Abstract
Obesity is a preventable risk factor for cerebrovascular disorders and it is associated with cerebral grey and white matter changes. Specifically, individuals with obesity show diminished grey matter volume and thickness, which seems to be more prominent among fronto-temporal regions in the brain. At the same time, obesity is associated with lower microstructural white matter integrity, and it has been found to precede increases in white matter hyperintensity load. To date, however, it is unclear whether these findings can be attributed solely to obesity or whether they are a consequence of cardiometabolic complications that often co-exist with obesity, such as low-grade systemic inflammation, hypertension, insulin resistance, or dyslipidemia. In this narrative review we aim to provide a comprehensive overview of the potential impact of obesity and a number of its cardiometabolic consequences on brain integrity, both separately and in synergy with each other. We also identify current gaps in knowledge and outline recommendations for future research.

Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
Abbreviations
- BMI:
-
Body mass index
- Cam-CAN:
-
Cambridge Centre for Ageing and Neuroscience
- FA:
-
Fractional anisotropy
- FFA:
-
Free fatty acids
- LBP:
-
Lipopolysaccharide binding protein
- TG:
-
Triglycerides
- TNF-alpha:
-
Tumor necrosis factor alpha
- TOF:
-
Time-of-flight
- T2DM:
-
Type 2 diabetes mellitus
References
González-Muniesa P, Mártinez-González MA, Hu FB, Després JP, Matsuzawa Y, Loos RJF, et al. Obesity. Nat Rev Dis Prim. 2017;3.
Schwartz MW, Seeley RJ, Zeltser LM, Drewnowski A, Ravussin E, Redman LM, et al. Obesity pathogenesis: An endocrine society scientific statement. Endocr Rev. 2017;38:267–96.
Bastien M, Poirier P, Lemieux I, Després JP. Overview of epidemiology and contribution of obesity to cardiovascular disease. Prog Cardiovasc Dis. 2014;56:369–81.
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation. International Circulation United States. 2009;120:1640–5.
Stefan N, Schick F, Häring HU. Causes, Characteristics, and Consequences of Metabolically Unhealthy Normal Weight in Humans. Cell Metab. 2017;26:292–300.
Tchernof A, Després J-P. Pathophysiology of Human Visceral Obesity: An Update. Physiol Rev. 2013;93:359–404.
Lemieux I, Poirier P, Bergeron J, Alméras N, Lamarche B, Cantin B, et al. Hypertriglyceridemic waist: a useful screening phenotype in preventive cardiology? Can J Cardiol. 2007;23 Suppl B:23B-31B.
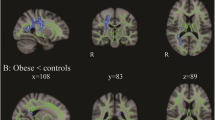
García-García I, Michaud A, Dadar M, Zeighami Y, Neseliler S, Collins DL, et al. Neuroanatomical differences in obesity: meta-analytic findings and their validation in an independent dataset. Int J Obes. 2019;43:943.
Shaw ME, Sachdev PS, Abhayaratna W, Anstey KJ, Cherbuin N. Body mass index is associated with cortical thinning with different patterns in mid- and late-life. Int J Obes. 2018;42:455–61.
Kandel ER, Schwartz JH, Jessell TM, Siegelbaum S, Hudspeth AJ, Mack S. Principles of neural science. New York: McGraw-Hil; 2013.
Cox SR, Lyall DM, Ritchie SJ, Bastin ME, Harris MA, Buchanan CR, et al. Associations between vascular risk factors and brain MRI indices in UK Biobank. Eur Heart J. 2019;40:2290–9.
Caunca MR, Gardener H, Simonetto M, Cheung YK, Alperin N, Yoshita M, et al. Measures of obesity are associated with MRI markers of brain aging: The Northern Manhattan Study. Neurology. 2019;93:e791-803.
Janowitz D, Wittfeld K, Terock J, Freyberger HJ, Hegenscheid K, Völzke H, et al. Association between waist circumference and gray matter volume in 2344 individuals from two adult community-based samples. Neuroimage. 2015;122:149–57.
Opel N, Redlich R, Kaehler C, Grotegerd D, Dohm K, Heindel W, et al. Prefrontal gray matter volume mediates genetic risks for obesity. Mol Psychiatry Nature Publishing Group. 2017;22:703–10.
