Abstract
Aging is one of the main risk factors for venous thromboembolism (VTE). Changes in prevention, diagnosis, and treatment strategies for this condition in recent years require an analysis of its rates in health services. The objective of this study was to analyze a temporal trend of hospitalizations for VTE in Brazilian older adults. This ecological time series study used data from the Hospital Information System (HIS) on VTE hospitalizations from 2010 to 2020, selecting admissions with the main diagnosis of pulmonary thromboembolism (PTE) (I.26.0, I.26.9) and deep vein thrombosis (DVT) (I.80.0, I80.1, I80.2, I80.3, I80.8, I80.9). Hospitalization rates were calculated for each year and the Prais–Winsten. In Brazil, the trend of hospitalizations for VTE decreased, with an annual percentage change of – 40.71 (confidence interval [CI] – 50.46; − 29.04). DVT decreased, with an annual percentage change of − 43.14 (95% confidence interval [CI] − 51.36; − 33.54). All Brazilian regions showed a downward trend in hospitalizations for VTE and DVT, except for the Northeast region, which remained stable. Conversely, the trend of hospitalizations for PTE showed an upward in Brazil, with an annual percentage change of 4.33 (95% CI 1.26; 7.48). An upward trend was observed in hospitalizations for PTE in the Northeast region, and a stationary trend was observed in the other regions. The results showed a downward trend in hospitalization rates for DVT and an upward trend for PTE. The study indicates regional differences in rates and trends.

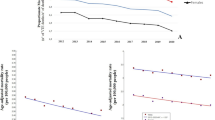
Source: SIH/SUS

Source: SIH/SUS

Source: SIH/SUS
Similar content being viewed by others
References
Ageno W, Haas S, Weitz JI, Goldhaber SZ, Turpie A, Goto S, Angchaisuksiri P, Nielsen JD, Kayani G, Pieper KS, Schellong S, Bounameaux H, Mantovani LG, Prandoni P, Kakkar AK, GARFIELD-VTE investigators, (2019) Characteristics and management of patients with venous thromboembolism: the GARFIELD-VTE Registry. Thromb Haemost 119(2):319–327. https://doi.org/10.1055/s-0038-1676611
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Barker-Collo S, Bartels DH, Bell ML, Benjamin EJ et al (2012) Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380(9859):2095–2128. https://doi.org/10.1016/S0140-6736(12)61728-0
Phillippe HM (2017) Overview of venous thromboembolism. Am J Manag Care 23(20 Suppl):S376–S382
Steering Committee for World Thrombosis Day (2014) Thrombosis: a major contributor to the global disease burden. J Thromb Haemost 12(10):1580–1590. https://doi.org/10.1111/jth.12698
Tritschler T, Aujesky D (2017) Venous thromboembolism in the elderly: a narrative review. Thromb Res 155:140–147. https://doi.org/10.1016/j.thromres.2017.05.015
Tzoran I, Hoffman R, Monreal M (2018) Hemostasis and thrombosis in the oldest old. Semin Thromb Hemost 44(7):624–631. https://doi.org/10.1055/s-0038-1657779
Lauber S, Limacher A, Tritschler T, Stalder O, Méan M, Righini M, Aschwanden M, Beer JH, Frauchiger B, Osterwalder J, Kucher N, Lämmle B, Cornuz J, Angelillo-Scherrer A, Matter CM, Husmann M, Banyai M, Staub D, Mazzolai L, Hugli O et al (2018) Predictors and outcomes of recurrent venous thromboembolism in elderly patients. Am J Med 131(6):703.e7-703.e16. https://doi.org/10.1016/j.amjmed.2017.12.015
Münster AM, Rasmussen TB, Falstie-Jensen AM, Harboe L, Stynes G, Dybro L, Hansen ML, Brandes A, Grove EL, Johnsen SP (2019) A changing landscape: temporal trends in incidence and characteristics of patients hospitalized with venous thromboembolism 2006–2015. Thromb Res 176:46–53. https://doi.org/10.1016/j.thromres.2019.02.009
