Abstract
Objective
The present study aims to assess the relationship between red blood cell distribution width (RDW) and clinically significant prostate cancer (csPCa).
Methods
A total of 458 patients with prostate-specific antigen (PSA) ≤ 10 ng/ml, who subsequently underwent 11-core transperineal template-guided prostate biopsy from June 15, 2015 to November 24, 2020, were included in the present study. Receiver-operating characteristic (ROC)-derived area under the curve analysis was performed to evaluate the predictive accuracy. In addition, univariate and multivariate logistic regression analysis was carried out to determine the association between RDW and csPCa detection.
Results
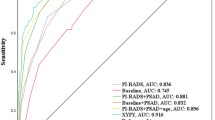
A total of 89 patients were diagnosed with csPCa, and these patients presented with higher median RDW. The optimal RDW cut-off was set at 12.35%, which gained the maximal Yuden’s index. In addition to csPCa, RDW demonstrated a positive correlation with age (r = 0.210, P < 0.001). It was observed that RDW was independent of prostate-specific antigen density for csPCa detection. Compared with the low-RDW group, patients in the high-RDW group had a 1.586-fold increased risk of being diagnosed with csPCa (OR = 2.586, P = 0.007). In the ROC analysis, the accuracy level increased by 3.1% for the prediction of csPCa, when RDW was added to the multivariate logistic model.
Conclusion
A high-RDW value is an independent risk factor for csPCa detection. However, more large-scale studies are needed to confirm these findings. If validated, RDW can become an inexpensive, non-invasive, and convenient indicator for csPCa prediction.



Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A (2020) Cancer statistics. CA Cancer J Clin 70(1):7–30. https://doi.org/10.3322/caac.21590
Stabile A, Giganti F, Rosenkrantz AB, Taneja SS, Villeirs G, Gill IS, Allen C, Emberton M, Moore CM, Kasivisvanathan V (2020) Multiparametric MRI for prostate cancer diagnosis: current status and future directions. Nat Rev Urol 17(1):41–61. https://doi.org/10.1038/s41585-019-0212-4
Fujita K, Nonomura N (2018) Urinary biomarkers of prostate cancer. Int J Urol 25(9):770–779. https://doi.org/10.1111/iju.13734
Fukuokaya W, Kimura T, Onuma H, Mori K, Honda M, Inaba H, Sasaki H, Shimomura T, Miki K, Egawa S (2019) Red cell distribution width predicts prostate-specific antigen response and survival of patients with castration-resistant prostate cancer treated with androgen receptor axis-targeted agents. Clin Genitourin Cancer 17(3):223–230. https://doi.org/10.1016/j.clgc.2019.04.010
Machidori A, Shiota M, Kobayashi S, Matsumoto T, Monji K, Kashiwagi E, Takeuchi A, Takahashi R, Inokuchi J, Eto M (2020) Prognostic significance of complete blood count parameters in castration-resistant prostate cancer patients treated with androgen receptor pathway inhibitors. Urol Oncol. https://doi.org/10.1016/j.urolonc.2020.09.036
Salvagno GL, Sanchis-Gomar F, Picanza A, Lippi G (2015) Red blood cell distribution width: a simple parameter with multiple clinical applications. Crit Rev Clin Lab Sci 52(2):86–105. https://doi.org/10.3109/10408363.2014.992064
Hou GD, Zheng Y, Zheng WX, Gao M, Zhang L, Hou NN, Yuan JR, Wei D, Ju DE, Dun XL, Wang FL, Yuan JL (2020) A novel nomogram predicting the risk of positive biopsy for patients in the diagnostic gray area of prostate cancer. Sci Rep 10(1):17675. https://doi.org/10.1038/s41598-020-74703-8
Song GG, Lee YH (2020) Red cell distribution width, platelet-to-lymphocyte ratio, and mean platelet volume in ankylosing spondylitis and their correlations with inflammation: A meta-analysis. Mod Rheumatol 30(5):894–899. https://doi.org/10.1080/14397595.2019.1645373