Beyer F, García-García I, Heinrich M, Schroeter ML, Sacher J, Luck T, et al. Neuroanatomical correlates of food addiction symptoms and body mass index in the general population. Hum Brain Mapp. 2019;1–12.
Kharabian Masouleh S, Arélin K, Horstmann A, Lampe L, Kipping JA, Luck T, et al. Higher body mass index in older adults is associated with lower gray matter volume: implications for memory performance. Neurobiol Aging. 2016;40:1–10.
Opel N, Thalamuthu A, Milaneschi Y, Grotegerd D, Flint C, Leenings R, et al. Brain structural abnormalities in obesity: relation to age, genetic risk, and common psychiatric disorders: Evidence through univariate and multivariate mega-analysis including 6420 participants from the ENIGMA MDD working group. Mol Psychiatry. 2021;26:4839–52.
Franz CE, Xian H, Lew D, Hatton SN, Puckett O, Whitsel N, et al. Body mass trajectories and cortical thickness in middle-aged men: A 42 year longitudinal study starting in young adulthood. Neurobiol Aging. 2019;79:11–21.
Bobb JF, Schwartz BS, Davatzikos C, Caffo B. Cross-sectional and longitudinal association of body mass index and brain volume. Hum Brain Mapp. 2014;35:75–88.
Arnoldussen IAC, Gustafson DR, Leijsen EMC, de Leeuw F-E, Kiliaan AJ. Adiposity is related to cerebrovascular and brain volumetry outcomes in the RUN DMC study. Neurology 2019;93:e864 LP-e878.
Daoust J, Schaffer J, Zeighami Y, Dagher A, García-García I, Michaud A. White Matter Integrity Differences in Obesity: A Meta-Analysis of Diffusion Tensor Imaging Studies. Neurosci Biobehav Rev. 2021; Available from: https://www.sciencedirect.com/science/article/pii/S0149763421003195
Kringelbach ML. The human orbitofrontal cortex: linking reward to hedonic experience. Nat Rev. 2005;6:691–702.
Stice E, Burger K. Neural vulnerability factors for obesity. Clin Psychol Rev. 2019;68:38–53.
García-García I, Morys F, Dagher A. Nucleus accumbens volume is related to obesity measures in an age-dependent fashion. J Neuroendocrinol. 2019; 32:e12812
Birdsill AC, Oleson S, Kaur S, Pasha E, Ireton A, Tanaka H, et al. Abdominal obesity and white matter microstructure in midlife. Hum Brain Mapp. 2017;38:3337–44.
Zhang R, Beyer F, Lampe L, Luck T, Riedel-Heller SG, Loeffler M, et al. White matter microstructural variability mediates the relation between obesity and cognition in healthy adults. Neuroimage. 2018;172:239–49.
Verstynen TD, Weinstein A, Erickson KI, Sheu LK, Marsland AL, Gianaros PJ. Competing physiological pathways link individual differences in weight and abdominal adiposity to white matter microstructure. Neuroimage. 2013;79:129–37.
Bouhrara M, Khattar N, Elango P, Resnick SM, Ferrucci L, Spencer RG. Evidence of association between obesity and lower cerebral myelin content in cognitively unimpaired adults. Int J Obes. 2021;45:850–9.
Lampe L, Zhang R, Beyer F, Huhn S, Kharabian Masouleh S, Preusser S, et al. Visceral obesity relates to deep white matter hyperintensities via inflammation. Ann Neurol. 2019;85:194–203.
Wardlaw JM, Smith C, Dichgans M. Small vessel disease: mechanisms and clinical implications. Lancet Neurol. 2019;18:684–96.
Ronan L, Alexander-Bloch AF, Wagstyl K, Farooqi S, Brayne C, Tyler LK, et al. Obesity associated with increased brain age from midlife. Neurobiol Aging. 2016;47:63–70.
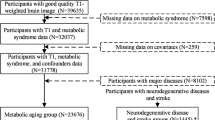
Morys F, Dadar M, Dagher A. Association between mid-life obesity, its metabolic consequences, cerebrovascular disease and cognitive decline. J Clin Endocrinol Metab. United States; 2021;
Allen B, Muldoon MF, Gianaros PJ, Jennings JR. Higher Blood Pressure Partially Links Greater Adiposity to Reduced Brain White Matter Integrity. Am J Hypertens. 2016;29:1029–37.
