Abstract
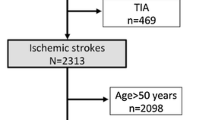
Few data are available on age-related burden and characteristics of embolic stroke of undetermined source (ESUS) in the real world clinical practice. The aim of our study was to provide information about it. We retrospectively analyzed data of patients consecutively admitted to our Stroke Unit along 1 year (2017, November 1st–2018, October 31st). The etiology of ischemic stroke was defined at hospital discharge; ESUS was considered as a subset of cryptogenic stroke, and defined according to the 2014 international criteria. In the analyzed period, 306 patients, 52.3% females, mean age ± SD 77.9 ± 11.9 years, were discharged with diagnosis of ischemic stroke. Ischemic strokes of cardioembolic and lacunar origin were the most frequent subtypes: 30.1% and 29.4%, respectively. Cardioembolic strokes were particularly frequent in patients ≥ 75 years, and almost always associated with atrial fibrillation. Overall, in 80 patients (26.1%) the etiology of stroke was undetermined; in 25 (8.2%) it remained undefined because of death or severe comorbidity, making further diagnostic work-up not worthy. Cryptogenic stroke occurred in 55 patients (18%), and ESUS criteria were satisfied in 39 of them (12.7%). According to age, cryptogenic stroke was diagnosed in 21.1% (21.1% ESUS) of patients < 65 years, 24.2% (19.4% ESUS) of patients aged 65–74 years, 15.5% (9.2% ESUS) of patients ≥ 75 years. After diagnostic work-up, patent foramen ovale was most commonly associated with ESUS (17.9%), especially in patients < 65 years (62.5%); covert paroxysmal atrial fibrillation was detected in 10.5% of ESUS patients ≥ 75 years. In the real world clinical practice, the frequency of ischemic strokes of undetermined etiology, and of those satisfying ESUS criteria, is not negligible, especially in younger patients. A thorough diagnostic work-up, with an age-specific approach, is therefore necessary and of the utmost importance for the identification of stroke etiology, in order to optimize secondary stroke prevention strategies.



Similar content being viewed by others
References
Chen PH, Gao S, Wang YJ et al (2012) Classyfing ischemic stroke, from TOAST to CISS. CNS Neurosci Ther 00:1–5. https://doi.org/10.1111/j.1755-5949.2011.00292.x
Adams HP Jr, Bendixen BH, Kappelle LJ et al (1993) Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 24:35–41
Hart RG, Diener HC, Coutts SB, for the Cryptogenic Stroke/ESUS International Working Group et al (2014) Embolic strokes of undetermined source: the case for a new clinical construct. Lancet Neurol 13:429–438. https://doi.org/10.1016/S1474-4422(13)70310-7
Hart RG, Catanese L, Perera KS et al (2017) Embolic stroke of undetermined source. A systematic review and clinical update. Stroke 48:867–872. https://doi.org/10.1161/STROKEAHA.116.016414
Schulman S, Kearon C, Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis (2005) Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost 3:692–694. https://doi.org/10.1111/j.1538-7836.2005.01204.x
Tatu L, Moulin T, Bogousslavsky J et al (1996) Arterial territories of the human brain: brainstem and cerebellum. Neurology 47:1125–1135
Tatu L, Moulin T, Bogousslavsky J et al (1998) Arterial territories of the human brain: cerebral hemispheres. Neurology 50:1699–1708
Perera KS, Vanassche T, Bosch J, Global Registry Investigators ESUS et al (2016) Global survey of the frequency of atrial fibrillation associated stroke: embolic stroke of undetermined source global registry. Stroke 47:2197–2202. https://doi.org/10.1161/STROKEAHA.116.013378
Perera KS, Vanassche T, Bosch J et al (2016) Embolic strokes of undetermined source: prevalence and patient features in the ESUS Global Registry. Int J Stroke 11:526–533. https://doi.org/10.1177/1747493016641967
Ntaios G, Papavasileiou V, Milionis H et al (2015) Embolic strokes of undetermined source in the Athens stroke registry: an outcome analysis. Stroke 46:2087–2093. https://doi.org/10.1161/STROKEAHA.115.009334
