hening WA, Trenkwalder C, Walters AS, Montplaisi J et al (2003) Restless legs syndrome: diagnostic criteria, special considerations, and epidemiology. A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Med 4:101–119
Kennedy C, Ryan SA, Kane T, Costello RW, Conlon PJ (2018) The impact of change of renal replacement therapy modality on sleep quality in patients with end-stage renal disease: a systematic review and meta-analysis. J Nephrol 31:61–70
Sinclair PM (2018) Interventions for chronic kidney disease-associated restless legs syndrome. Int J Evid Based Healthc 16:182–184
Novak M, Winkelman JW, Unruh M (2015) restless legs syndrome in patients with chronic kidney disease. Semin Nephrol 35:347–358
Mucsi I, Molnar MZ, Ambrus C, Szeifert L, Kovacs AZ, Zoller R et al (2005) Restless legs syndrome, insomnia and quality of life in patients on maintenance dialysis. Nephrol Dial Transplant 20:571–577
DeFerio JJ, Govindarajulu U, Brar A, Cukor D, Lee KG, Salifu MO (2017) Association of restless legs syndrome and mortality in end-stage renal disease: an analysis of the United States Renal Data System (USRDS). BMC Nephrol 18:258
Molnar MZ, Lu JL, Kalantar-Zadeh K, Kovesdy CP (2016) Association of incident restless legs syndrome with outcomes in a large cohort of US veterans. J Sleep Res 25:47–56
Winkelman JW, Chertow GM, Lazarus JM (1996) Restless legs syndrome in end-stage renal disease. Am J Kidney Dis 28:372–378
Zhang J, Wang C, Gong W, Peng H, Tang Y, Li CC et al (2014) Association between sleep quality and cardiovascular damage in pre-dialysis patients with chronic kidney disease. BMC Nephrol 15:131
Pierratos A, Hanly PJ (2011) Sleep disorders over the full range of chronic kidney disease. Blood Purif 31:146–150
Anand S, Johansen KL, Grimes B, Kaysen GA, Dalrymple LS, Kutner NG et al (2013) Physical activity and self-reported symptoms of insomnia, restless legs syndrome, and depression: the comprehensive dialysis study. Hemodial Int 17:50–58
Giannaki CD, Sakkas GK, Karatzaferi C, Hadjigeorgiou GM, Lavdas E, Liakopoulos V et al (2011) Evidence of increased muscle atrophy and impaired quality of life parameters in patients with uremic restless legs syndrome. PLoS ONE 6:e25180
Mao S, Shen H, Huang S, Zhang A (2014) Restless legs syndrome in dialysis patients: a meta-analysis. Sleep Med 15:1532–1538
Neves PD, Graciolli FG, Oliveira IB, Bridi RA, Moyses RM, Elias RM (2017) Effect of mineral and bone metabolism on restless legs syndrome in hemodialysis patients. J Clin Sleep Med 13:89–94
Zadeh Saraji N, Hami M, Boostani R, Mojahedi MJ (2017) Restless leg syndrome in chronic hemodialysis patients in Mashhad hemodialysis centers. J Renal Inj Prev 6:137–141
Gigli GL, Adorati M, Dolso P, Piani A, Valente M, Brotini S et al (2004) Restless legs syndrome in end-stage renal disease. Sleep Med 5:309–315
Kim JM, Kwon HM, Lim CS, Kim YS, Lee SJ, Nam H (2008) Restless legs syndrome in patients on hemodialysis: symptom severity and risk factors. J Clin Neurol 4:153–157
Murtagh FE, Addington-Hall J, Higginson IJ (2007) The prevalence of symptoms in end-stage renal disease: a systematic review. Adv Chronic Kidney Dis 14:82–99
Hazara AM, Bhandari S (2019) Can incremental haemodialysis reduce early mortality rates in patients starting maintenance haemodialysis? Curr Opin Nephrol Hypertens 28:641–647
Walters AS, LeBrocq C, Dhar A, Hening W, Rosen R, Allen RP et al (2003) Validation of the International Restless Legs Syndrome Study Group rating scale for restless legs syndrome. Sleep Med 4:121–132
NICE Guideline (2018) Chronic kidney disease in adults: assessment and management (CG182). National Institute of Health and Care Excellence, London (Online)
