Abstract
This study examines the impact of reducing formal care benefits on the well-being of informal caregivers, contributing to the ongoing discourse about establishing sustainable and adequate levels of formal care. We utilize a reform introduced in Japan’s public long-term care insurance system, which curtailed formal care benefits for a group of recipients with low care needs. Employing a difference-in-difference approach with fixed effects on a nationally representative sample of coresident informal caregivers, we explore both the overall and temporal effects of this reform. Our findings reveal that the reform had an adverse impact on caregivers’ physical well-being, leading to diminished mobility and stability. The impact on caregivers’ mental well-being was less clear, reflecting a competing influence of stress and the psychological rewards associated with caregiving. The decline in physical well-being endured over time, while the effects on mental well-being were transient. Additionally, female caregivers exhibited greater vulnerability compared to their male counterparts, experiencing more significant deterioration in both physical and mental well-being. Alarmingly, the reform also negatively influenced the well-being of care recipients, suggesting that reducing formal care benefits does not yield positive outcomes for either caregivers or recipients. This study underscores the necessity of accounting for caregivers’ well-being when evaluating the cost-effectiveness of reducing formal care benefits and advocates for policies aimed at safeguarding female caregivers from health and financial challenges.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
1 Introduction
The rapid demographic transition, accompanied by global growth in the older population, has intensified the need for long-term care (LTC) (Agree & Glaser, 2009). Research indicates that in developed and aging societies, such as Japan, family members constitute the primary caregivers for older people (Colombo et al., 2011; Ministry of Health Labour and Welfare (MHLW), 2014).
However, informal care accessibility has been decreasing for decades, and this trend is expected to continue due to smaller family sizes, lower fertility rates, increased mobility of younger generations, and a higher proportion of women in the labor force, who are typically primary family caregivers. To address this issue, many countries have established formal LTC systems. Japan is one of the early adopters of such a system, implementing a public insurance scheme for LTC in 2000, known as the long-term care insurance (LTCI). The LTCI has been successful in supporting elderly individuals to lead independent lives with dignity and reducing the burden of care duties on family caregivers (Tamiya et al., 2011).
The growing demand for LTC, coupled with a decline in informal care, has placed significant pressure on the fiscal sustainability of public LTC systems, especially given the global economic stagnation. The annual growth rate of public LTC spending was 4.6% from 2005 to 2015 among OECD countries, which was more than double the contemporary GDP growth rate (OECD, 2017). According to projections, public resources devoted to LTC, measured as a proportion of GDP, may triple or more by 2060 (De La Maisonneuve & Martins, 2013). Therefore, balancing the provision of adequate formal care with ensuring the fiscal sustainability of such coverage is one of the most challenging tasks for governments.
In response, many governments have implemented reforms in their LTC systems, often involving reductions in welfare protection (Ranci & Pavolini, 2013). Japan, for instance, initiated a significant reform of the LTCI in 2006, aimed at ensuring the fiscal sustainability of the system by reducing formal care availability for a group of low-need care recipients (see Section 3). However, the reduction in formal care has raised concerns about potential declines in the well-being of both care recipients and caregivers. Informal care often serves as a substitute for formal care, especially among recipients with moderate care needs (Bonsang, 2009; Bremer et al., 2017). Therefore, ongoing discussions regarding the determination of an appropriate level of sustainable and adequate formal care are of paramount importance. Understanding how changes in formal care availability impact the well-being of informal caregivers is crucial from a policy perspective.
Despite the extensive body of studies examining the association between informal care burden and caregivers’ well-being (e.g., Do et al., 2015; Schmitz & Westphal, 2015), there is a scarcity of evidence on the impact of changes in formal care availability on caregivers’ well-being (e.g., Van den Broek and Crundy, 2020). Notably, Miyawaki et al. (2020) analyzed the impact of Japan’s 2006 LTCI reform on caregivers’ well-being using a difference-in-differences approach with propensity score matching (PSM-DD) with nationally representative survey data. They identified worsened self-rated health, depressive symptoms, and musculoskeletal symptoms among caregivers following the reform, underscoring the importance of formal care for caregivers’ well-being. They also showed that the impact did not vary by gender. The findings by Miyawaki et al. (2020) provide significant insights regarding the impact of reduced formal care on well-being. Yet, it remains vital to seek an extensive understanding of the reform’s broader implications, with an emphasis on expanding the analytical horizon. It is particularly advantageous to examine the heterogeneous effects of the reform across various individuals and over time, as well as to consider its consequences for other critical stakeholders, notably the care recipients.
This study aims to comprehensively evaluate the well-being impact of Japan’s 2006 LTCI reform in a natural experimental setting. Utilizing a fixed effect difference-in-differences (FE-DD) approach with nationally representative survey data, we evaluated the impact on a broad range of well-being indicators. More importantly, we conducted an event study to show the temporal changes in the reform’s impact and undertook a detailed re-examination of gender heterogeneity, considering the substantial roles gender plays in informal caregiving in the Japanese societal context. Finally, we extended the scope of our research to examine the reform’s impact on the well-being of care recipients. While a few studies have explored the association between reduced formal care and recipients’ health (Ishibashi & Ikegami, 2010; Ito et al., 2021), their findings were inconclusive and did not support causal inferences. By examining the reform’s impacts on the well-being of both caregivers and recipients, we provided a broader view of the consequences of reducing formal care benefits for multiple stakeholders.
Our findings provide new evidence regarding the impact of reducing care benefits on the well-being of caregivers. We confirm a negative impact of reducing formal care benefits on caregivers’ physical well-being. This is reflected in reduced mobility and stability, along with an increase in symptoms related to the musculoskeletal (by 9.8 pp), systemic (by 6.9 pp), chest (by 5.1 pp), limb (by 4.5 pp), and respiratory systems (by 4.5 pp). Notably, this impact persisted over time, as indicated by significant temporal results. However, our results suggest ambiguous impact on the mental well-being of caregivers. While some specific stress factors, such as challenges in managing financial and domestic responsibilities, initially increased after the reform, these impacts exhibited a transient pattern and diminished over time. Furthermore, in contrast to Miyawaki et al. (2020), we identify significant gender-specific impacts of the reform, highlighting the heightened vulnerability of female caregivers (e.g., a 6.1-pp higher likelihood of physical symptoms) to the reduced formal care benefits compared to their male counterparts (i.e., no deterioration in physical well-being). Intriguingly, in certain cases, male caregivers even experienced reduced stress levels following the reform. This gender disparity may be attributed to differences in how caregivers perceive the costs and benefits of providing informal care. Lastly, our results indicate adverse effects of the reform on the well-being of care recipients (e.g., a 6.6-pp higher likelihood of outpatient visits), suggesting that the reduction in formal care benefits is unlikely to lead to improvements in the well-being of either recipients or caregivers.