Shakeel M, Thachil J (2017) Dilemmas in the management of venous thromboembolism in older patients. Br J Hosp Med 78(10):552–557
World Health Organization (2020) Decade of healthy ageing 2020–2030. https://cdn.int/media/docs/default-source/decade-of-healthy-ageing/final-decade-proposal/decade-proposal-final-apr2020-en.pdf?sfvrsn=b4b75ebc_25&download=true
Raskob GE, Angchaisuksiri P, Blanco AN, Buller H, Gallus A, Hunt BJ, Hylek EM, Kakkar A, Konstantinides SV, McCumber M, Ozaki Y, Wendelboe A, Weitz JI; ISTH Steering Committee for World Thrombosis Day (2014) Thrombosis: a major contributor to global disease burden. Arterioscler Thromb Vasc Biol 34(11):2363–2371. https://doi.org/10.1161/ATVBAHA.114.304488
Wendelboe AM, McCumber M, Hylek EM, Buller H, Weitz JI, Raskob G; ISTH Steering Committee for World Thrombosis Day (2015) Global public awareness of venous thromboembolism. J Thromb Haemost 13(8):1365–1371. https://doi.org/10.1111/jth.13031
Johnson SA, Eleazer GP, Rondina MT (2016) Pathogenesis, diagnosis, and treatment of venous thromboembolism in older adults. J Am Geriatr Soc 64(9):1869–1878. https://doi.org/10.1111/jgs.14279
Aleidan F (2020) The cumulative incidence and risk factors of recurrent venous thromboembolism in the elderly. Vasc Health Risk Manag 16:437–443. https://doi.org/10.2147/VHRM.S264814
Heit JA (2015) Epidemiology of venous thromboembolism. Nat Rev Cardiol 12(8):464–474. https://doi.org/10.1038/nrcardio.2015.83
Jang MJ, Bang SM, Oh D (2011) Incidence of venous thromboembolism in Korea: from the Health Insurance Review and Assessment Service database. J Thromb Haemost 9(1):85–91. https://doi.org/10.1111/j.1538-7836.2010.04108.x
Curtarelli A, Silva LPC, de Camargo PAB, Pimenta REF, Jaldin R, Bertanha M, Sobreira ML, Yoshida WB (2019) Profilaxia de tromboembolismo venoso, podemos fazer melhor? Perfil de risco e profilaxia de tromboembolismo venoso em Hospital Universitário do interior do Estado de São Paulo. J Vasc Brasil 18:e20180040. https://doi.org/10.1590/1677-5449.004018
Bouée S, Emery C, Samson A, Gourmelen J, Bailly C, Cotté FE (2016) Incidence of venous thromboembolism in France: a retrospective analysis of a national insurance claims database. Thromb J 14:4. https://doi.org/10.1186/s12959-016-0078-0
Couto TZC, Domingues TAM, Morais SCRV, Lopes JL, Lopes CT (2020) Risk of venous thromboembolism and implementation of preventive measures. Enfermeria Clin 30(5):333–339. https://doi.org/10.1016/j.enfcli.2018.12.005
Farhat FCLG, Gregório HCT, Carvalho RDP (2018) Avaliação da profilaxia da trombose venosa profunda em um hospital geral. J Vasc Brasil 17(3):184–192. https://doi.org/10.1590/1677-5449.007017
Fernandes ALC, Andrade AMS, Constança MSC, Oliveira EN (2015) Novos anticoagulantes orais (NOACs) na prevenção de acidente vascular encefálico (AVE) e fenômenos tromboembólicos em pacientes com fibrilação atrial. Rev Soc Brasil Clín Méd 13:2
Mello TT, Carneiro J, Mello GA, Bizzacchi J (2020) Venous thromboembolism in childhood: where is Brazil after 20 years? Hematol Transfus Cell Ther 42(1):62–69. https://doi.org/10.1016/j.htct.2019.01.006
Darze ES, Casqueiro JB, Ciuffo LA, Santos JM, Magalhães IR, Latado AL (2016) Pulmonary embolism mortality in Brazil from 1989 to 2010: gender and regional disparities. Arq Bras Cardiol 106(1):4–12. https://doi.org/10.5935/abc.20160001
