Abstract
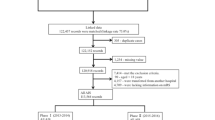
High-performance in-hospital workflow may save time and improve the efficacy of thrombectomy in patients with acute ischemic stroke. However, the optimal in-hospital workflow is far from being formulated, and the current models varied distinctly among centers. This study aimed to evaluate the impacts of in-hospital workflow on functional outcomes after thrombectomy. Patients were enrolled from a multi-center registry program in China. Based on in-hospital managing procedure and personnel involved, two workflow models, neurologist-dominant and non-neurologist-dominant, were identified in the participating centers. Favorable outcome was defined as a mRS score of ≤ 2 at 90 days of stroke onset. After patients being matched with propensity score matching (PSM) method, ratios of favorable outcomes and symptomatic intracerebral hemorrhage (sICH) were compared between patients with different workflow models. Of the 632 enrolled patients, 543 (85.9%) were treated with neurologist-dominant and 89 (14.1%) with non-neurologist-dominant model. 88 patients with neurologist-dominant model and 88 patients with non-neurologist-dominant model were matched with PSM. For the matched patients, no significant differences concerning the ratios of successful recanalization (92.0% vs 87.5%, P = 0.45), sICH (17.0% vs 14.8%, P = 0.85), favorable outcome (42.0% vs 42.0%, P = 1.00) were detected between patients with neurologist-dominant model and those with non-neurologist-dominant model. Patients with neurologist-dominant model had shorter door to puncture time (124 (86–172) vs 156 (120–215), P = 0.005), fewer passes of retriever (2 (1–3) vs 2 (1–4), P = 0.04), lower rate of > 3 passes (11.4% vs 28.4%, P = 0.004), and lower incidence of asymptomatic intracerebral hemorrhage rate (27.3% vs 43.2%, P = 0.045). Although the neurologist-dominant model may decrease in-hospital delay and risk of asymptomatic intracerebral hemorrhage, workflow models may not influence the functional outcome significantly after thrombectomy in patients with acute ischemic stroke.


Similar content being viewed by others
References
Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, Yavagal DR, Ribo M, Cognard C, Hanel RA, Sila CA, Hassan AE, Millan M, Levy EI, Mitchell P, Chen M, English JD, Shah QA, Silver FL, Pereira VM, Mehta BP, Baxter BW, Abraham MG, Cardona P, Veznedaroglu E, Hellinger FR, Feng L, Kirmani JF, Lopes DK, Jankowitz BT, Frankel MR, Costalat V, Vora NA, Yoo AJ, Malik AM, Furlan AJ, Rubiera M, Aghaebrahim A, Olivot JM, Tekle WG, Shields R, Graves T, Lewis RJ, Smith WS, Liebeskind DS, Saver JL, Jovin TG, Investigators DT (2018) Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. New Engl J Med 378:11–21. https://doi.org/10.1056/NEJMoa1706442
Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, McTaggart RA, Torbey MT, Kim-Tenser M, Leslie-Mazwi T, Sarraj A, Kasner SE, Ansari SA, Yeatts SD, Hamilton S, Mlynash M, Heit JJ, Zaharchuk G, Kim S, Carrozzella J, Palesch YY, Demchuk AM, Bammer R, Lavori PW, Broderick JP, Lansberg MG, Investigators D (2018) Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. New Engl J Med 378:708–718. https://doi.org/10.1056/NEJMoa1713973
Goyal M, Menon BK, van Zwam WH, Dippel DWJ, Mitchell PJ, Demchuk AM, Dávalos A, Majoie CBLM, van der Lugt A, de Miquel MA, Donnan GA (2016) Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. The Lancet 387:1723–1731. https://doi.org/10.1016/s0140-6736(16)00163-x