We suggest that future LTCI reforms consider the diverse impact of informal caregiving on the well-being of caregivers. It is crucial to adopt a sustainable approach that combines both formal and informal care, finding a balance between fiscal sustainability and the well-being of caregivers and recipients. This approach should consider the needs of those who may struggle with informal caregiving as well as those who may benefit from it.
2 Literature
2.1 Conceptual frameworks
The caregiver stress model is a widely used framework to understand the relationship between the load of informal care and caregivers’ well-being, which serves to evaluate how the availability of formal care affects the welfare of caregivers. It proposes two main stressors that stem from providing informal care: primary and secondary stressors (Pearlin et al., 1990). Primary stressors denote strains or problems that are directly related to the caregiving situation, such as lengthy care hours. Secondary stressors arise from balancing caregiving with other roles, like being a spouse or holding a formal job, and are influenced by primary stressors.
According to the stress model, formal care availability affects caregivers’ well-being by influencing the stressors. Formal care can act as an external resource, reducing caregiving intensity and freeing up caregivers’ time for other responsibilities. A reduction in formal care benefits can increase the burden on caregivers, leading to conflicts with family and work obligations, as well as financial strain. This heightened stress can result in physical and mental health issues for caregivers (Lazarus & Folkman, 1984; McEwen, 1998). Research also suggests that female caregivers, due to perceived and coping differences, are more vulnerable to caregiving stressors than male caregivers and tend to report higher care burdens and lower well-being (Pinquart & Sörensen, 2006; Sharma et al., 2016).
While caregiving can indeed pose challenges, it’s essential to consider that it may not always have detrimental effects on caregivers’ well-being. An alternative perspective acknowledges the potential benefits of providing informal care. Caregivers who perceive caregiving as a choice rather than a burden and have a sense of control over their situation may experience less stress and greater well-being (Roth et al., 2015). Psychological research suggests that individuals tend to experience less stress when they believe they have control over adverse events (Rotter, 1966). Moreover, caregiving can lead to personal growth, altruism, and a sense of purpose for caregivers (Brown & Brown, 2014; Marino et al., 2017).
Overall, providing informal care can have mixed impacts on caregivers’ well-being. Well-being outcomes are typically a result of the balance between these competing impacts, which may vary depending on the relative magnitudes of the costs and benefits associated with caregiving.
2.2 Empirical evidence
Previous research has shown a positive relationship between the utilization of formal care benefits and the well-being of caregivers (Ruppanner & Bostean, 2014).Footnote 1 Access to formal care can mitigate negative outcomes for caregivers, leading to reduced feelings of unhappiness, improved self-rated health, and lower frailty indices. Furthermore, this positive impact tends to be more pronounced in regions with more generous formal care programs (Uccheddu et al., 2019; Verbakel, 2014; Wagner & Brandt, 2015). This improvement is attributed to the fact that professional care workers assume some of the care responsibilities, thereby relieving informal caregivers of their burden (Suanet et al., 2012; Verbakel et al., 2016). This shift in care responsibilities can occur at various levels, including the likelihood of providing care (extensive level), the intensity of caregiving (intensive level), and the types of caregiving tasks (qualitative level).
Several studies have attempted to causally assess the impact of informal caregiving on caregivers’ well-being. For instance, Gonçalves et al., (2021), using panel data to compare couples who utilize formal home care with those who do not, found no significant impact on the physical or mental health of spouses. Dong et al. (2019) employed the instrumental variable (IV) approach to investigate the shift from nursing homes to formal home care on spouse caregivers’ well-being. They found a decline in physical health but an improvement in mental health, attributed to increased care obligations and greater satisfaction, respectively. Similarly, Do et al. (2015), utilizing the IV approach, discovered that providing informal care had adverse effects on multiple dimensions of health for female caregivers in South Korea. Moreover, a recent study by Le and Ibuka (2023) has emphasized the gender disparities in the impact of informal caregiving on caregivers’ well-being. These gender variations are attributed to differences in caregivers’ subjective assessments of the stress and rewards associated with caregiving.
However, there is a scarcity of evidence concerning the well-being impact resulting from changes in formal care availability due to policy reforms. Several studies employed a regime method to identify this causal relationship. Di Novi et al. (2015) highlighted the disparities between North and South Europe in caregivers’ quality of life and concluded that these variations are attributed to gradients in formal care settings, with the north exhibiting greater generosity than the south. Van Den Broek and Grundy (2020) leveraged the different timing of formal care reduction in Sweden and Denmark and found deteriorations in caregivers’ quality of life. Among others, Miyawaki et al. (2020) analyzed the impact of Japan’s 2006 LTCI reform on caregivers’ well-being. They found a detrimental impact of the reform on caregivers’ self-rated health, depressive symptoms, and musculoskeletal symptoms, respectively. They also found no significant variations in the detrimental impact by gender.
3 Background
3.1 The long-term care insurance
In 2000, Japan introduced the LTCI with the aim of socializing care for dependent older individuals and easing the burden on family caregivers. Participation in the LTCI is mandatory for all citizens aged 40 and older (40+), and the monthly premium is determined based on their age and income. Citizens aged 65 or older (65 + ) and those 40+ with specific types of disease are eligible for LTCI benefits (i.e., recipients) provided that they have received a care-need certificate issued by local authorities after undergoing an assessment of their physical and mental statuses (Fu & Noguchi, 2019).Footnote 2 In the initial five years after its introduction, the number of recipients 65+ increased by 1.7 times, rising from 2.47 million to 4.18 million (Appendix Figures A1). This growth was accompanied by an increase in the percentage of citizens 65+ eligible for formal care benefits, climbing from 11% to 16% (Appendix Figure A2).
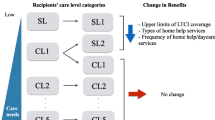
Recipients of formal care are required to bear 10% of the costs until they reach a monthly upper limit.Footnote 3 The upper limit is determined by the recipient’s care-need level, which is divided into six categories ranging from the mildest support-required level (SL) to the most severe care-required level (CL5), with CL1, CL2, CL3, and CL4 in between.Footnote 4 The upper limit for monthly care costs is highest for CL5 and decreases as the care-need level decreases. Notably, neither the assessment of care needs nor the upper limit requires a means test.
The demand for formal care benefits increases with care-need level, particularly for recipients classified as CL3 or above. This increased demand poses a considerable fiscal challenge for the government (Campbell et al., 2010). Public expenditures on LTCI doubled within the initial five years of its introduction, rising from 0.7% of GDP in 2000 to 1.3% in 2005 (MHLW, 2019). To ensure fiscal sustainability, the government implemented a reform in April 2006, which aimed to reduce benefits for low-care-need recipients, namely those in the SL and CL1 categories. This change could potentially result in an increased reliance on informal caregiving.
