Abstract
The cumulative incidence of symptomatic venous thromboembolism (VTE) among patients with malignant gliomas (MG) is estimated to be as high as 36% during the course of therapy. Development of VTE is associated with an increased risk of hospitalization, delays in cancer treatment, and an increased risk of complications including intracranial hemorrhage as well as VTE specific symptoms. Despite the high risk of VTE and associated morbidity, there is no standard recommendations regarding long term outpatient VTE prophylaxis in patients with MG due to the lack of clinical trial evidence in this patient population. In this study, we treated ten patients with newly diagnosed MG with apixaban, 2.5 mg twice daily beginning 2–21 days after craniotomy and continuing for up to 6 months. Unacceptable toxicity was defined by ≥ grade 2 CNS or non-CNS hemorrhage, a thromboembolic event (i.e. stroke) or cardiovascular event requiring anticoagulation or anti-platelet therapy. There were no unacceptable toxicities to report and no treatment-related adverse events. None of the patients on the study were diagnosed with a VTE while receiving apixaban. We conclude that apixaban can be given safely to patients with primary MG shortly after craniotomy and should be considered for VTE prevention in these high-risk patients.


Similar content being viewed by others
References
Stupp R et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352(10):987–996
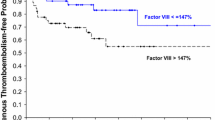
Streiff MB et al (2015) A prospective multicenter study of venous thromboembolism in patients with newly-diagnosed high-grade glioma: hazard rate and risk factors. J Neurooncol 124(2):299–305
Petterson TM et al (2015) Risk of site-specific cancer in incident venous thromboembolism: a population-based study. Thromb Res 135(3):472–478
Walker AJ et al (2013) Incidence of venous thromboembolism in patients with cancer—a cohort study using linked United Kingdom databases. Eur J Cancer 49(6):1404–1413
Perry JR (2010) Anticoagulation of malignant glioma patients in the era of novel antiangiogenic agents. Curr Opin Neurol 23(6):592–596
Perry SL et al (2009) Tinzaparin prophylaxis against venous thromboembolic complications in brain tumor patients. J Neurooncol 95(1):129–134
Robins HI et al (2008) Effect of dalteparin and radiation on survival and thromboembolic events in glioblastoma multiforme: a phase II ECOG trial. Cancer Chemother Pharmacol 62(2):227–233
Carrier M et al (2019) Apixaban to prevent venous thromboembolism in patients with cancer. N Engl J Med 380(8):711–719
Prins MH, Marrel A, Carita P, Anderson D, Bousser MG, Crijns H, Consoli S, Arnould B (2009) Multinational development of a questionnaire assessing patient satisfactionw ith anti-coagulation treatment: the Perception of Anticoagulation Treatment Questionnaire (PACT-Q). Helath Qual Lif Outcomes 6:7–9
Carrier M et al (2014) Lack of evidence to support thromboprophylaxis in hospitalized medical patients with cancer. Am J Med 127(1):82–86
Miranda S, Benhamou Y, Wells P, Carrier M (2019) Safety of primary thrombophylaxis using apixaban in ambulatory cancer patients with intracranial metastatic disease or primary brain tumors. Thromb Haemost 119(11):1886–1887
Artang R, Anderson M, Nielsen JD (2019) Fully automated thromboelastograph TEG 6s to measure anticoagulant effects of direct oral anticoagulants in healthy male volunteers. Res Pract Thromb Haemost 3(3):391–396
Funding
This study was funded by a pilot grant from the Lake Champlain Cancer Research Organization (Grant No. CON000703-LCCRO 2016).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors A. Thomas, H. Wright, K. Chan, H. Ross, P. Prasad, A. Goodwin, and C. Homes have no conflicts of interest to disclose. Dr. Thomas (AAT) is the local principal investigator for clinical trials sponsored by Novocure and by Spectrum Pharmaceuticals.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institution and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Research involving animal rights
This article does not contain any studies with animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Thomas, A.A., Wright, H., Chan, K. et al. Safety of apixaban for venous thromboembolic primary prophylaxis in patients with newly diagnosed malignant glioma. J Thromb Thrombolysis 53, 479–484 (2022). https://doi.org/10.1007/s11239-021-02537-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-021-02537-w