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, Brown M, Demaerschalk BM, Hoh B, Jauch EC, Kidwell CS, Leslie-Mazwi TM, Ovbiagele B, Scott PA, Sheth KN, Southerland AM, Summers DV, Tirschwell DL, American Heart Association Stroke C (2018) Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2018(49):e46–e110. https://doi.org/10.1161/STR.0000000000000158
Schregel K, Behme D, Tsogkas I, Knauth M, Maier I, Karch A, Mikolajczyk R, Hinz J, Liman J, Psychogios MN (2016) Effects of workflow optimization in endovascularly treated stroke patients—a pre-post effectiveness study. PLoS ONE 11:e0169192. https://doi.org/10.1371/journal.pone.0169192
Cheung VJ, Wali AR, Santiago-Dieppa DR, Rennert RC, Brandel MG, Steinberg JA, Hirshman BR, Porras K, Abraham P, Jurf J, Botts E, Olson S, Pannell JS, Khalessi AA (2018) Improving door to groin puncture time for mechanical thrombectomy via iterative quality protocol interventions. Cureus 10:e2300. https://doi.org/10.7759/cureus.2300
Schregel K, Behme D, Tsogkas I, Knauth M, Maier I, Karch A, Mikolajczyk R, Bahr M, Schaper J, Hinz J, Liman J, Psychogios MN (2018) Optimized management of endovascular treatment for acute ischemic stroke. J Vis Exp. https://doi.org/10.3791/56397
Aghaebrahim A, Streib C, Rangaraju S, Kenmuir CL, Giurgiutiu DV, Horev A, Saeed Y, Callaway CW, Guyette FX, Martin-Gill C, Pacella C, Ducruet AF, Jankowitz BT, Jovin TG, Jadhav AP (2017) Streamlining door to recanalization processes in endovascular stroke therapy. J Neurointerv Surg 9:340–345. https://doi.org/10.1136/neurintsurg-2016-012324
Kansagra AP, Meyers GC, Kruzich MS, Cross DT, Moran CJ (2017) Wide variability in prethrombectomy workflow practices in the united states: a multicenter survey. Am J Neuroradiol 38:2238–2242. https://doi.org/10.3174/ajnr.A5384
Zi W, Wang H, Yang D, Hao Y, Zhang M, Geng Y, Lin M, Wan Y, Shi Z, Zhou Z, Wang W, Xu H, Tian X, Lv P, Wang S, Liu W, Wang Z, Liu X, Guo F, Zheng D, Li H, Tu M, Jin P, Xiao G, Liu Y, Xu G, Xiong Y, Liu X, Investigators A (2017) Clinical effectiveness and safety outcomes of endovascular treatment for acute anterior circulation ischemic stroke in China. Cerebrovasc Dis 44:248–258. https://doi.org/10.1159/000478667
Wang H, Thevathasan A, Dowling R, Bush S, Mitchell P, Yan B (2017) Streamlining workflow for endovascular mechanical thrombectomy: lessons learned from a comprehensive stroke center. J Stroke Cerebrovasc Dis 26:1655–1662. https://doi.org/10.1016/j.jstrokecerebrovasdis.2017.04.021
von Kummer R, Broderick JP, Campbell BCV, Demchuk A, Goyal M, Hill MD, Treurniet KM, Majoie CBLM, Marquering HA, Mazya MV, Román LS, Saver JL, Strbian D, Whiteley W, Hacke W (2015) The Heidelberg bleeding classification. Stroke 46:2981–2986. https://doi.org/10.1161/strokeaha.115.010049
Higashida RT, Furlan AJ, Roberts H, Tomsick T, Connors B, Barr J, Dillon W, Warach S, Broderick J, Tilley B, Sacks D (2003) Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke 34:e109–e137. https://doi.org/10.1161/01.STR.0000082721.62796.09
Saver JL, Jahan R, Levy EI, Jovin TG, Baxter B, Nogueira RG, Clark W, Budzik R, Zaidat OO (2012) Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT): a randomised, parallel-group, non-inferiority trial. The Lancet 380:1241–1249. https://doi.org/10.1016/s0140-6736(12)61384-1
Nogueira RG, Lutsep HL, Gupta R, Jovin TG, Albers GW, Walker GA, Liebeskind DS, Smith WS (2012) Trevo versus Merci retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischaemic stroke (TREVO 2): a randomised trial. The Lancet 380:1231–1240. https://doi.org/10.1016/s0140-6736(12)61299-9