Van Gelder IC, Healey JS, Crijns HJGM et al (2017) Duration of device-detected subclinical atrial fibrillation and occurrence of stroke in ASSERT. Eur Heart J 38:1339–1344. https://doi.org/10.1093/eurheartj/ehx042
Glotzer TV, Daoud EG, Wyse DG et al (2009) The relationship between daily atrial tachyarrhythmia burden from implantable device diagnostics and stroke risk: the TRENDS study. Circ Arrhythm Electrophysiol 2:474–480. https://doi.org/10.1161/CIRCEP.109.849638
Martin DT, Bersohn MM, Waldo AL et al (2015) Randomized trial of atrial arrhythmia monitoring to guide anticoagulation in patients with implanted defibrillator and cardiac resynchronization devices. Eur Heart J 36:1660–1668. https://doi.org/10.1093/eurheartj/ehv115
Goette A, Kalman JM, Aguinaga L et al (2016) EHRA/HRS/APHRS/SOLAECE expert consensus on atrial cardiomyopathies: definition, characterization, and clinical implication. Europace 18:1455–1490. https://doi.org/10.1093/europace/euw161
Guichard J-B, Nattel S (2017) Atrial cardiomyopathy: a useful notion in cardiac disease management or a passing fad? J Am Coll Cardiol 70:756–765. https://doi.org/10.1016/j.jacc.2017.06.033
Ricci B, Chang AD, Hemendinger M et al (2018) A simple score that predicts paroxysmal atrial fibrillation on outpatient cardiac monitoring after embolic stroke of unknown source. J Stroke Cerebrovasc Dis 27:1692–1696. https://doi.org/10.1016/j.jstrokecerebrovasdis.2018.01.028
Masotti L, Grifoni E, Dei A et al (2019) Direct oral anticoagulants in the early phase of non valvular atrial fibrillation-related acute ischemic stroke: focus on real life studies. J Thromb Thrombolysis 47:292–300. https://doi.org/10.1007/s11239-018-1775-2
Hankey GJ (2002) Warfarin-Aspirin Recurrent Stroke Study (WARSS) trial: is warfarin really a reasonable therapeutic alternative to aspirin for preventing recurrent noncardioembolic ischemic stroke? Stroke 33:1723–1726
Sacco RL, Prabhakaran S, Thompson JLP et al (2006) Comparison of warfarin versus aspirin for the prevention of recurrent stroke or death: subgroup analyses from the Warfarin-Aspirin Recurrent Stroke Study. Cerebrovasc Dis 22:4–12. https://doi.org/10.1159/000092331
Hart RG, Sharma M, Mundl H et al (2018) Rivaroxaban for stroke prevention after embolic stroke of undetermined source. N Engl J Med 378:2191–2201. https://doi.org/10.1056/NEJMoa1802686
Diener HC, Sacco RL, Easton JD, RE-SPECT ESUS Steering Committee and Investigators et al (2019) Dabigatran for prevention of stroke after embolic stroke of undetermined source. N Engl J Med 380:1906–1917. https://doi.org/10.1056/NEJMoa1813959
Geisler T, Poli S, Meisner C et al (2017) Apixaban for treatment of embolic stroke of undetermined source (ATTICUS randomized trial): rationale and study design. Int J Stroke 12:985–990. https://doi.org/10.1177/1747493016681019
Kamel H, Longstreth WT, Tirschwell DL et al (2019) The atrial cardiopathy and antithrombotic drugs in prevention after cryptogenic stroke randomized trial: rationale and methods. Int J Stroke 14:207–214. https://doi.org/10.1177/1747493018799981
Kasner SE, Swaminathan B, Lavados P et al (2018) Rivaroxaban or aspirin for patent foramen ovale and embolic stroke of undetermined source: a prespecified subgroup analysis from the NAVIGATE ESUS trial. Lancet Neurol 17:1053–1060. https://doi.org/10.1016/S1474-4422(18)30319-3
Healey JS, Gladstone DJ, Swaminathan B et al (2019) Recurrent stroke with rivaroxaban compared with aspirin according to predictors of atrial fibrillation: secondary analysis of the NAVIGATE ESUS Randomized clinical trial. JAMA Neurol. https://doi.org/10.1001/jamaneurol.2019.0617
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Grifoni, E., Giglio, D., Guazzini, G. et al. Age-related burden and characteristics of embolic stroke of undetermined source in the real world clinical practice. J Thromb Thrombolysis 49, 75–85 (2020). https://doi.org/10.1007/s11239-019-01951-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-019-01951-5