Abstract
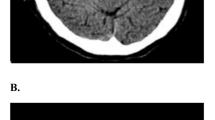
Disappearance of hyperdense middle cerebral artery sign (HMCAS) on non-contrast brain computed tomography (CT) scan is a reliable sign of arterial recanalization after intravenous (IV) thrombolysis for ischemic stroke. We aimed to assess whether stroke etiologic subtype may influence the rate of HMCAS disappearance and the clinical outcome after IV thrombolysis. We conducted a retrospective analysis of data prospectively collected from 1031 consecutive stroke patients treated with IV thrombolysis. Outcome measures were HMCAS disappearance on follow-up CT scan within 22–36 h of IV thrombolysis, neurologic improvement (NIH Stroke Scale [NIHSS] ≤4 points from baseline or NIHSS score of 0) at 7 days, and modified rankin scale (mRS) ≤1 at 3 months. Of 256 patients with HMCAS on admission CT scan, 125 had a cardioembolic stroke, 67 a stroke due to large-artery atherosclerosis (LAA), 58 a stroke of undetermined etiology, and six a stroke secondary to carotid artery dissection. HMCAS disappearance occurred in 145 (56.6 %) patients, neurologic improvement in 122 (55.0 %) patients, and mRS ≤1 in 64 (32.8 %) patients. Compared with cardioembolic stroke patients, patients with stroke due to LAA had lower odds ratios (OR) for HMCAS disappearance (OR 0.29, 95 % CI 0.15–0.58, p < 0.001), neurologic improvement (OR 0.42, 95 % CI 0.22–0.82, p = 0.011), and mRS ≤1 (OR 0.18, 95 % CI 0.06–0.52, p = 0.002). No significant differences in outcome measures were found between cardioembolic strokes and strokes of undetermined etiology. This study suggests that stroke due to LAA is associated with lower rates of HMCAS disappearance, neurologic improvement, and mRS ≤1 after IV thrombolysis, compared with cardioembolic stroke.

Similar content being viewed by others
References
Muir KW, Buchan A, von Kummer R, Rother J, Baron JC (2006) Imaging of acute stroke. Lancet Neurol 5:755–768
Mair G, Boyd EV, Chappell FM et al (2015) Sensitivity and specificity of the hyperdense artery sign for arterial occlusion in acute ischemic stroke. Stroke 46:102–107
Manelfe C, Larrue V, von Kummer R et al (1999) Association of hyperdense middle cerebral artery sign with clinical outcome in patients treated with tissue plasminogen activator. Stroke 30:769–772
Kharitonova T, Ahmed N, Thorén M et al (2009) Hyperdense middle cerebral artery sign on admission CT scan: prognostic significance for ischaemic stroke patients treated with intravenous thrombolysis in the safe implementation of thrombolysis in stroke-international stroke thrombolysis register. Cerebrovasc Dis 27:51–59
Kharitonova T, Thorén M, Ahmed N et al (2009) Disappearing hyperdense middle cerebral artery sign in ischaemic stroke patients treated with intravenous thrombolysis: clinical course and prognostic significance. J Neurol Neurosurg Psychiatry 80:273–278
Mair G, von Kummer R, Morris Z et al (2016) Effect of alteplase on CT hyperdense artery sign and outcome after ischemic stroke. Neurology 86:118–125
Molina CA, Montaner J, Arenillas JF, Ribo M, Rubiera M, Alvarez-Sabín J (2004) Differential pattern of tissue plasminogen activator-induced proximal middle cerebral artery recanalization among stroke subtypes. Stroke 35:486–490
Wahlgren N, Ahmed N, Dávalos A et al (2008) Thrombolysis with alteplase 3–4.5 h after acute ischaemic stroke (SITS-ISTR): an observational study. Lancet 372:1303–1309
Adams HP Jr, Bendixen BH, Kappelle LJ et al (1993) Classification of subtype of acute ischemic stroke: definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in acute stroke treatment. Stroke 24:35–41
Kharitonova T, Mikulik R, Roine RO, Soinne L, Ahmed N, Wahlgren N (2011) Association of early National Institute of Health Stroke Scale improvement with vessel recanalization and functional outcome after intravenous thrombolysis in ischemic stroke. Stroke 42:1638–1643
Liebeskind DS, Sanossian N, Yong WH et al (2011) CT and MRI early vessel signs reflect clot composition in acute stroke. Stroke 42:1237–1243
Sato Y, Ishibashi-Ueda H, Iwakiri T et al (2012) Thrombus components in cardioembolic and atherothrombotic strokes. Thromb Res 130:278–280
Kim SK, Yoon W, Kim TS, Kim HS, Heo TW, Park MS (2015) Histologic analysis of retrieved clots in acute ischemic stroke: correlation with stroke etiology and gradient-echo MRI. AJNR Am J Neuroradiol 36:1756–1762
Kirchhof K, Welzel T, Mecke C, Zoubaa S, Sartor K (2003) Differentiation of white, mixed and red thrombi: value of CT in estimation of the prognosis of thrombolysis—phantom study. Radiology 228:126–130
Kim EY, Heo JH, Lee SK et al (2006) Prediction of thrombolytic efficacy in acute ischemic stroke using thin-section noncontrast CT. Neurology 67:1846–1848
Puig J, Pedraza S, Demchuk A et al (2012) Quantification of thrombus Hounsfield units on noncontrast CT predicts stroke subtype and early recanalization after intravenous recombinant tissue plasminogen activator. AJNR Am J Neuroradiol 33:90–96
Rubiera M, Ribo M, Delgado-Mederos R et al (2006) Tandem internal carotid artery/middle cerebral artery occlusion: an independent predictor of poor outcome after systemic thrombolysis. Stroke 37:2301–2305
Lau YC, Lane DA, Lip GY (2014) Atrial fibrillation in cryptogenic stroke: look harder, look longer, but just jeep looking. Stroke 45:3184–3185
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
Ethical approval for SITS-ISTR was provided in each participant country in accordance with national legislation and local rules. Written informed consent was obtained from all patients enrolled in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Forlivesi, S., Bovi, P., Tomelleri, G. et al. Stroke etiologic subtype may influence the rate of hyperdense middle cerebral artery sign disappearance after intravenous thrombolysis. J Thromb Thrombolysis 43, 86–90 (2017). https://doi.org/10.1007/s11239-016-1404-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-016-1404-x