Meretoja A, Keshtkaran M, Tatlisumak T, Donnan GA, Churilov L (2017) Endovascular therapy for ischemic stroke: save a minute-save a week. Neurology. 88:2123–2127
Sun CH, Ribo M, Goyal M, Yoo AJ, Jovin T, Cronin CA, Zaidat O, Nogueira R, Nguyen T, Hussain S, Menon BK, Mehta B, Jindal G, Horev A, Norbash A, Leslie-Mazwi T, Wisco D, Gupta R (2014) Door-to-puncture: a practical metric for capturing and enhancing system processes associated with endovascular stroke care, preliminary results from the rapid reperfusion registry. J Am Heart Assoc 3:e000859. https://doi.org/10.1161/jaha.114.000859
Ribo M, Boned S, Rubiera M, Tomasello A, Coscojuela P, Hernández D, Pagola J, Juega J, Rodriguez N, Muchada M, Rodriguez-Luna D, Molina CA (2018) Direct transfer to angiosuite to reduce door-to-puncture time in thrombectomy for acute stroke. J Neurointerv Surg 10:221–224. https://doi.org/10.1136/neurintsurg-2017-013038
Liebeskind DS, Tomsick TA, Foster LD, Yeatts SD, Carrozzella J, Demchuk AM, Jovin TG, Khatri P, von Kummer R, Sugg RM, Zaidat OO, Hussain SI, Goyal M, Menon BK, Al Ali F, Yan B, Palesch YY, Broderick JP (2014) Collaterals at angiography and outcomes in the interventional management of stroke (IMS) III trial. Stroke 45:759–764. https://doi.org/10.1161/strokeaha.113.004072
Goyal M, Menon BK, Coutts SB, Hill MD, Demchuk AM, Penumbra Pivotal Stroke Trial Investigators CSP, the Seaman MRRC (2011) Effect of baseline CT scan appearance and time to recanalization on clinical outcomes in endovascular thrombectomy of acute ischemic strokes. Stroke 42:93–97. https://doi.org/10.1161/STROKEAHA.110.594481
Shi ZS, Liebeskind DS, Xiang B, Ge SG, Feng L, Albers GW, Budzik R, Devlin T, Gupta R, Jansen O, Jovin TG, Killer-Oberpfalzer M, Lutsep HL, Macho J, Nogueira RG, Rymer M, Smith WS, Wahlgren N, Duckwiler GR, Multi Merci T, Investigators T (2014) Predictors of functional dependence despite successful revascularization in large-vessel occlusion strokes. Stroke 45:1977–1984. https://doi.org/10.1161/STROKEAHA.114.005603
Jayaraman MV, Grossberg JA, Meisel KM, Shaikhouni A, Silver B (2013) The clinical and radiographic importance of distinguishing partial from near-complete reperfusion following intra-arterial stroke therapy. AJNR Am J Neuroradiol 34:135–139. https://doi.org/10.3174/ajnr.A3278
Hao Y, Yang D, Wang H, Zi W, Zhang M, Geng Y, Zhou Z, Wang W, Xu H, Tian X, Lv P, Liu Y, Xiong Y, Liu X, Xu G, (2017) Predictors for symptomatic intracranial hemorrhage after endovascular treatment of acute ischemic stroke. Stroke 48:1203–1209. https://doi.org/10.1161/STROKEAHA.116.016368
Baek JH, Kim BM, Heo JH, Nam HS, Kim YD, Park H, Bang OY, Yoo J, Kim DJ, Jeon P, Baik SK, Suh SH, Lee KY, Kwak HS, Roh HG, Lee YJ, Kim SH, Ryu CW, Ihn YK, Kim B, Jeon HJ, Kim JW, Byun JS, Suh S, Park JJ, Lee WJ, Roh J, Shin BS (2018) Number of stent retriever passes associated with futile recanalization in acute stroke. Stroke 49:2088–2095. https://doi.org/10.1161/STROKEAHA.118.021320
Gao F, Lo WT, Sun X, Mo DP, Ma N, Miao ZR (2015) Combined use of mechanical thrombectomy with angioplasty and stenting for acute basilar occlusions with underlying severe intracranial vertebrobasilar stenosis: preliminary experience from a Single Chinese Center. AJNR Am J Neuroradiol 36:1947–1952. https://doi.org/10.3174/ajnr.A4364