3.2 The 2006 reform
The 2006 reform was a two-part process. First, it refined the care-need levels, renaming SL to SL1 and adding a new category called SL2. This increased the total number of care-need levels to seven, ranging from the mildest (SL1 and SL2) to the most severe (CL5). Recipients who were previously classified as SL were reassigned to SL1, while those previously classified as CL1 were reassigned as SL2 if their health was expected to remain stable for the next six months; otherwise, they remained in CL1.
Second, the reform limited the type and quantity of formal care available to SL1 and SL2 recipients. The available benefits were narrowed down to focus on preventing recipients’ health conditions from deteriorating, with popular services such as housekeeping and transportation assistance to hospitals no longer available for these groups. Prior to the reform, recipients in SL or CL1 categories used more than 60% of housekeeping services and over half of transportation assistance services (MHLW, 2004). The exclusion of these benefits may have had a significant impact on the well-being of both recipients and caregivers. Additionally, the monthly upper limit for formal care benefits was reduced (Fu et al., 2017). The reduction was mostly significant for recipients in the SL1 category, who could use services worth up to 61,500 JPY (approximately 530 USD) per month before the reform, but only 50,030 JPY (approximately 431 USD) thereafter.Footnote 5 Notably, the reform did not alter the type or quantity of care provided to CL2–CL5 recipients; therefore, they may serve as the control group, as described in Section 4.2.
The reform slowed the previous upward trend in the number of recipients (Appendix Figures A1 and A2). In 2006, the number of recipients remained stable at approximately 4.2 million. This stabilization corresponded to a 0.2-percentage-point decrease in the proportion in total insureds who were eligible for formal care benefits, compared to the preceding year.
4 Methods
4.1 Data
We employed the Comprehensive Survey of Living Conditions (CSLC), a nationally representative and repeated cross-sectional survey in Japan that covers non-institutionalized populations, to conduct our study.Footnote 6 This survey, conducted every three years by the MHLW, consists of four questionnaires assessing household, health, income/savings, and LTC.
The household and health questionnaires, administered to over 600,000 respondents from more than 300,000 households in each wave, collect information on demographic, socioeconomic, and health status of each household member. The income/savings questionnaire involves approximately 100,000 respondents from the full sample, collecting detailed income information. The LTC questionnaire focuses on approximately 6,000 respondents from the full sample who are eligible for formal care benefits. The income/savings and LTC questionnaires are separate samples and do not overlap, and therefore income information was not used in the estimations due to our focus on LTC.
We identified the co-residing primary informal caregivers for each recipient in the LTC questionnaire. To achieve this, we linked the household questionnaire to the LTC questionnaire to access a set of relevant questions in the former one. Specifically, respondents were asked to identify their primary caregiver, if any, with response options including “spouse,” “children or in-laws,” “parents,” “other relatives,” “formal care workers,” and “others.”Footnote 7 If the primary caregiver was a family member, denoted as an informal caregiver, the recipient was further queried about their co-residence with the primary caregiver. If co-residence was confirmed, the recipient was requested to provide the household-member identification number of the caregiver. We cross-referenced this identification number with all family members of the recipient to identify the primary caregiver. We then obtained demographic, socioeconomic, and health status information for each caregiver from the household and health questionnaires. Our sample included surveys conducted between 2001 and 2013, with the earliest available LTC questionnaire in 2001 and excluding waves after 2013 to avoid confounding impacts from the 2015 LTCI reform.Footnote 8 The sample included 18,603 caregivers.
Our sample was limited to co-residing informal caregivers, potentially prompting concerns about its representativeness. To evaluate the extent to which our sample accurately reflects the population in need of care and their corresponding informal caregivers, we reviewed several public statistics. Firstly, as depicted in Appendix Figure A4, during the period of our study, the average proportion of care recipients living alone in Japan was approximately 20%. This suggests that elderly individuals in need of care typically reside with their families. Moreover, as reported in Fu et al., (2023), regardless of living arrangement, the majority of care recipients require informal care, with only 17% of them relying solely on formal care. Additionally, the statistics revealed that at least 85% of recipients receiving informal care were living with their primary caregivers (Appendix Figure A5). These observations emphasize the relevance of our sample for this specific demographic. We further elaborated other potential limitations of the sample in Section 6.
4.2 Measurements
4.2.1 Treatment and control groups
We employed the exogenous variation in care-need levels, which arose from the 2006 reform, to examine the influence of reducing formal care benefits on the well-being of caregivers. The treatment group consisted of informal caregivers of recipients classified as SL prior to the reform and as SL1 following it. These recipients, and therefore their caregivers, experienced a reduction in the type and quantity of formal care available. The control group included caregivers of recipients classified as CL2 or CL3 before and after the reform, who were unaffected by the policy change. The sample of treatment and control groups comprised 8696 caregivers.
It is important to note that we excluded caregivers of CL1 recipients throughout the research period and those of SL2 recipients after the reform. The exclusion of CL1 recipients was due to uncertainty regarding their reassignment to SL2 (potentially “treatment”) or continued classification as CL1 (potentially “control”). The control group also did not include caregivers of CL4 and CL5 recipients. While these caregivers were not directly affected by the reform, they may differ systematically from those in the treatment group because they cared for recipients with the most severe conditions. To assess the robustness of the results, we included these caregivers in the control group and compared the estimates with the primary findings (see Section 5.6).
4.2.2 Outcome variables
We assessed caregivers’ overall well-being using five binary variables: “Any symptom,” “Outpatient visits,” “Limitations in activities of daily living (ADL limitations),” “Self-rated poor health,” and “Being stressed.” Each variable denoted the presence ( = 1) or absence ( = 0) of the respective condition, signifying poor health status.Footnote 9 Except for the last variable measuring mental well-being, the first four gauged physical well-being of caregivers. Reporting physical symptoms and outpatient visits provided insights into caregivers’ general physical well-being, with the latter indicating more severe conditions. The presence of limitations in ADL was a relevant indicator for caregivers’ well-being in Japan, especially considering that many caregivers were elderly themselves (Fu et al., 2023). The use of self-rated poor health aligned with the measurement by Miyawaki et al. (2020), enabling the replication of their findings. Based on the theoretical framework outlined above, we expected that the reduction in formal care benefits has a negative impact on caregivers’ physical well-being, as it may escalate the primary stressors. The impact on mental well-being, however, remains ambiguous, as it involves competing impacts arising from secondary stressors and psychological rewards.
Additionally, we formulated a set of dummy variables for the subcategories of “Any symptom” and “Being stressed” to scrutinize the well-being impacts at a more granular level. Each variable denoted the presence ( = 1) or absence ( = 0) of the respective condition. Within the “Any symptom” category, we identified 11 subcategories associated with physical components, including “systemic symptoms,” “respiratory system,” “musculoskeletal system,” “limb,” “injury,” “eyes and ears,” “chest,” “digestive system,” “gum,” “skin,” and “urinary tract.”Footnote 10 To ensure consistency across survey waves, we categorized the stress factors into nine distinct groups: “family relationship,” “social network,” “reason for living,” “having no free time,” “financial strain,” “own health and LTC issues,” “family health and LTC issues,” “childcare and domestic work,” and “marriage, love, and sexual life.” A detailed depiction of the outcomes is shown in Appendix Table A1.