Alfaro FJ, Gavrieli A, Saade-Lemus P, Lioutas VA, Upadhyay J, Novak V. White matter microstructure and cognitive decline in metabolic syndrome: A review of diffusion tensor imaging. Metabolism. 2018;78:52–68.
Reilly SM, Saltiel AR. Adapting to obesity with adipose tissue inflammation. Nat Rev Endocrinol. 2017;13:633–43.
Longo M, Zatterale F, Naderi J, Parrillo L, Formisano P, Raciti GA, et al. Adipose tissue dysfunction as determinant of obesity-associated metabolic complications. Int J Mol Sci. 2019;20.
Lumeng CN, Saltiel AR. Inflammatory links between obesity and metabolic disease. J Clin Invest. 2011;121:2111–7.
Hotamisligil GS. Inflammation and metabolic disorders. Nature. 2006;444:860–7.
Olefsky JM, Glass CK. Macrophages, inflammation, and insulin resistance. Annu. Rev. Physiol. 2009.
Guillemot-Legris O, Muccioli GG. Obesity-induced neuroinflammation: beyond the hypothalamus. Trends Neurosci. 2017;40:237–53.
Baufeld C, Osterloh A, Prokop S, Miller KR, Heppner FL. High-fat diet-induced brain region-specific phenotypic spectrum of CNS resident microglia. Acta Neuropathol. 2016;132:361–75.
Cazettes F, Cohen JI, Yau PL, Talbot H, Convit A. Obesity-mediated inflammation may damage the brain circuit that regulates food intake. Brain Res. 2011;1373:101–9.
Prats-Soteras X, Jurado MA, Ottino-González J, García-García I, Segura B, Caldú X, et al. Inflammatory agents partially explain associations between cortical thickness, surface area, and body mass in adolescents and young adulthood. Int J Obes. 2020;44:1487–96.
Debette S, Beiser A, Hoffmann U, Decarli C, O’Donnell CJ, Massaro JM, et al. Visceral fat is associated with lower brain volume in healthy middle-aged adults. Ann Neurol. 2010;68:136–44.
Syme C, Pelletier S, Shin J, Abrahamowicz M, Leonard G, Perron M, et al. Visceral fat-related systemic inflammation and the adolescent brain: a mediating role of circulating glycerophosphocholines. Int J Obes. 2019;43:1223–30.
Moreno-Navarrete JM, Blasco G, Puig J, Biarnés C, Rivero M, Gich J, et al. Neuroinflammation in obesity: Circulating lipopolysaccharide-binding protein associates with brain structure and cognitive performance. Int J Obes. 2017;41:1627–35.
Adelantado-Renau M, Esteban-Cornejo I, Rodriguez-Ayllon M, Cadenas-Sanchez C, Gil-Cosano JJ, Mora-Gonzalez J, et al. Inflammatory biomarkers and brain health indicators in children with overweight and obesity: The ActiveBrains project. Brain Behav Immun. 2019;81:588–97.
do Carmo JM, da Silva AA, Wang Z, Fang T, Aberdein N, de Lara Rodriguez CEP, et al. Obesity-Induced Hypertension: Brain Signaling Pathways. Curr Hypertens Rep 2016;18.
Iadecola C, Davisson RL. Hypertension and Cerebrovascular Dysfunction. Cell Metab. 2008;7:476–84.
Cipolla MJ, Liebeskind DS, Chan SL. The importance of comorbidities in ischemic stroke: Impact of hypertension on the cerebral circulation. J Cereb Blood Flow Metab. 2018;38:2129–49.
Kelly DM, Rothwell PM. Blood pressure and the brain: The neurology of hypertension. Pract Neurol. 2020;20:100–11.
Dahlöf B. Prevention of Stroke in Patients with Hypertension. Am J Cardiol. 2007;100.
Chauhan G, Adams HHH, Satizabal CL, Bis JC, Teumer A, Sargurupremraj M, et al. Genetic and lifestyle risk factors for MRI-defined brain infarcts in a population-based setting. Neurology. 2019;92:E486-503.