Bourcier R, Saleme S, Labreuche J, Mazighi M, Fahed R, Blanc R, Gory B, Kyheng M, Marnat G, Bracard S, Desal H (2018) More than three passes of stent retriever is an independent predictor of parenchymal hematoma in acute ischemic stroke. J Neurointerv Surg 11:625
Feigin VL, Nguyen G, Cercy K, Johnson CO, Alam T, Parmar PG, Abajobir AA, Abate KH, Abd-Allah F, Abejie AN, Abyu GY, Ademi Z, Agarwal G, Ahmed MB, Akinyemi RO, Al-Raddadi R, Aminde LN, Amlie-Lefond C, Ansari H, Asayesh H, Asgedom SW, Atey TM, Ayele HT, Banach M, Banerjee A, Barac A, Barker-Collo SL, Bärnighausen T, Barregard L, Basu S, Bedi N, Behzadifar M, Béjot Y, Bennett DA, Bensenor IM, Berhe DF, Boneya DJ, Brainin M, Campos-Nonato IR, Caso V, Castañeda-Orjuela CA, Castillo Rivas J, Catalá-López F, Christensen H, Criqui MH, Damasceno A, Dandona L, Dandona R, Davletov K, de Courten B, de Veber G, Dokova K, Edessa D, Endres M, Faraon EJA, Farvid MS, Fischer F, Foreman K, Forouzanfar MH, Gall SL, Gebrehiwot TT, Gillum RF, Giroud M, Goulart AC, Gupta R, Gupta R, Hachinski V, Hamadeh RR, Hankey GJ, Hareri HA, Havmoeller R, Hay SI, Hegazy MI, Hibstu DT, James SL, Jeemon P, John D, Jonas JB, Jóźwiak J, Kalani R, Kandel A, Kasaeian A, Kengne AP, Khader YS, Khan AR, Khang Y-H, Khubchandani J, Kim D, Kim YJ, Kivimaki M, Kokubo Y, Kolte D, Kopec JA, Kosen S, Krishnamurthi R, Kumar GA, Lafranconi A, Lavados PM, Legesse Y, Li Y, Liang X, Lo WD, Lorkowski S, Lotufo PA, Loy CT, Mackay MT, Mahdavi M, Majeed A, Malekzadeh R, Malta DC, Mamun AA, Mantovani LG, Martins SCO, Mate KK, Mazidi M, Mehata S, Meier T, Melaku YA, Mendoza W, Mensah GA, Meretoja A, Mezgebe HB, Miazgowski T, Miller TR, Ibrahim NM, Mohammed S, Mokdad AH, Moosazadeh M, Moran AE, Musa KI, Negoi RI, Nguyen M, Nguyen QL, Nguyen TH, Nguyen TT, Nguyen TT, Ningrum DNA, Norrving B, Noubiap JJN, O’Donnell MJ, Olagunju AT, Onuma OK, Owolabi MO, Parasaeian M, Patton GC, Piradov M, Pletcher MA, Pourmalek F, Prakash V, Qorbani M, Rahman M, Rahman MA, Rai RK, Ranta A, Rawaf D, Rawaf S, Renzaho AMN, Robinson SR, Sahathevan R, Sahebkar A, Salomon JA, Santalucia P, Santos IS, Sartorius B, Schutte AE, Sepanlou SG, Shafieesabet A, Shaikh MA, Shamsizadeh M, Sheth KN, Shiferaw MS, Shin M-J, Shiue I, Santos Silva DA, Sobngwi E, Soljak M, Sorensen RJD, Sposato LA, Stranges S, Suliankatchi RA, Tabarés-Seisdedos R, Tanne D, Nguyen CT, Thakur JS, Thrift AG, Tirschwell DL, Topor-Madry R, Tran BX, Tran LT, Truelsen T, Tsilimparis DN, Tyrovolas S, Ukwaja KN, Uthman OA, Vasankari T, Venketasubramanian N et al (2018) Global, regional, and country-specific lifetime risks of stroke, 1990 and 2016. New Engl J Med 379:2429–2437
Wei D, Oxley TJ, Nistal DA, Mascitelli JR, Wilson N, Stein L, Liang J, Turkheimer LM, Morey JR, Schwegel C, Awad AJ, Shoirah H, Kellner CP, De Leacy RA, Mayer SA, Tuhrim S, Paramasivam S, Mocco J, Fifi JT (2017) Mobile interventional stroke teams lead to faster treatment times for thrombectomy in large vessel occlusion. Stroke 48:3295–3300. https://doi.org/10.1161/strokeaha.117.018149
Funding
This project was supported by the National Natural Science Foundation of China (Nos. 81530038, 81220108008 and 81671172) and the Jiangsu Provincial Special Program of Medical Science (No. BL2013025).
Author information
Authors and Affiliations
Consortia
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yang, D., Zi, W., Wang, H. et al. Impacts of in-hospital workflow on functional outcome in stroke patients treated with endovascular thrombectomy. J Thromb Thrombolysis 51, 203–211 (2021). https://doi.org/10.1007/s11239-020-02178-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-020-02178-5