We expected that the reduction in formal care benefits would substantially increase symptoms related to mobility and stability, particularly affecting systemic and musculoskeletal systems, and limbs. This expectation stems from the physically demanding nature of caregiving responsibilities. Regarding the impact on mental well-being, we expected a mixed result. Caregivers might experience heightened stress due to intensified secondary stressors, such as increased financial strain. However, they could also experience reduced stress due to the psychological rewards associated with caregiving and subsequently express less concern about issues like family health and LTC.
4.2.3 Heterogeneity analyses
Given the potential divergence in perspectives between male and female caregivers when providing informal care, we conducted gender-specific heterogeneity analyses. To gain a deeper understanding of the mechanisms underlying the gender-specific impacts, we conducted additional analyses, considering income levels and the caregiver-recipient relationship, for both male and female caregivers.
Income levels were approximated by per-capita monthly household expenditures, classified as either “Low HH-Exp” or “High HH-Exp,” based on whether the expenditure fell below or above the sample median, respectively. The income level of caregivers is closely intertwined with the secondary stressors associated with caregiving. According to Becker’s theory of time allocation within households (Becker, 1965), the time dedicated to informal caregiving can potentially conflict with other paid social roles, making caregiver income an appropriate indicator of the opportunity costs associated with providing informal care. Higher income levels were considered indicative of greater opportunity costs, implying potentially greater burdens perceived by caregivers.
The caregiver-recipient relationship was categorized as either caring for spouses, parents, or parents-in-law.Footnote 11 This categorization is a proxy for the potential psychological rewards associated with caregiving. Existing literature indicates that the degree of intimacy and emotional connection between caregivers and recipients plays a critical role in moderating the caregiving burden (Lawrence et al., 1998). Caregivers with closer relationships to the recipient may perceive greater psychological rewards, which, in turn, can aid in alleviating the burden associated with caregiving.
4.2.4 Covariates
We controlled for a broad range of covariates, including caregivers’ age (in years), marital status (with married as reference, single, widowed, and divorced), working status (working and not working) health insurance status (with national health insurance as reference, employee health insurance, advance elderly health insurance, and other), pension status (seven types of pensions with basic pension as reference), gender and age (in years) of the care recipients, and number of family members.
4.3 Empirical strategy
4.3.1 Difference-in-differences with fixed effects
We utilized the FE-DD approach, including multiple sets of fixed effects and geographic linear trends in the model.Footnote 12 Instead of employing nonlinear approaches for the binary outcomes, we opted for a linear probability model to avoid difficulties in interpreting the estimates for interaction terms (Puhani, 2012),
\({{\rm{Y}}}_{{it}}\) denotes the outcomes of well-being for respondent \(i\) in year \(t\). \({{\rm{Treat}}}_{{it}}\) and \({{\rm{Post}}}_{t}\) represent the treatment status and post-reform period, respectively, and \({{\bf{X}}}_{{it}}\) represents the set of covariates. \(\gamma\) shows the overall impact of the reform. Based on the theoretical framework, the sign of \(\gamma\) may be positive, negative, or zero. It could be positive if the negative well-being impact induced by the formal care reduction outweighs the positive impact; it could be negative if the opposite is true; and it can be zero if the two impacts cancel one another out.
\({{\boldsymbol{\lambda }}}_{c}\), \({{\boldsymbol{\lambda }}}_{t}\), and \({{\boldsymbol{\lambda }}}_{p}\) represent the FEs at the care level, year level, and prefecture level, respectively. The FEs account for unobservable systematic variations related to care level, time, and geographical context that may influence caregivers’ well-being. These unobservable factors could potentially confound the assessment of the reform’s impact. In addition, \({{\boldsymbol{\Lambda }}}_{p}\) includes either a prefectural linear trend by treatment status \(c{{\boldsymbol{\lambda }}}_{p}\), a prefectural-year trend \(t{{\boldsymbol{\lambda }}}_{p}\), or both. The linear trends could further mitigate the confounding influence of unobserved systematic time and treatment trends in variations concerning the outcomes. As indicated in Table 1, we considered four models, which include all possible combinations of linear trends. Finally, \({\tau }_{{it}}\) is the error term. We clustered standard errors at the levels of care level, year, and prefecture for all estimations. We conducted gender-specific heterogeneity analyses based on Eq. (1) and employed an alternative specification of Eq. (1) to assess the robustness of our findings.Footnote 13
One primary concern when using the DD-FE approach is if the common trend assumption holds. We conducted a placebo test by assuming a placebo reform in 2003,
\({{\rm{Placebo}}}_{t}\) takes the value of zero for the period before 2003 and one for the period between 2003 and 2006; thus, \({\rm{\theta }}\) shall be non-significant if the common trend holds. The other variables are identically defined as in Eq. (1).Footnote 14 We selected the primary model for Eq. (1) based on its performance in the placebo estimation. In the primary model, the common trend should hold for both main and gender-specific heterogeneity analyses.
An additional concern relates to potential changes in the composition of the treatment and control groups before and after the reform. As depicted in Appendix Figures A2, there was a marginal decrease in the percentage of recipients relative to the total insureds after the reform. This decrease could suggest that the reform unintentionally reduced the eligibility rate among low-care-need recipients (a reverse “woodwork effect”), potentially due to their perception that the benefits did not align the effort required for application. Fortunately, Appendix Figure A1 illustrates that the number of CL1 recipients experienced the most substantial changes during the reform; this cohort was excluded from our primary analyses. Additionally, using the data in this figure, we conducted a straightforward analysis by regressing the proportion of CL4–CL5 recipients relative to the total recipients on an indicator for the post-reform period and a linear year trend. If elderly individuals with lower care needs refrained from applying for eligibility, it might have resulted in a scenario where the recipients eligible for formal care benefits predominantly had higher care needs, subsequently leading to an increase in the proportion of CL4–CL5 recipients. However, the analysis revealed no statistically significant increase in the proportion of CL4–CL5 recipients following the reform. Moreover, the magnitude of the change in proportion was minimal, measuring only 0.013 in comparison to the average proportion of 0.241. Moreover, as Appendix Table A2 shows, the proportions of recipients classified as SL and SL1 (treatment group) and CL2–CL3 (control group) remained consistent before and after the reform. Appendix Table A3 also demonstrates little before-and-after difference in caregiver and recipient characteristics across treatment status. In sum, the confounding effect of changes in caregiver composition could be minimal in our study.
Lastly, we addressed the multiple-testing issue that could arise from examining the impacts of the reform on various outcomes. In addition to clustering standard errors, we adjusted standard errors according to the Simes (1986)‘s method for multiple hypothesis testing.