Sun Z, Ju Y, Han F, Sun X, Wang F (2018) Clinical implications of pretreatment inflammatory biomarkers as independent prognostic indicators in prostate cancer. J Clin Lab Anal. https://doi.org/10.1002/jcla.22277
Tewari AK, Stockert JA, Yadav SS, Yadav KK, Khan I (2018) Inflammation and prostate cancer. Adv Exp Med Biol 1095:41–65. https://doi.org/10.1007/978-3-319-95693-0_3
Rani A, Dasgupta P, Murphy JJ (2019) Prostate cancer: the role of inflammation and chemokines. Am J Pathol 189(11):2119–2137. https://doi.org/10.1016/j.ajpath.2019.07.007
Huang TB, Yan Y, Guo ZF, Zhang XL, Liu H, Geng J, Yao XD, Zheng JH (2014) Aspirin use and the risk of prostate cancer: a meta-analysis of 24 epidemiologic studies. Int Urol Nephrol 46(9):1715–1728. https://doi.org/10.1007/s11255-014-0703-4
Oh JJ, Kwon O, Lee JK, Byun SS, Lee SE, Lee S, Hong SK (2016) Association of the neutrophil-to-lymphocyte ratio and prostate cancer detection rates in patients via contemporary multi-core prostate biopsy. Asian J Androl 18(6):937–941. https://doi.org/10.4103/1008-682X.164198
Guan Y, Xiong H, Feng Y, Liao G, Tong T, Pang J (2020) Revealing the prognostic landscape of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in metastatic castration-resistant prostate cancer patients treated with abiraterone or enzalutamide: a meta-analysis. Prostate Cancer Prostatic Dis 23(2):220–231. https://doi.org/10.1038/s41391-020-0209-3
Murray NP, Fuentealba C, Salazar A, Reyes E (2020) Platelet-to-lymphocyte ratio and systemic immune-inflammation index versus circulating prostate cells to predict significant prostate cancer at first biopsy. Turk J Urol 46(2):115–122. https://doi.org/10.5152/tud.2020.19203
Kamali K, Ashrafi M, Shadpour P, Ameli M, Khayyamfar A, Abolhasani M, Azizpoor A (2018) The role of blood neutrophil count and the neutrophil-to-lymphocyte ratio as a predictive factor for prostate biopsy results. Urologia 85(4):158–162. https://doi.org/10.1177/0391560318766822
Albayrak S, Zengin K, Tanik S, Bakirtas H, Imamoglu A, Gurdal M (2014) Red cell distribution width as a predictor of prostate cancer progression. Asian Pac J Cancer Prev 15(18):7781–7784. https://doi.org/10.7314/apjcp.2014.15.18.7781
Yan Z, Fan Y, Meng Z, Huang C, Liu M, Zhang Q, Song K, Jia Q (2019) The relationship between red blood cell distribution width and metabolic syndrome in elderly Chinese: a cross-sectional study. Lipids Health Dis 18(1):34. https://doi.org/10.1186/s12944-019-0978-7
Yin Y, Ye S, Wang H, Li B, Wang A, Yan W, Dou J, Mu Y (2018) Red blood cell distribution width and the risk of being in poor glycemic control among patients with established type 2 diabetes. Ther Clin Risk Manag 14:265–273. https://doi.org/10.2147/TCRM.S155753
Nada AM (2015) Red cell distribution width in type 2 diabetic patients. Diabetes Metab Syndr Obes Targets Ther 8:525–533. https://doi.org/10.2147/DMSO.S85318
Acknowledgements
Tian-bao Huang was responsible for the initial plan, data collection and statistical analysis, and for conducting the study. Liang-Yong Zhu contributed to the data collection. Tian-bao Huang and Guang-chen Zhou contributed to the data interpretation and manuscript drafting. Xue-fei Ding is the guarantor for the manuscript, and has full responsibility for the study. This work was supported by Yangzhou Science and Technology Plan Project (YZ2019053). We thank Lu Feng for the manuscript revision.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Author’s disclosures of potential conflicts of interest: none for all authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, Tb., Zhu, Ly., Zhou, Gc. et al. Pre-treatment red blood cell distribution width as a predictor of clinically significant prostate cancer. Int Urol Nephrol 53, 1765–1771 (2021). https://doi.org/10.1007/s11255-021-02900-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-021-02900-z