Lin Z, Zhao C, Luo Q, Xia X, Yu X, Huang F (2016) Prevalence of restless legs syndrome in chronic kidney disease: a systematic review and meta-analysis of observational studies. Ren Fail 38:1335–1346
Kutner NG, Bliwise DL (2002) Restless legs complaint in African–American and Caucasian hemodialysis patients. Sleep Med 3:497–500
Stefanidis I, Vainas A, Dardiotis E, Giannaki CD, Gourli P, Papadopoulou D et al (2013) Restless legs syndrome in hemodialysis patients: an epidemiologic survey in Greece. Sleep Med 14:1381–1386
Lin XW, Zhang JF, Qiu MY, Ni LY, Yu HL, Kuo SH et al (2019) Restless legs syndrome in end stage renal disease patients undergoing hemodialysis. BMC Neurol 19:47
Rohani M, Aghaei M, Jenabi A, Yazdanfar S, Mousavi D, Miri S (2015) Restless legs syndrome in hemodialysis patients in Iran. Neurol Sci 36:723–727
Weinstock LB, Walters AS, Paueksakon P (2012) Restless legs syndrome—theoretical roles of inflammatory and immune mechanisms. Sleep Med Rev 16:341–354
Nuhu F, Bhandari S (2018) Oxidative stress and cardiovascular complications in chronic kidney disease, the impact of anaemia. Pharmaceuticals (Basel) 11:103
La Manna G, Pizza F, Persici E, Baraldi O, Comai G, Cappuccilli ML et al (2011) Restless legs syndrome enhances cardiovascular risk and mortality in patients with end-stage kidney disease undergoing long-term haemodialysis treatment. Nephrol Dial Transplant 26:1976–1983
Seeman MV (2020) Why are women prone to restless legs syndrome? Int J Environ Res Public Health 17:368
Trenkwalder C, Allen R, Hogl B, Paulus W, Winkelmann J (2016) Restless legs syndrome associated with major diseases: a systematic review and new concept. Neurology 86:1336–1343
Hazara AM, Bhandari S (2015) Intravenous iron administration is associated with reduced platelet counts in patients with chronic kidney disease. J Clin Pharm Ther 40:20–23
Gopaluni S, Sherif M, Ahmadouk NA (2016) Interventions for chronic kidney disease-associated restless legs syndrome. Cochrane Database Syst Rev 11:CD010690
Happe S, Sauter C, Klosch G, Saletu B, Zeitlhofer J (2003) Gabapentin versus ropinirole in the treatment of idiopathic restless legs syndrome. Neuropsychobiology 48:82–86
Oertel W, Trenkwalder C, Benes H, Ferini-Strambi L, Hogl B, Poewe W et al (2011) Long-term safety and efficacy of rotigotine transdermal patch for moderate-to-severe idiopathic restless legs syndrome: a 5-year open-label extension study. Lancet Neurol 10:710–720
Acknowledgements
The authors would like to thank Mr. Archie Lamplugh and Ms. Tracy Cathcart for their help with data collection during this study.
Funding
None.
Author information
Authors and Affiliations
Contributions
AB and SB conceived the study. AB and AMH, conducted the analysis and wrote the first draft. AMH and SB completed the final draft. All authors approve the final draft.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests. The results presented in this paper have not been published previously in whole or part, except in abstract format.
Ethics approval and consent to participate
The study received favourable ethical approval from the South Central—Oxford C Research Ethics Committee reference 18/SC/0476; and IRAS Reference 251719.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Brzuszek, A., Hazara, A.M. & Bhandari, S. The prevalence and potential aetiological factors associated with restless legs syndrome in patients with chronic kidney disease: a cross-sectional study. Int Urol Nephrol 54, 2599–2607 (2022). https://doi.org/10.1007/s11255-022-03166-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-022-03166-9