Abstract
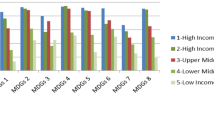
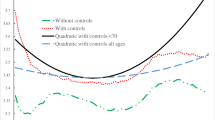
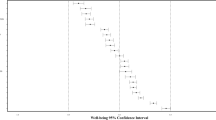
Health inequalities that are avoidable and unfair are considered more relevant for policy intervention. Recent work has improved on using life years (LY) to measure longevity inequality by developing a health indicator—the Realization of Potential Life Years (RePLY)—to adjust for unavoidable mortality risks. This approach, however, estimates unavoidable mortality risks by using the globally lowest mortality risks for each age–sex group of any country, and thus, benchmarking countries at different levels of development against the same unavoidable mortality risks without considering their heterogeneity. The current paper proposes to attempt to control for a country’s national resources in estimating their (conditional) avoidable mortality risks. This allows the construction of a new health indicator—Realization of Conditional Potential Life Years (RCPLY). This paper presents and contrasts the empirical results for LY, RePLY and RCPLY based on life tables for 136 countries from the year 2009.





Similar content being viewed by others
Notes
Health inequality due to risky behaviors such as smoking and drinking could be considered as avoidable but not necessarily unfair if people conduct those activities at free will and with the full knowledge of the consequences. See Fleurbaey and Schokkaert (2009) for a more detailed discussion.
For instance, Allison and Foster (2004) use self-reported health status data from the US National Health Interview Survey to examine health inequality in the US.
The actual population can be used to scale up the stationary population if one is interested in measuring average health or health inequality for a multi-country region or the world as a whole.
We do not use constant international dollars because of the lack of data.
This method is like the DEA method used in this paper, except that it does not involve any input and production function.
Here q is a conditional probability as it is conditional on the person having survived from birth till age x. However, we simply use the term “probability” rather than “conditional probability” throughout the paper so that we can preserve the word “conditional” for cases where the probabilities are measured after controlling for income.
In life tables, life expectancy at age x in country k, \(e_{xk}\), is defined as the number of further years a person is expected to live if the person has lived to age x.
The formulas for these indexes are provided as supplementary material to the paper.
Japan, however, does not have the highest survival probabilities for some age–sex groups.
In Petrie and Tang (2014), we achieve the same by developing an indicator that focuses on health-shortfall instead of health-attainment as in the current paper.
We would like to thank a reviewer for clarifying this.
References
Allanson, P., & Petrie, D. (2013). On the choice of health inequality measure for the longitudinal analysis of income-related health inequalities. Health Economics, 22(3), 353–365.
Allanson, P., & Petrie, D. (2014). Understanding the vertical equity judgements underpinning health inequality measures. Health Economics. doi:10.1002/hec.2984.
Allison, R. A., & Foster, J. (2004). Measuring health inequality using qualitative data. Journal of Health Economics, 23(3), 505–524.
Benjamins, M. R., Hummer, R. A., Eberstein, I. W., & Nam, C. B. (2004). Self-reported health and adult mortality risk: An analysis of cause-specific mortality. Social Science and Medicine, 59(6), 1297–1306.
Bloom, D., & Canning, D. (2009). Population health and economic growth. In M. Spence & M. Lewis (Eds.), Health and Growth, Chapter 3 (pp. 53–76). Washington, D.C: World Bank Publication.
Cai, Y., & Lavely, W. (2003). China’s missing girls: Numerical estimates and effects on population growth. The China Review, 3(2), 13–29.
Caldwell, J. C. (1986). Routes to low mortality in poor countries. Population and Development Review, 12(2), 171–220.
Castelli, A & Nizalova, O (2011). Avoidable mortality: What it means and how it is measured. CHE Research Paper #63, Centre for Health Economics, the University of York.
Centers for Diseases Control and Prevention (CDC). (1986). Premature mortality in the United States: Public health issues in the use of potential life lost. Morbidity and Mortality Weekly Report Supplement, 35(2S), 1s–11s.
Coale, A. J., & Kisker, E. (1986). Mortality crossover: Reality or bad data. Population Studies, 40(3), 389–401.
Coelli, T., Rao, D. S. P., O’Donnell, C. J., & Battese, G. E. (2005). An introduction to efficiency and productivity analysis (2nd ed.). New York: Springer.
Erreygers, G. (2009). Correcting the concentration index. Journal of Health Economics, 28(2), 504–515.
Farr, W. (1885). Methods for comparing local with standard death-rates. London: Office of the Sanitary Institute.
Fleurbaey, M., & Schokkaert, E. (2009). Unfair inequalities in health and health care. Journal of Health Economics, 28(1), 73–90.
Jonhansson, S., & Nygren, O. (1991). The missing girls of China: A new demographic account. Population and Development Review, 17(1), 35–51.
Kjellsson, G., & Gerdtham, U.-G. (2013). Correcting the concentration index for binary variables. Journal of Health Economics, 32(3), 659–670.
Kossarova, L., Holland, W., Nolte, E., & McKee, M. (2009). Measuring avoidable mortality: Methodological note. European Commission: Social and Demographic Analysis.
