Abstract
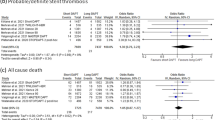
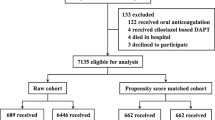
There is still a debate about the safety and efficacy of an aspirin free strategy after percutaneous coronary intervention (PCI). Hence, we performed a meta-analysis comparing aspirin free strategy to dual antiplatlets therapy (DAPT). Randomized trials (RCTs) comparing aspirin free strategy to DAPT in patients who received PCI were included. The primary outcome of interest was bleeding, defined per the Bleeding Academic Research Consortium (BARC). Secondary outcomes included major adverse cardiovascular and cerebrovascular events (MACE); defined as all-cause mortality, myocardial infarction or stroke, the individual component of MACE and stent thrombosis. A total of 4 RCTs with 29,089 patients were included. There was significant reduction in BARC 2,3 or 5 bleeding events in patients who were treated with aspirin free strategy versus DAPT (HR 0.61, 95% CI 0.39−, p = 0.03, I2 = 89%). Moreover, although there was a trend of reduced major bleeding (BARC 3 or 5) outcomes in the aspirin free strategy group compared to the DAPT group, this did not achieve statistical significance (HR 0.63, 95% CI 0.37–1.06, p = 0.08, I2 = 795). Additionally, there was no difference between the aspirin free strategy and DAPT in term of MACE (HR 0.92, 95% CI 0.82–1.03, p = 0.13, I2 = 0%), all-cause mortality (HR 0.89, 95% CI 0.77–1.04, p = 0.15, I2 = 0%), MI (HR 0.89, 95% CI 0.74–1.08, p = 0.24, I2 = 0%), stroke (HR 1.13, 95% CI 0.65–1.99, p = 0.66, I2 = 60%) or stent thrombosis (HR 0.1.01, 95% CI 0.83–1.22, p = 0.93, I2 = 0%). Aspirin free strategy is as effective as DAPT in reducing MACE with better safety profile in term of bleeding.




Similar content being viewed by others
References
Levine GN, Bates ER, Bittl JA et al (2016) 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 68:1082–1115
Capodanno D, Mehran R, Valgimigli M et al (2018) Aspirin-free strategies in cardiovascular disease and cardioembolic stroke prevention. Nat Rev Cardiol 15:480–496
Lewis HD Jr, Davis JW, Archibald DG et al (1983) Protective effects of aspirin against acute myocardial infarction and death in men with unstable angina. Results of a Veterans Administration Cooperative Study. N Engl J Med 309:396–403
Randomised trial of intravenous streptokinase (1988) oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2. ISIS-2 (Second International Study of Infarct Survival) Collaborative Group. Lancet 2:349–360
Diener HC, Bogousslavsky J, Brass LM et al (2004) Aspirin and clopidogrel compared with clopidogrel alone after recent ischaemic stroke or transient ischaemic attack in high-risk patients (MATCH): randomised, double-blind, placebo-controlled trial. Lancet 364:331–337
Moher D, Shamseer L, Clarke M et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4:1
Khan SU, Duran CA, Rahman H, Lekkala M, Saleem MA, Kaluski E (2018) A meta-analysis of continuous positive airway pressure therapy in prevention of cardiovascular events in patients with obstructive sleep apnoea. Eur Heart J 39:2291–2297
Yusuf S, Zhao F, Mehta SR et al (2001) Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med 345:494–502
Mallouk N, Labruyere C, Reny JL et al (2012) Prevalence of poor biological response to clopidogrel: a systematic review. Thromb Haemost 107:494–506
Campo G, Fileti L, Valgimigli M et al (2010) Poor response to clopidogrel: current and future options for its management. J Thromb Thrombolysis 30:319–331
Wallentin L, Becker RC, Budaj A et al (2009) Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 361:1045–1057
Wiviott SD, Braunwald E, McCabe CH et al (2007) Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 357:2001–2015
Vranckx P, Valgimigli M, Juni P et al (2018) Ticagrelor plus aspirin for 1 month, followed by ticagrelor monotherapy for 23 months vs aspirin plus clopidogrel or ticagrelor for 12 months, followed by aspirin monotherapy for 12 months after implantation of a drug-eluting stent: a multicentre, open-label, randomised superiority trial. Lancet 392:940–949
Hahn JY, Song YB, Oh JH et al (2019) Effect of P2Y12 inhibitor monotherapy vs dual antiplatelet therapy on cardiovascular events in patients undergoing percutaneous coronary intervention: the SMART-CHOICE Randomized Clinical Trial. JAMA 321:2428–2437
Mehran R, Baber U, Sharma SK et al (2019) Ticagrelor with or without aspirin in high-risk patients after PCI. N Engl J Med. https://doi.org/10.1056/NEJMoa1908419
Kim C, Hong SJ, Shin DH et al (2019) Randomized evaluation of ticagrelor monotherapy after 3-month dual-antiplatelet therapy in patients with acute coronary syndrome treated with new-generation sirolimus-eluting stents: tICO trial rationale and design. Am Heart J 212:45–52
Schupke S, Neumann FJ, Menichelli M et al (2019) Ticagrelor or prasugrel in patients with acute coronary syndromes. N Engl J Med 381:1254–1534
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
11239_2019_1997_MOESM2_ESM.tif
Supplementary material 2 (TIFF 514 kb). eFigure2: Subgroup analysis for major adverse cardiovascular events (MACE) based on the initial duration of dual antiplatelets therapy in the aspirin free strategy
Rights and permissions
About this article
Cite this article
Osman, M., Farjo, P.D., Osman, K. et al. The dawn of aspirin free strategy after short term dual antiplatelet for percutaneous coronary intervention: meta-analysis of randomized controlled trials. J Thromb Thrombolysis 49, 184–191 (2020). https://doi.org/10.1007/s11239-019-01997-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-019-01997-5