Cox S, Ritchie S, Fawns-Ritchie C, Tucker-Drob E, Deary I. Brain imaging correlates of general intelligence in UK Biobank. Intelligence 2019;76:599472.
Fuhrmann D, Nesbitt D, Shafto M, Rowe JB, Price D, Gadie A, et al. Strong and specific associations between cardiovascular risk factors and white matter micro- and macrostructure in healthy aging. Neurobiol Aging. 2019;74:46–55.
Williams OA, An Y, Beason-Held L, Huo Y, Ferrucci L, Landman BA, et al. Vascular burden and APOE ε4 are associated with white matter microstructural decline in cognitively normal older adults. Neuroimage. 2019;188:572–83.
De Havenon A, Majersik JJ, Tirschwell DL, McNally JS, Stoddard G, Rost NS. Blood pressure, glycemic control, and white matter hyperintensity progression in type 2 diabetics. Neurology. 2019;92:E1168–75.
Seshadri S, Wolf PA, Beiser A, Vasan RS, Wilson PWF, Kase CS, et al. Elevated midlife blood pressure increases stroke risk in elderly persons: The Framingham study. Arch Intern Med. 2001;161:2343–50.
Lane CA, Barnes J, Nicholas JM, Sudre CH, Cash DM, Parker TD, et al. Associations between blood pressure across adulthood and late-life brain structure and pathology in the neuroscience substudy of the 1946 British birth cohort (Insight 46): an epidemiological study. Lancet Neurol 2019;18:942–52. 4422(19)30228–5
Iadecola C, Gottesman RF. Neurovascular and Cognitive Dysfunction in Hypertension: Epidemiology, Pathobiology, and Treatment. Circ Res. 2019;124:1025–44.
Alateeq K, Walsh EI, Cherbuin N. Higher Blood Pressure is Associated with Greater White Matter Lesions and Brain Atrophy: A Systematic Review with Meta-Analysis. J Clin Med. 2021;10:637.
Schaare HL, Kharabian Masouleh S, Beyer F, Kumral D, Uhlig M, Reinelt JD, et al. Association of peripheral blood pressure with gray matter volume in 19- to 40-year-old adults. Neurology. 2019;92:e758–73.
Maciejczyk M, Żebrowska E, Chabowski A. Insulin resistance and oxidative stress in the brain: What’s new? Int. J. Mol. Sci. 2019. p. 874.
Kullmann S, Heni M, Hallschmid M, Fritsche A, Preissl H, Häring HU. Brain insulin resistance at the crossroads of metabolic and cognitive disorders in humans. Physiol Rev. 2016;96:1169–209.
Boden G. Obesity, insulin resistance and free fatty acids. Curr Opin Endocrinol Diabetes Obes. 2011;18:139–43.
Zeyda M, Stulnig TM. Obesity, inflammation, and insulin resistance - A mini-review Gerontology; 2009. p. 379–86.
Lebovitz H. Insulin resistance: definition and consequences. Exp Clin Endocrinol Diabetes. 2001;109:S135–48.
Sripetchwandee J, Chattipakorn N, Chattipakorn SC. Links between obesity-induced brain insulin resistance, brain mitochondrial dysfunction, and dementia. Front. Endocrinol. 2018. p. 496.
Chen L, Chen R, Wang H, Liang F. Mechanisms Linking Inflammation to Insulin Resistance. Int. J. Endocrinol. Hindawi Limited; 2015.
de la Monte SM. Insulin Resistance and Neurodegeneration: Progress Towards the Development of New Therapeutics for Alzheimer’s Disease. Drugs 2017. p. 47–65.
Dandona P, Aljada A, Bandyopadhyay A. Inflammation: The link between insulin resistance, obesity and diabetes. Trends Immunol. 2004. p. 4–7.
Whitmer RA. Type 2 diabetes and risk of cognitive impairment and dementia. Curr. Neurol. Neurosci. Rep. 2007. p. 373–80.
Najem D, Bamji-Mirza M, Chang N, Liu QY, Zhang W. Insulin resistance, neuroinflammation, and Alzheimer’s disease. Rev. Neurosci. 2014. p. 509–25.