4.3.2 Event study
We further conducted an event study to evaluate the temporal impact of the reform,
where t = 2001, 2007, 2010, 2013.
We replaced the single indicator \({{\rm{Post}}}_{t}\) in Eq. (1) with a set of year dummies \({{\rm{Year}}}_{t}\), where \({{\rm{Year}}}_{2004}\) serves as the reference year. All other variables are defined in an identical manner as outlined in Eq. (1). \({{\rm{\alpha }}}_{t}\) is the set of estimates of interest. Given that 2004 is the reference year, we expected that the pre-reform coefficient \({{\rm{\alpha }}}_{2001}\) is statistically insignificant. The null \({{\rm{\alpha }}}_{2001}\) not only further validates the common trend assumption but also suggests that the reform did not have an anticipation effect. The estimates of years post the reform—\({{\rm{\alpha }}}_{2007}\), \({{\rm{\alpha }}}_{2010}\), and \({{\rm{\alpha }}}_{2013}\)—capture the temporal impact of the reform in each survey year that follows. If the magnitude and statistical significance of the estimates remain constant or increase over time, it would imply an enduring impact of the reform on caregivers’ well-being. Conversely, if the estimates become statistically insignificant or diminish in magnitude over time, it would suggest that the impact of the reform was transitory and not sustained.
5 Results
5.1 Basic statistics
Table 2 shows the basic statistics for outcomes, caregiver characteristics, and covariates adjusted in the estimations. The first two columns (1) and (2) provide information on the control group before and after the policy reform, respectively, while columns (3) and (4) present the corresponding information for the treatment group. Columns (5) and (6) display the before-and-after differences for the control and treatment groups, respectively, along with the statistical significance. Finally, column (7) shows the simple DD estimates without any adjustment.
Upon examining column (7), we observed that caregivers in the treatment group reported an increased changes to the likelihoods of experiencing symptoms (6.00 percentage points, pp) and outpatient visits (8.17 pp) after the reform in comparison to those in the control group. However, we did not detect statistically significant changes in other health dimensions. This includes self-rated poor health, which was observed to have significantly deteriorated in the study by Miyawaki et al. (2020).
When examining the specific symptoms and stress factors, we observed a general decline in specific symptoms, with musculoskeletal (7.4 pp), systemic (6.4 pp), and respiratory (5.7 pp) symptoms showing the most significant deterioration. Although the overall stress level did not exhibit a noticeable change following the reform, there was an elevated stress risk associated with specific factors, such as financial strain (3.1 pp), domestic work (2.9 pp), and social networks (3.6 pp). Intriguingly, the stress risk related to family health and LTC issues decreased by 6.1 pp after the reform. In terms of the magnitude of the changes, it is evident that physical health was more profoundly impacted by the reform than mental health.
In terms of caregivers’ characteristics, following the reform, the treatment group was more inclined to provide care to a spouse, had a higher likelihood of not being employed, and resided in smaller households compared to the control group. Further details on caregiver characteristics based on gender and socioeconomic status are shown in Appendix Figures A6–A8 and Table A5. In general, female caregivers experienced more health deteriorations than their male counterparts.
5.2 Placebo test for common trend and model selection
The disparities in caregiver characteristics between the treatment and control groups underscore the importance of assessing if these distinctions remain consistent over time (i.e., common trend). Figure 1 displays the results from the placebo test for the common trend assumption.
Placebo impact on caregivers’ well-being across models. The markers with 95% confidence intervals represent the estimates of \({\rm{\theta }}\) from Eq. (2). Model 1 controlled for the full set of caregiver characteristics and recipients’ gender and age, as well as year FE, care level FE, and prefecture FE. Based on Model 1, Model 2 further controlled for prefecture-treatment trend, Model 3 further controlled for prefecture-year trend, and Model 4 further controlled for both trends. Standard errors are clustered at the municipal level. Standard errors are clustered at the municipal level. “Outpatient” for outpatient visits, “ADL” for limitations in ADLs, “SRH” for self-report poor health. Standard errors were clustered at the level of care level, year, and prefecture.
All four models demonstrated a common trend between the treatment and control groups prior to the reform. Furthermore, Appendix Figure B1 displays the heterogeneous placebo effects by gender. The models varied in their capacity to satisfy the common trend assumption. Notably, Model 3 proved to be the most robust in adhering to this assumption, both in the primary analysis and the gender-specific analyses. Thus, we adopted Model 3 as the primary model, which controlled for the full set of FEs and prefecture-year trends (Table 1). For reference purposes, we presented the main results from all models in Appendix C, where we confirmed that the direction, magnitude, and statistical inferences of the impacts were consistent across the models.
5.3 Main results
5.3.1 The overall impact of the reform
We first estimated the overall impact of the reform, as shown in Panel A of Table 3. We found that the reform significantly increased the likelihoods of having physical symptoms (by 7.4 pp) and using outpatient visits (by 5.8 pp) among informal caregivers. However, unlike Miyawaki et al. (2020), we did not observe any deteriorations in self-rated health or stress levels following the reform. The reduction in formal care benefits had a negative impact on caregivers’ physical well-being from an objective standpoint. However, this impact was not severe enough to impair their fundamental abilities in managing basic needs (ADL), nor did it lead to a substantial decline in mental well-being.
We further pinpointed the specific physical symptoms and stress factors influenced by the reform. Panels B and C of Table 3 depict these specific impacts in a descending order, respectively. The reform significantly increased the likelihoods of musculoskeletal symptoms (by 9.8 pp), systemic symptoms (by 6.9 pp), chest symptoms (by 5.1 pp), limb symptoms (by 4.5 pp), and respiratory symptoms (by 4.5 pp). Notably, the deterioration in the musculoskeletal system we observed was more than twice as substantial as reported in Miyawaki et al. (2020). The reform also raised the likelihoods of stress due to financial strain (by 4.7 pp) and domestic work (by 3.0 pp) among caregivers. While not statistically significant, the direction of the reform’s impacts on stress factors such as family relations, health, and LTC issues was negative. This suggests the possibility of psychological rewards associated with providing informal care. For enhanced readability, we focused the following estimations on these prominently affected specific symptoms and stress factors, relegating the remaining findings to the appendix.Footnote 15
5.3.2 The temporal impact of the reform
We then delved into the temporal impact of the reform. Figure 2 depicts the results from the event study. The findings aligned with the overall impacts of the reform, revealing significantly increased likelihoods of having physical symptoms and using outpatient visits, alongside minimal changes in other health dimensions. Furthermore, the impacts on symptoms and outpatient visits exhibited varying patterns over time. The risk of having symptoms exhibited an immediate deterioration after the reform (an increase by 8.3 pp in 2007), which was slightly diminished over time. In contrast, the impact on outpatient visits was initially negligible but became significant in the later stage of the study, with an increased likelihood of 7.2 pp in 2013. Given that outpatient visits indicate more severe health conditions compared to reporting symptoms, it is possible that a longer period is required for the impact to become evident.
