Abstract
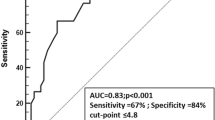
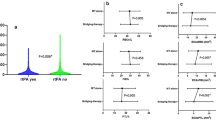
Thrombelastography (TEG) measures coagulation in venous blood. We hypothesized that TEG, by reflecting clot subtype and ex vivo fibrinolysis, might predict fibrinolytic response to tPA as reflected by rapid clinical improvement or hemorrhagic transformation of the infarct. 171 acute ischemic stroke patients treated with tPA were prospectively enrolled. Venous blood for TEG was drawn before and 10 min after tPA bolus. We measured rapid clinical improvement (RCI = 8 point improvement on NIHSS or total NIHSS of 0, 1 at 36 h), Hemorrhagic transformation (HT = any blood on imaging within 36 h), and hyperdense middle cerebral artery sign (HDMCA = biomarker for erythrocyte-rich clot). Multivariable regression models compared TEG parameters after adjusting for potential confounders. No differences in pre- or post-tPA TEG were found between patients with or without RCI. Also, there was no correlation between TEG and HDMCA. Clotting was slightly prolonged in patients with HT (p = 0.046). We failed to find a robust association between TEG and clinical response to tPA. It is likely that arterial clot lysis is determined by factors unrelated to coagulation status as measured by TEG in the venous circulation. It is unlikely that TEG will be useful to predict clinical response to tPA, but may help predict bleeding.

Similar content being viewed by others
References
Saqqur M, Tsivgoulis G, Molina CA, Demchuk AM et al (2008) Symptomatic intracerebral hemorrhage and recanalization after IV rt-PA A multicenter study. Neurology 71:1304–1312
Alexandrov AV, Demchuk AM, Burgin WS, Robinson DJ, Grotta JC (2004) Ultrasound-enhanced thrombolysis for acute ischemic stroke: phase I. Findings of the CLOTBUST trial. J Neuroimaging 14:113–117
Zangerle A, Kiechl S, Spiegel M et al (2007) Recanalization after thrombolysis in stroke patients: predictors and prognostic implications. Neurology 68:39–44
González-Conejero R, Fernández-Cadenas I, Iniesta JA et al (2006) Role of fibrinogen levels and factor XIII V34L polymorphism in thrombolytic therapy in stroke patients. Stroke 37:2288–2293
Marti-Fabregas J, Borrell M, Cocho D et al (2005) Hemostatic markers of recanalization in patients with ischemic stroke treated with rt-PA. Neurology 65:366–370
Jang IK, Gold HK, Ziskind AA et al (1989) Differential sensitivity of erythrocyte-rich and platelet-rich arterial thrombi to lysis with recombinant tissue-type plasminogen activator: a possible explanation for resistance to coronary thrombolysis. Circulation 79:920–928
Boulaftali Y, Ho-Tin-Noe B, Pena A et al (2011) Platelet protease nexin-1, a serpin that strongly influences fibrinolysis and thrombolysis. Circulation 123:1326–1334
Liebeskind DS, Sanossian N, Yong WH et al (2011) CT and MRI early vessel signs reflect clot composition in acute stroke. Stroke 42:1237–1243
Enriquez LJ, Shore-Lesserson L (2009) Point-of-care coagulation testing and transfusion algorithms. Br J Anaesth 103(Suppl 1):i14–i22
Poston R, Gu J, Manchio J et al (2005) Platelet function tests predict bleeding and thrombotic events after off-pump coronary bypass grafting. Eur J Cardiothorac Surg 27:584–591
Bolliger D, Seeberger MD, Tanaka KA (2012) Principles and practice of thromboelastography in clinical coagulation management and transfusion practice. Transfus Med Rev 26:1–13
Onwuemene O, Green D, Keith L (2012) Postpartum hemorrhage management in 2012: predicting the future. Int J Gynecol Obstet 119:3–5
Welsby IJ, Jiao K, Ortel TL et al (2006) The kaolin-activated thrombelastograph® predicts bleeding after cardiac surgery. J Cardiothorac Vasc Anesth 20:531–535
Kawano-Castillo J, Ward E, Elliott A et al (2014) Thrombelastography detects possible coagulation disturbance in patients with intracerebral hemorrhage with hematoma enlargement. Stroke 45:683–688
Shore-Lesserson L, Manspeizer HE, DePerio M, Francis S, Vela-Cantos F, Ergin MA (1999) Thromboelastography-guided transfusion algorithm reduces transfusions in complex cardiac surgery. Anesth Analg 88:312–319
Elliott A, Wetzel J, Roper T et al (2015) Thromboelastography in patients with acute ischemic stroke. Int J Stroke 10:194–201