Lu R, Aziz NA, Diers K, Stöcker T, Reuter M, Breteler MMB. Insulin resistance accounts for metabolic syndrome-related alterations in brain structure. Hum Brain Mapp. 2021;42:2434–44.
Ryu SY, Coutu JP, Rosas HD, Salat DH. Effects of insulin resistance on white matter microstructure in middle-aged and older adults. Neurology. 2014;82:1862–70.
Shin J, Pelletier S, Richer L, Pike GB, Gaudet D, Paus T, et al. Adiposity‐related insulin resistance and thickness of the cerebral cortex in middle‐aged adults. J Neuroendocrinol 2020;32:e12921.
Dearborn JL, Schneider ALC, Sharrett AR, Mosley TH, Bezerra DC, Knopman DS, et al. Obesity, Insulin Resistance, and Incident Small Vessel Disease on Magnetic Resonance Imaging: Atherosclerosis Risk in Communities Study. Stroke. 2015;46:3131–6.
Willette AA, Xu G, Johnson SC, Birdsill AC, Jonaitis EM, Sager MA, et al. Insulin resistance, brain atrophy, and cognitive performance in late middle-aged adults. Diabetes Care. 2013;36:443–9.
Oliveira BC de L, Bellozi PMQ, Reis HJ, de Oliveira ACP. Inflammation as a Possible Link Between Dyslipidemia and Alzheimer’s Disease. Neuroscience 2018. p. 127–41.
Park JH, Hong KS, Lee EJ, Lee J, Kim DE. High levels of apolipoprotein B/AI ratio are associated with intracranial atherosclerotic stenosis. Stroke. 2011;42:3040–6.
Tóth ME, Dukay B, Hoyk Z, Sántha M. Cerebrovascular Changes and Neurodegeneration Related to Hyperlipidemia: Characteristics of the Human ApoB-100 Transgenic Mice. Curr Pharm Des. 2020;26:1486–94.
Bowman GL, Kaye JA, Quinn JF. Dyslipidemia and Blood-Brain Barrier Integrity in Alzheimer’s Disease. Curr Gerontol Geriatr Res. 2012;2012:184042.
Wardlaw JM, Makin SJ, Valdés Hernández MC, Armitage PA, Heye AK, Chappell FM, et al. Blood-brain barrier failure as a core mechanism in cerebral small vessel disease and dementia: evidence from a cohort study. Alzheimer’s Dement. 2017;13:634–43.
Schwarz NF, Nordstrom LK, Pagen LHG, Palombo DJ, Salat DH, Milberg WP, et al. Differential associations of metabolic risk factors on cortical thickness in metabolic syndrome. NeuroImage Clin. 2018;17:98–108.
Ward. Low HDL cholesterol is associated with lower gray matter volume in cognitively healthy adults. Front Aging Neurosci2010;2:29.
Shan H, Li P, Liu H, Nie B, Yin X, Zhang T, et al. Gray matter reduction related to decreased serum creatinine and increased triglyceride, Hemoglobin A1C, and low-density lipoprotein in subjects with obesity. Neuroradiology. 2019;61:703–10.
Crisby M, Bronge L, Wahlund L-O. Low Levels of High Density Lipoprotein Increase the Severity of Cerebral White Matter Changes: Implications for Prevention and Treatment of Cerebrovascular Diseases. Curr Alzheimer Res. 2010;7:534–9.
Bokura H, Yamaguchi S, Iijima K, Nagai A, Oguro H. Metabolic Syndrome Is Associated With Silent Ischemic Brain Lesions. Stroke. 2008;39:1607–9.
Williams VJ, Leritz EC, Shepel J, Mcglinchey RE, Milberg WP, Rudolph JL, et al. Interindividual variation in serum cholesterol is associated with regional white matter tissue integrity in older adults. Hum Brain Mapp. 2013;34:1826–41.
Iriondo A, García-Sebastian M, Arrospide A, Arriba M, Aurtenetxe S, Barandiaran M, et al. Plasma lipids are associated with white matter microstructural changes and axonal degeneration. Brain Imaging Behav Springer. 2021;15:1043–57.
Piché ME, Tchernof A, Després JP. Obesity Phenotypes, Diabetes, and Cardiovascular Diseases. Circ Res. 2020;1477–500.