The temporal impact of reducing formal care benefits on caregivers’ well-being. All estimates were derived based on Model 3 of Eq. (3), which controlled for the full set of caregiver characteristics and recipients’ gender and age, as well as year FE, care level FE, prefecture FE, and prefecture-year trend. The y‐axes share a uniform scale for visual comparability. The markers stand for the estimates of \({{\rm{\alpha }}}_{t}\) in Eq. (3). The thicker and thinner bars represent confidence intervals at the 90% and 95% levels, respectively. Standard errors were clustered at the level of care level, year, and prefecture
It also is worth noting that all estimates preceding the reform were statistically insignificant and of negligible magnitude. This reinforces the findings from the placebo test, showing that the treatment-control disparities remained consistent over time and providing further evidence that the reform had no anticipatory effect.
Figure 3 illustrates the temporal impacts on the specific symptoms and stress factors that were notably influenced by the reform.Footnote 16 The temporal impacts corroborate the overall impacts of the reform. The deteriorations in physical symptoms were generally stable over time, except for a diminishing impact on the systemic system. Specifically, the deteriorations in the musculoskeletal system remained substantial and significant throughout the entire study period, signifying sustained challenges related to mobility and stability among caregivers. In contrast, the impacts on the stress factors exhibited less persistence over time and became statistically insignificant in the later stages of the study, indicating transient mental health consequences resulting from the reduction in formal care benefits.
The temporal impact of reducing formal care benefits on specific symptoms and stress factors. Notes: All estimates were derived based on Model 3 of Eq. (3), which controlled for the full set of caregiver characteristics and recipients’ gender and age, as well as year FE, care level FE, prefecture FE, and prefecture-year trend. The y‐axes share a uniform scale for visual comparability. The markers stand for the estimates of \({{\rm{\alpha }}}_{t}\) in Eq. (3). The thicker and thinner bars represent confidence intervals at the 90% and 95% levels, respectively. Standard errors were clustered at the level of care level, year, and prefecture
5.4 The heterogeneous impacts of the reform
5.4.1 Gender disparities
Table 4 summarizes the gender-specific impact of the reform. Reducing formal care benefits had distinct effects on male and female caregivers. Female caregivers experienced a significant decline in physical well-being, characterized by increased likelihoods of having physical symptoms (by 6.1 pp), using outpatient visits (by 7.9 pp), and having limitations in ADL (by 6.2 pp). In contrast, male caregivers did not exhibit any deterioration in physical well-being, and they became less likely to experience stress (a decrease of 12.8 pp).
The results regarding specific symptoms and stress factors indicate deteriorations in nearly all well-being dimensions among female caregivers. This included elevated likelihoods of musculoskeletal issues (by 10.0 pp), systemic ailments (by 6.9 pp), chest discomfort (by 6.5 pp), respiratory problems (by 7.4 pp), and stress stemming from financial strain (by 5.9 pp) and domestic works (by 4.0 pp). In contrast, male caregivers did not report declines in any of the listed well-being dimensions. In fact, as presented in Appendix Table E1, male caregivers exhibited improved mental well-being, with lower likelihoods of worrying about their own health and LTC needs (a decrease of 9.7 pp) and their family’s health (a decrease of 10.6 pp).Footnote 17
The noteworthy gender-specific impacts we have identified deviate from the conclusions drawn in Miyawaki et al. (2020), which found no evidence indicating distinct effects of the reform on caregivers based on gender. To explore the underlying mechanisms responsible for these gender disparities, we analyzed the impact of the reform with respect to caregivers’ socioeconomic status (income level) and demographic status (caregiver-recipient relationship).
5.4.2 Gender disparities by caregivers’ characteristics
Figure 4 depicts the gender-specific impacts of the reform across income levels and caregiver-recipient relationships, except for male in-law caregivers due to a limited sample size (23 individuals). Among low-income caregivers (column Low HH-Exp) and those providing care for their parents (column Parent), we observed a similarity between genders in terms of both the magnitude and direction of the impacts. However, for high-income caregivers (column High HH-Exp) and those engaged in spousal caregiving (column Spouse), marked gender-based disparities emerge.
Heterogeneous impact of reducing formal care benefits: caregivers’ income levels and caregiver-recipient relationships. All estimates were derived based on Model 3 of Eq. (1), which controlled for the full set of caregiver characteristics and recipients’ gender and age, as well as year FE, care level FE, prefecture FE, and prefecture-year trend. The vertical bars stand for the estimates of \(\gamma\) in Eq. (1). The thicker and thinner horizontal bars represent confidence intervals at the 90% and 95% levels, respectively. Standard errors were clustered at the level of care level, year, and prefecture
The distinctions are driven by the fact that male caregivers experienced minimal or even positive changes in their well-beings within these two categories. To elaborate, male caregivers who were caring for their spouses reported no significant well-being changes following the reform. Remarkably, those with High HH-Exp even reported reduced likelihoods of ADL limitations (by 16 pp), self-reporting poor health (by 15 pp), and experiencing stress (by 19 pp).
Conversely, female caregivers generally reported health deteriorations following the reform, regardless of their socioeconomic or demographic attributes. The particularly vulnerable subgroups of female caregivers comprised those from high-income households and those providing care for their parent-in-laws. For instance, they experienced an increased likelihood of having outpatient visits by 10 pp and 12 pp, respectively. Additional insights from Appendix Figs. E1, E2 indicate that these female caregivers exhibited a heightened likelihood of reporting musculoskeletal, systemic, and chest conditions, along with an increased burden of financial stress.
5.5 Additional impacts of the reform
Our results underscore the adverse impact of reducing formal care benefits on the welfare of informal caregivers. To obtain a more comprehensive understanding of the reform’s consequences, we investigated whether and in what manner the reform influenced the well-being of recipients, a crucial aspect in comprehending the reform’s overall consequences. If informal care delivered by family members and close relatives possessed advantages such as tailed-made care, the net welfare impact of the reform remains ambiguous since it simultaneously reduced the well-being of caregivers while enhancing that of care recipients.
To explore this, we substituted the set of outcome variables outlined in Section 4.2.2 for all care recipients in the LTC questionnaire and examined the effects using the event study. Appendix Figure F1 illustrates that care recipients became 6.6-pp more likely to have outpatient visits and 5.7-pp more likely to experience ADL limitations immediately after the reform. These increments were sustained throughout the study period. However, the mental well-being of care recipients did not exhibit a significant change. Consequently, it appears that the reform led to a decline in the physical well-being of both caregivers and care recipients.
5.6 Robustness checks
The robustness of the main results, based on Eq. (1), is demonstrated in Appendix Figs. G1−G3. The estimates obtained from the robustness checks were close to those of the main results in terms of their direction, magnitude, and statistical inference.