World Health Organization (2013) Global action plan for the prevention and control of NCDs 2013–2020. http://www.who.int/nmh/events/ncd_action_plan/en/
Brazilian Institute of Geography and Statistics (2021) Panorama Brasil. 2021. https://cidades.ibge.gov.br/brasil/panorama
Brazil. Ministério da Saúde (2020) AIH Aprovadas segundo região 2019. http://tabnet.datasus.gov.br/cgi/tabcgi.exe?sih/cnv/nruf.def
Brämer GR (1988) International statistical classification of diseases and related health problems. Tenth revision. World Health Statistics quarterly. Rapport Trimestriel de Statistiques Sanitaires Mondiales 41(1):32–36
Antunes JLF, Cardoso MRA (2015) Uso da análise de séries temporais em estudos epidemiológicos. Epidemiologia e Serviços de Saúde. https://doi.org/10.5123/S1679-49742015000300024
Brazil. Ministério da Saúde (2016) Resolução nº510, de 7 abril de 2016. Diário Oficial da União da República Federativa do Brasil. Brasília (Brasil): Ministério da Saúde; 2016. http://conselho.saude.gov.br/resolucoes/2016/Reso510.pdf
Allaert FA, Benzenine E, Quantin C (2017) Hospital incidence and annual rates of hospitalization for venous thromboembolic disease in France and the USA. Phlebology 32(7):443–447. https://doi.org/10.1177/0268355516653005
Huang D, Chan PH, She HL, Wong CK, Ho CW, Cheng YY, Chan EW, Chiang CE, Siu CW (2018) Secular trends and etiologies of venous thromboembolism in Chinese from 2004 to 2016. Thromb Res 166:80–85. https://doi.org/10.1016/j.thromres.2018.04.021
Abreu DRMOM, Oliveira RR, Marcon SS, Mathias TAF, Novaes E (2016) Internação e mortalidade por quedas em idosos no Brasil: Análise de tendência. Ciências e Saude Coletiva. https://doi.org/10.1590/1413-81232018234.09962016
Soares AMM, Mendes TCO, Lima KC, Menezes MM (2019) Causes for hospitalization of elderly individuals due to primary care sensitive conditions and its associated contextual factors. Revista da Associação Médica Brasileira. https://doi.org/10.1590/1806-9282.65.8.1086
Lins JGMG (2019) A concentração de leitos nos municípios do Brasil pode estar associada a pressões de uso no sistema hospitalar do país? Braz J Health Rev. https://doi.org/10.34115/basrv3n4-002
Souza JLD, Kadosaki DJ, Luz PNV, Costa BN (2020) Internações e procedimentos cirúrgicos de urgência de doenças do sistema circulatório no Brasil. Braz J Health Rev. https://doi.org/10.34119/bjhrv3n5-027
Brazilian Society of Geriatrics and Gerontology. As instituições de longa permanência no Brasil. https://www.sbgg-sp.com.br/as-instituicoes-de-longa-permanencia-para-idosos-no-brasil/
Kroep S, Chuang LH, Cohen A, Gumbs P, van Hout B, Monreal M, Willich SN, Gitt A, Bauersachs R, Agnelli G (2018) The impact of co-morbidity on the disease burden of VTE. J Thromb Thrombolysis 46(4):507–515. https://doi.org/10.1007/s11239-018-1732-0
Nunes BP, Batista SRR, de Andrade FB, de Souza PRB, Lima-Costa MF, Facchini LA (2018) Multimorbidade em indivíduos com 50 anos ou mais de idade: ELSI-Brasil. Revista de Saúde Pública. https://doi.org/10.11606/s1518-8787.2018052000637
Pereira IFS, Spyrides MHC, Andrade LMB (2016) Estado nutricional de idosos no Brasil: uma abordagem multinível. Cadernos de Saúde Pública. https://doi.org/10.1590/0102-311X00178814
Hong J, Lee JH, Lee JY, Lee JO, Choi WI, Ahn S, Lim YH, Bang SM, Oh D (2020) Prominent seasonal variation in pulmonary embolism than deep vein thrombosis incidence: a Korean venous thrombosis epidemiology study. Korean J Int Med 35(3):682–691. https://doi.org/10.3904/kjim.2018.370