Hansson GK. Inflammation, Atherosclerosis, and Coronary Artery Disease. N Engl J Med. 2005;352:1685–95.
Coucha M, Abdelsaid M, Ward R, Abdul Y, Ergul A. Impact of Metabolic Diseases on Cerebral Circulation: Structural and Functional Consequences. Compr. Physiol. 2018. p. 773–99.
Shi Y, Thrippleton MJ, Makin SD, Marshall I, Geerlings MI, De Craen AJM, et al. Cerebral blood flow in small vessel disease: A systematic review and meta-analysis. J Cereb Blood Flow Metab. 2016;36:1653–67.
Kisler K, Nelson AR, Montagne A, Zlokovic BV. Cerebral blood flow regulation and neurovascular dysfunction in Alzheimer disease. Nat Rev Neurosci. 2017;18:419–34.
Kang KM, Byun MS, Lee JH, Yi D, Choi HJ, Lee E, et al. Association of carotid and intracranial stenosis with Alzheimer’s disease biomarkers. Alzheimer’s Res Ther. Alzheimer’s Research & Therapy; 2020;12:1–11.
Marshall RS, Asllani I, Pavol MA, Cheung YK, Lazar RM. Altered cerebral hemodyamics and cortical thinning in asymptomatic carotid artery stenosis. PLoS ONE. 2017;12:1–14.
Muller M, Van Der Graaf Y, Algra A, Hendrikse J, Mali WP, Geerlings MI. Carotid atherosclerosis and progression of brain atrophy: The SMART-MR Study. Ann Neurol. 2011;70:237–44.
Alhusaini S, Karama S, Nguyen TV, Thiel A, Bernhardt BC, Cox SR, et al. Association between carotid atheroma and cerebral cortex structure at age 73 years. Ann Neurol. 2018;84:576–87.
Laub GA. Time-of-flight method of MR angiography. Magn Reson Imaging Clin N Am. United States; 1995;3:391–8.
Telischak NA, Detre JA, Zaharchuk G. Arterial spin labeling MRI: Clinical applications in the brain. J Magn Reson Imaging. 2015;41:1165–80.
Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation. 2019.
Fjell AM, McEvoy L, Holland D, Dale AM, Walhovd KB. What is normal in normal aging? Effects of aging, amyloid and Alzheimer’s disease on the cerebral cortex and the hippocampus. Prog Neurobiol. 2014;117:20–40.
Liu H, Yang Y, Xia Y, Zhu W, Leak RK, Wei Z, et al. Aging of cerebral white matter. Ageing Res Rev. 2017;34:64–76.
Park DC, Reuter-Lorenz P. The adaptive brain: aging and neurocognitive scaffolding. Annu Rev Psychol. 2009;60:173–96.
Lampe L, Kharabian-Masouleh S, Kynast J, Arelin K, Steele CJ, Löffler M, et al. Lesion location matters: The relationships between white matter hyperintensities on cognition in the healthy elderly. J Cereb Blood Flow Metab. 2019;39:36–43.
Bycroft C, Freeman C, Petkova D, Band G, Elliott LT, Sharp K, et al. The UK Biobank resource with deep phenotyping and genomic data. Nature. 2018;562:203–9.
Van Essen DC, Ugurbil K, Auerbach E, Barch D, Behrens TEJ, Bucholz R, et al. The Human Connectome Project: A data acquisition perspective. Neuroimage. 2012;62:2222–31.
Taylor JR, Williams N, Cusack R, Auer T, Shafto MA, Dixon M, et al. The Cambridge Centre for Ageing and Neuroscience (Cam-CAN) data repository: Structural and functional MRI, MEG, and cognitive data from a cross-sectional adult lifespan sample. Neuroimage. 2017;144:262–9.
Funding
This research was funded by the Spanish Ministry of Science, Innovation and Universities (grant number: PSI2017-8653). Ministerio de Ciencia, Innovación y Universidades, PSI2017-8653, María Ángeles Jurado
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None declared.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
García-García, I., Michaud, A., Jurado, M.Á. et al. Mechanisms linking obesity and its metabolic comorbidities with cerebral grey and white matter changes. Rev Endocr Metab Disord 23, 833–843 (2022). https://doi.org/10.1007/s11154-021-09706-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11154-021-09706-5