6 Discussion
This study examined the consequences of reducing formal care benefits on the well-being of informal caregivers, using a broad set of well-being indicators. We leveraged the 2006 reform of Japan’s LTCI and investigated not only its overall impact but also its temporal impact. We further examined the impact by caregivers’ gender and socioeconomic statuses.
Our findings point to a negative impact on caregivers’ physical well-being due to the reduction in formal care benefits, which is consistent with previous studies. Furthermore, adding to the literature, our findings indicate that the impact is particularly evident in decreased mobility and stability, particularly accompanied by an increase in symptoms related to musculature, skeleton, and limb. Importantly, this impact has persisted over time, as indicated by consistent temporal trends. However, the mental well-being of caregivers appears to be less affected. While certain stress factors, like managing financial and domestic responsibilities, initially increased after the reform, these impacts were temporary and decreased over time. In addition, contrary to Miyawaki et al.’s (2020) conclusion of null gender-specific effects, our results demonstrate significant gender-specific impacts of the reform. Female caregivers were more adversely affected by the reduced formal care benefits compared to their male counterparts. Interestingly, in some cases, male caregivers even experienced reduced stress levels after the reform. These gender differences may stem from varying perceptions of the costs and benefits associated with providing informal care. Lastly, adding to the literature, our results show a negative impact on the physical well-being of care recipients, indicating that reducing formal care benefits is unlikely to lead to improvements in the well-being of either caregivers or recipients.
Our findings suggest that informal caregiving is accompanied by significant primary stressors, making reducing formal care a risky proposition for caregivers’ physical well-being. The increased caregiving responsibilities exert physical strain on caregivers, leading to musculoskeletal issues that hinder their mobility and stability. Simultaneously, the competing influences of secondary stressors and psychological rewards within caregiving lead to an uncertain impact on caregivers’ mental well-being. Inadequate formal care support hinders caregivers from effectively balancing their caregiving responsibilities with other familial and societal roles. This results in heightened concerns about finance and domestic responsibility, reflecting the opportunity costs associated with dedicating more time and effort to caregiving (Heitmueller & Inglis, 2007). On the flip side, caregiving, especially for males, may yield a sense of reward and control, reducing their concerns about family relations and health/LTC issues (Dong et al., 2019). Furthermore, the impact on mental well-being is less pronounced and enduring than on physical well-being. Caregivers may potentially adapt or acclimate gradually to the heightened caregiving burden, resulting in a more stable mental state over time (De Zwart et al., 2017). Overall, our findings underscore the importance of primary stressors and emphasizes the necessity for comprehensive interventions to alleviate physical burden of caregivers.
The gender-specific impact of reducing formal care benefits contribute new insights to existing literature. These differences can be attributed to the distinct stressors and rewards perceived by female and male caregivers. Female caregivers tend to face more pronounced stressors associated with caregiving compared to their male counterparts. Contemporary societal trends show that women are increasingly engaged in paid employment and play a significant role in their families’ financial stability. However, the responsibility for providing informal care predominantly falls on women. As a result, female caregivers are more likely to experience the opportunity cost of lost income due to providing informal care (Carmichael & Charles, 2003; Le & Ibuka, 2023; Schmitz & Westphal, 2015). Our sample of female caregivers is characterized by a younger age group and a higher likelihood of being married compared to their male counterparts (Appendix Table A5). Balancing their professional, social, and marital obligations while providing extensive care poses a significant challenge for these caregivers, making them particularly susceptible to the reform (Fu et al., 2017; Schmitz and Stroka, 2013; Van Houtven et al., 2013). In contrast, male caregivers tend to experience more psychological rewards compared to their female counterparts. They often engage in caregiving relationships that are more intimate in nature. Our sample of male caregivers primarily provides care to their wives, as opposed to parents-in-law (Appendix Table A5). These closer relationships may result in higher levels of emotional connection and satisfaction derived from fulfilling their caregiving role, thus conferring significant psychological benefits (Collins & Feeney, 2000; Penning & Wu, 2016).
However, the gender-specific impact cannot be fully explained by the disparities in perceived stressors and psychological rewards alone. Even when male and female caregivers have similar income levels or the same relationship to care recipients, female caregivers remain more susceptible to the adverse effects of formal care reductions compared to male caregivers. This suggests that there are additional factors at play that contribute to the gender-specific differences. One possible explanation lies in the nature of the care provided by male and female caregivers. Informal caregiving is often a demanding and challenging task, and caregivers may have little choice but to assume this role (Pearlin, 2010). This situation is particularly pronounced for female caregivers in Japan, where societal gender norms tend to dictate their primary responsibility in providing informal care (Kumagai, 2017; Sharma et al., 2016). These gender norms may place a heavier burden on female caregivers, leading to increased levels of stress and challenges in maintaining their own well-being. Furthermore, male caregivers may have a broader interpretation of informal care than female caregivers. For instance, male caregivers may view tasks such as paperwork or making phone calls as constituting informal care, while female caregivers may view caregiving as encompassing more labor-intensive activities involving both physical and emotional support. This difference in interpretation may lead to variations in the perceived level of caregiving responsibilities between male and female caregivers. Considering these factors, it becomes evident that female caregivers are inherently more vulnerable to formal care reduction, even if they perceive similar stressors and psychological rewards as their male counterparts. The heavier burden placed on female caregivers by societal gender norms, coupled with the labor-intensive nature of their caregiving tasks, may also contribute to the observed gender-specific disparities.
The negative impact of the reform on care recipients adds to the mixed findings in Japanese literature (Ishibashi & Ikegami, 2010; Ito et al., 2021) and contradicts the notion that informal care may be more beneficial than formal care for recipients. For example, Cohen et al. (2002) suggest that informal caregivers, often family members or close acquaintances, possess a deep understanding of the care recipient’s needs, preferences, and values. This understanding allows them to provide highly personalized care tailored to the recipient’s specific requirements. However, our findings emphasize that even for recipients with moderate care needs, formal care services offer specialized and professional care that informal caregivers may find challenging to replicate. Consequently, reducing formal care services is unlikely to have a positive impact on either caregivers or recipients.
This study has several limitations. Due to the data structure, our sample is susceptible to selection issues. Specifically, our sample covers only co-residing primary caregivers, which limits our ability to gain a comprehensive understanding of the reform’s impact on caregivers with lighter care duties or different living arrangements.Footnote 18 As a result, the total impact on the entire caregiver cohort remains ambiguous. Additionally, we cannot observe low-need recipients who may have found it not worthwhile to apply for formal care benefits after the reform, indicating potential selection into the treatment group. Likewise, we are unable to observe high-income caregivers who might have entirely outsourced their care duties by placing recipients in private nursing homes after the reform. This implies that our results for high-income caregivers could potentially be conservative estimates. Lastly, since we could not track transitions into or out of the caregiver role, we are unable to investigate the impact of reducing formal care benefits on the extensive margin of caregiving. Further studies using longitudinal datasets with comprehensive information to track individuals over time are necessary to provide more clarity on our results.