Ohki AV, van Bellen B (2017) A incidência regional do tromboembolismo venoso no Brasil. J Vasc Bras 16(3):227–231. https://doi.org/10.1590/1677-5449.000517
Brahmandam A, Abougergi MS, Chaar CIO (2017) National trends in hospitalizations for venous thromboembolism. J Vasc Surg 5(5), 621–629.e2. https://doi.org/10.1016/j.jvsv.2017.04.006
Delluc A, Tromeur C, Le Ven F, Gouillou M, Paleiron N, Bressollette L, Nonent M, Salaun PY, Lacut K, Leroyer C, Le Gal G, Couturaud F, Mottier D, EPIGETBO study group, (2016) Current incidence of venous thromboembolism and comparison with 1998: a community-based study in Western France. Thromb Haemost 116(5):967–974. https://doi.org/10.1160/TH16-03-0205
Gouveia M, Pinheiro L, Costa J, Borges M (2016) Embolia Pulmonar em Portugal: Epidemiologia e Mortalidade Intra-Hospitalar [Pulmonary embolism in Portugal: epidemiology and in-hospital mortality]. Acta Med Portuguesa 29(7–8):432–440
Wells PS, Forgie MA, Rodger MA (2014) Treatment of venous thromboembolism. JAMA 311(7):717–728. https://doi.org/10.1001/jama.2014.65
Crous-Bou M, Harrington LB, Kabrhel C (2016) Environmental and genetic risk factors associated with venous thromboembolism. Semin Thromb Hemost 42(8):808–820. https://doi.org/10.1055/s-0036-1592333
Patel H, Sun H, Hussain AN, Vakde T (2020) Advances in the diagnosis of venous thromboembolism: a literature review. Diagnostics (Basel, Switzerland) 10(6):365. https://doi.org/10.3390/diagnostics10060365
Righini M, Goehring C, Bounameaux H, Perrier A (2000) Effects of age on the performance of common diagnostic tests for pulmonary embolism. Am J Med 109(5):357–361. https://doi.org/10.1016/s0002-9343(00)00493-9
Robert-Ebadi H, Righini M (2014) Diagnosis and management of pulmonary embolism in the elderly. Eur J Int Med 25(4):343–349. https://doi.org/10.1016/j.ejim.2014.03.009
Burwen DR, Wu C, Cirillo D, Rossouw JE, Margolis KL, Limacher M, Wallace R, Allison M, Eaton CB, Safford M, Freiberg M (2017) Venous thromboembolism incidence, recurrence, and mortality based on Women’s Health Initiative data and Medicare claims. Thromb Res 150:78–85. https://doi.org/10.1016/j.thromres.2016.11.015
Kort D, van Rein N, van der Meer F, Vermaas HW, Wiersma N, Cannegieter SC, Lijfering WM (2017) Relationship between neighborhood socioeconomic status and venous thromboembolism: results from a population-based study. J Thromb Haemost 15(12):2352–2360. https://doi.org/10.1111/jth.13868
Kourlaba G, Relakis J, Kontodimas S, Holm MV, Maniadakis N (2016) A systematic review and meta-analysis of the epidemiology and burden of venous thromboembolism among pregnant women. Int J Gynaecol Obstet 132(1):4–10. https://doi.org/10.1016/j.ijgo.2015.06.054
Acknowledgements
Coordination for the Improvement of Higher Education Personnel (CAPES) for support in the study.
Author information
Authors and Affiliations
Contributions
MB and VP contributes substantially to the design and planning of the study; in the analysis and interpretation of data; writing and critical review of the article. VSMC contributed to the design and planning of the study; in the analysis and interpretation of data. SGM contributed to the design and planning of the study; writing and critical review of the article.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Barp, M., Carneiro, V.S.M., Malaquias, S.G. et al. Temporal trend in venous thromboembolism hospitalization rates in Brazilian older adults, 2010–2020. J Thromb Thrombolysis 55, 156–165 (2023). https://doi.org/10.1007/s11239-022-02724-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-022-02724-3