Windelv NA, Welling KL, Ostrowski SR, Johansson PI (2011) The prognostic value of thrombelastography in identifying neurosurgical patients with worse prognosis. Blood Coagul Fibrinolysis 22:416–419
Yao X, Dong Q, Song Y, Wang Y, Deng Y, Li Y (2014) Thrombelastrography maximal clot strength could predict one-year functional outcome in patients with ischemic stroke. Cerebrovasc Dis 38:182–190
Huang RP, McDonald MM, Wetzel JS et al (2015) Clot strength as measured by thromboelastography correlates with platelet reactivity in stroke patients. Ann Clin Lab Sci 45(3):301–307
Jauch EC, Saver JL, Adams HP, Bruno A, Connors JJ, Demaerschalk BM et al (2013) Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 44:870–947
Kharitonova T, Mikulik R, Roine RO, Soinne L, Ahmed N, Wahlgren N (2013) Association of early National Institutes of Health Stroke Scale improvement with vessel recanalization and functional outcome after intravenous thrombolysis in ischemic stroke. Stroke 42:1638–1643
Wolpert SM, Bruckmann H, Greenlee R, Wechsler L, Pessin MS, del Zoppo GJ (1990) Neuroradiologic evaluation of patients with acute stroke treated with recombinant tissue plasminogen activator. The rt-PA Acute Stroke Study Group. Am J Neuroradiol 14:3–13
Berger C, Fiorelli M, Steiner T et al (2001) Hemorrhagic transformation of ischemic brain tissue asymptomatic or symptomatic? Stroke 32:1330–1335
Moulin T, Cattin F, Crepin-Leblond T et al (1996) Early CT signs in acute middle cerebral artery infarction predictive value for subsequent infarct locations and outcome. Neurology 47:366–375
Alexandrov AV, Demchuk AM, Felberg RA et al (2000) High rate of complete recanalization and dramatic clinical recovery during tPA infusion when continuously monitored with 2-MHz transcranial Doppler monitoring. Stroke 31:610–614
Alexandrov AV, Molina CA, Grotta JC et al (2004) Ultrasound-enhanced systemic thrombolysis for acute ischemic stroke. N Engl J Med 351:2170–2178
Fay WP, Eitzman DT, Shapiro AD, Madison EL, Ginsburg D (1994) Platelets inhibit fibrinolysis in vitro by both plasminogen activator inhibitor-1-dependent and-independent mechanisms. Blood 83:351–356
Collet JP, Montalescot G, Lesty C et al (2001) Disaggregation of in vitro preformed platelet-rich clots by abciximab increases fibrin exposure and promotes fibrinolysis. Arterioscler Thromb Vasc Biol 21:142–148
Riedel CH, Zimmermann P, Jensen-Kondering U, Stingele R, Deuschl G, Jansen O (2011) The importance of size: successful recanalization by intravenous thrombolysis in acute anterior stroke depends on thrombus length. Stroke 42:1775–1777
Rha JH, Saver JL (2007) The impact of recanalization on ischemic stroke outcome a meta-analysis. Stroke 38:967–973
Lee KY, Han SW, Kim SH et al (2007) Early recanalization after intravenous administration of recombinant tissue plasminogen activator as assessed by pre-and post-thrombolytic angiography in acute ischemic stroke patients. Stroke 38:192–193
Gonzalez E, Kashuk JL, Moore EE, Silliman CC (2010) Differentiation of enzymatic from platelet hypercoagulability using the novel thrombelastography parameter delta (Δ). J Surg Res 163:96–101
Gonzalez E, Pieracci FM, Moore EE, Kashuk JL (2010) Coagulation abnormalities in the trauma patient: the role of point-of-care thromboelastography. Semin Thromb Hemost 36:723–737
Kharitonova TV, Melo TP, Andersen G, Egido JA, Castillo J, Wahlgren N (2013) Importance of cerebral artery recanalization in patients with stroke with and without neurological improvement after intravenous thrombolysis. Stroke 44:2513–2518
Acknowledgments
Supported by Tissue and Data Cores of National Institutes of Health 5P50NS044227-08. Haemonetics Corporation loaned a TEG coagulation analyzer Model 5000 and provided supplies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Grotta receives consulting fees from Haemonetics.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
McDonald, M.M., Wetzel, J., Fraser, S. et al. Thrombelastography does not predict clinical response to rtPA for acute ischemic stroke. J Thromb Thrombolysis 41, 505–510 (2016). https://doi.org/10.1007/s11239-015-1280-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-015-1280-9