Le Grand, J. (1987). Inequality in health: Some international comparisons. European Economic Review, 31(1–2), 182–191.
Le Grand, J. (1989). An international comparison of distributions of ages-at-death. In J. Fox (Ed.), Health inequalities in European countries (pp. 75–91). Aldershort: Gower.
Mackenbach, J., & Looman, C. (2013). Life expectancy and national income in Europe, 1900–2008: An update of Preston’s analysis. The International Journal of Epidemiology, 42(4), 1100–1110.
McCracken, K. (2002). What if New South Wales was more equal? NSW Public Health Bulletin, 13(6), 123–127.
Nolte, E., & McKee, C. M. (2004). Does health care save lives? Avoidable mortality revisited. London: The Nuffield Trust.
Norheim, O. F. (2010). Gini impact analysis: Measuring pure health inequity before and after interventions. Public Health Ethics, 3(3), 282–292.
Petrie, D. & Tang, K. K. (2014). Relative health performance in the BRICS over the last 20 years: The winners and losers. Bulletin of the World Health Organization, 92(6), 396-404.
Preston, S. H. (1975). The changing relation between mortality and level of economic development. Population Studies, 29(2), 231–248.
Preston, S., Elo, I. T., & Steward, Q. (1999). Effects of age misreporting on mortality estimates at older ages. Population Studies, 53(2), 165–177.
Rodriguez, M., & Lopez-Valcarcel, B. (2011). Alas, there are no shortcuts to the complexities of the economy. Journal of Epidemiology and Community Health, 65(5), 389–390.
Romeder, J.-M., & McWhinnie, J. R. (1977). Potential years of life lost between ages 1 and 70: An indicator of premature mortality for health planning. International Journal of Epidemiology, 8(2), 143–151.
Rutstein, D. D., Berenberg, W., Chalmers, T. C., et al. (1976). Measuring the quality of medical care. The New England Journal of Medicine, 294(11), 582–588.
Salomon, J., Tandon, A., & Murray, C. (2004). Comparability of self rated health: Cross sectional multi-country survey using anchoring vignettes. BMJ, 328(7434), 258.
Tang, K. K., Chin, J. T. C., & Rao, D. S. P. (2008). Avoidable mortality risks and measurement of wellbeing and inequality. Journal of Health Economics, 27(3), 624–641.
Tang, K. K., Petrie, D., & Rao, D. S. P. (2007). Measuring health inequalities between genders and age groups with Realization of Potential Life Years (RePLY). Bulletin of the World Health Organization, 85(9), 681–688.
Tang, K. K., Petrie, D., & Rao, D. S. P. (2009a). Measuring health inequality with Realization of Potential Life Years (RePLY). Health Economics, 18(S1), s55–s75.
Tang, K. K., Petrie, D., & Rao, D. S. P. (2009b). The income-climate trap of health development: A comparative analysis of African and Non-African countries. Social Science and Medicine, 69(7), 1099–1106.
Tang, K. K., & Rao, D. S. P. (2008). Measuring social disadvantage with avoidable mortality risks. In Clem Tisdell (ed.) Poverty, poverty alleviation, and social disadvantage, Serials Publications. New Delhi. p. 117–131.
Uemura, K. (1989). Excess mortality ratio with reference to the lowest age–sex-specific death rates amongst countries. World Health Statistics Quarterly, 42, 26–41.
Van Doorslaer, E., & Gerdtham, U. G. (2003). Does inequality in self-assessed health predict inequality in survival by income? Evidence from Swedish data. Social Science and Medicine, 57(9), 1621–1629.
Wagstaff, A. (2005). The bounds of the concentration index when the variable of interest is binary, with an application to immunization inequality. Health Economics, 14, 429–432.
Woolsey, T. D. (1981). Toward an index of preventable mortality, 85. Hyattsville: Department of Health and Human Services.
World Health Organization (WHO). (2012). Life Tables for WHO Member States. http://www.who.int/whosis/database/life_tables/life_tables.cfm. Accessed 2012.
World Health Organization (WHO). (2013). Handbook on health inequality monitoring: With a special focus on low- and middle-income countries. Geneva: Switzerland.
Zaridze, D., Lewington, S., Boroda, A., Scélo, G., Karpov, R., Lazarev, A., Konobeevskaya, I., Igitov, V., Terechova, T., Boffetta, P., Sherliker, P., Kong, X., Whitlock, G., Boreham, J., Brennan, P., Peto, R. (2014). Alcohol and mortality in Russia: Prospective observational study of 151000 adults. The Lancet, 383(9927), 1465–1473.
Acknowledgments
The authors would like to acknowledge helpful comments by Roberto Zelli on an earlier version of this paper. Kam Ki Tang would also like to acknowledge the support by a grant from Australian Research Council (DP0878752).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Petrie, D., Tang, K.K. & Rao, D.S.P. Measuring Health Inequality with Realization of Conditional Potential Life Years (RCPLY). Soc Indic Res 122, 21–44 (2015). https://doi.org/10.1007/s11205-014-0677-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11205-014-0677-8