7 Conclusion
In summary, this study shows that reducing formal care benefits has a detrimental effect on caregivers’ physical health, while its impact on mental health remains ambiguous. Additionally, these effects are notably gender specific. We underscore the significance of considering caregiver well-being in the evaluation of cost-effectiveness when reducing formal care availability based on care needs. While the economic advantage of providing formal care to recipients with moderate care needs may seem less than the cost, it contributes positively to the well-being of caregivers. Thus, any decline in caregiver well-being should be factored in when assessing the impact of reducing formal care benefits.
Moreover, we suggest that the observed loss in well-being could be a conservative estimate of the potential effects of a reform targeting a broader range of recipients, including those with more severe conditions. Reducing formal care benefits may have even more adverse consequences if future reforms are directed at a wider spectrum of recipients. As such, it is necessary to explore alternative approaches, such as affordability-based methods, to manage public spending on long-term care. In fact, the government has already initiated an affordability-based reform in 2018 by increasing the co-insurance rate for affluent recipients, and future research should assess the impact of this reform.
Lastly, it is important to acknowledge the diversity among caregivers when formulating support policies. Female caregivers are particularly vulnerable to an increased caregiving burden, necessitating protective measures against financial and health-related issues. These policies could encompass respite care, counseling services, and financial assistance.
Notes
The likelihood of being eligible for formal care services upon application appears to be quite high. As demonstrated in Appendix Figure A3, out of 8117 applicants in a city in Tokyo prefecture in 2015, only 71 were found to be ineligible, which accounts for less than 1% of the total applicants. This fraction remained relatively stable over time.
Recipients should pay 100% out-of-pocket if their monthly service use exceeds the upper limit.
For the details of assessment that determines the care-need levels, see Fu, Iizuka, & Noguchi (2023).
1 USD = 116.31 JPY as per the annual closing USD-JPY exchange rate in 2006. The monthly upper limit for SL1 was equivalent to 17.2% of the upper limit for CL5 before the reform and 13.9% afterwards.
It is worth noting that the set of questions from the household questionnaire was posed to all respondents aged six years and older. In other words, the designation of a primary caregiver may not be contingent upon the need for LTC. Our sample concentrated on individuals who were both designated primary caregivers and were concurrently included in the LTC questionnaire. This allows us to ensure the active engagement of these identified primary caregivers in the delivery of LTC.
Unlike Miyawaki et al. (2020), we excluded data from 2016 in the post-policy period to prevent potential confounding effects on the control group from a major reform that took place in 2015. The 2015 reform raised the coinsurance rate from 10% to 20% for recipients with incomes equivalent to the current labor force. This adjustment could have a notable influence on the usage of formal care services among recipients in the control group, particularly those with higher levels of care needs, such as those classified as CL3 and above.
In the previous study by Miyawaki et al. (2020), a selective approach was used to measure caregivers’ well-being, which might limit the understanding of the overall policy impacts. For example, in the assessment of mental health, they used indicators associated with physical health, such as fatigue, insomnia, and appetite loss, rather than directly considering the stress levels reported by caregivers in the survey. Similarly, among the 11 available categories of physical symptoms from the survey, they focused solely on musculoskeletal symptoms, potentially overlooking the multidimensional impacts of caregiving on physical health.
“Systemic symptoms” encompassed indications such as fever, dizziness, and headaches, among others. Symptoms related to the respiratory system, such as nasal congestion and coughing, were categorized under the “respiratory system.” The musculoskeletal system included manifestations such as back pain and arthralgia, while “limb” symptoms were characterized by sensations of numbness or chills in the hands or feet. “Injury” encompassed traumatic occurrences such as bone fractures or lacerations. “Eye and ear” symptoms included vision impairment and tinnitus, while “chest” symptoms were marked by palpitations and chest pain. “Digestive system” symptoms comprised issues such as heartburn, diarrhea, and stomach aches, whereas dental issues and toothaches were subsumed under the “gum” condition. “Skin” issues encompassed symptoms such as rashes and itchy skin, while problems associated with the “urinary tract” were related to urinary complications.
We were unable to conduct the heterogeneity analyses for male in-law caregivers due to a limited sample size (23 individuals).
Due to the repeated cross-sectional nature of the data, we opted not to employ PSM-DD as was done by Miyawaki et al. (2020), as it is unclear whether PSM was adjusted for the repeated cross-sectional nature of the data. Unlike the standard PSM for cross-sectional or longitudinal data, PSM for repeated cross-sectional data should involve three separate matching processes: matching between treatment and control groups before the policy, matching between treatment and control groups after the policy, and matching between pre-policy and post-policy control groups. Furthermore, while PSM can help balance observed treatment-control disparities in cross-sectional or panel data, its effectiveness may be limited in the context of repeated cross-sectional data (Smith and Todd, 2005). It is also important to note that PSM cannot address unobserved systematic treatment-control disparities, which may potentially violate the common trend—a critical assumption for the DD approach to be valid. However, Miyawaki et al. (2020) did not account for unobserved fixed effects in their model.
We replaced \({{\rm{Treat}}}_{{it}}\) in Eq. (1) with \({{\rm{Robust}}}_{{it}}\), where caregivers of CL2–CL5 recipients served as the control group, \({{\rm{Y}}}_{{it}}={\rm{\rho }}{{\rm{Robust}}}_{{it}}{\rm{\times }}{{\rm{Post}}}_{t}+{{\bf{X}}}_{{it}}{\boldsymbol{\sigma }}+{{\boldsymbol{\lambda }}}_{c}+{{\boldsymbol{\lambda }}}_{t}+{{\boldsymbol{\lambda }}}_{p}+{{\boldsymbol{\Lambda }}}_{p}+{\tau }_{{it}}.\) We expected \({\rm{\rho }}\) to be close to\(\,\gamma\) in terms of sign, magnitude, and statistical inference.
We also conducted a placebo test, in which caregivers of CL2 and CL3 recipients were given a placebo treatment. The control group consisted of caregivers of CL4 and CL5 recipients. Appendix Figure B2 summarizes the results. Except for intensive care, we found little difference in well-being between the placebo treatment and the control after the reform.
Given the extensive scope of the outcomes, we conducted a robust multiple-hypothesis testing adjustment to assess the reliability of our results. Appendix Table D1 confirms the robustness of our findings after accounting for this adjustment.
Appendix Figure D1 displays the temporal impacts of the reform on the remaining symptoms and stress factors.
Appendix Table E2 provides insight into the robustness of the results for female, as they retained statistical significance even after undergoing adjustment for multiple-hypothesis testing. However, the statistical significance of the impacts on male caregivers did not withstand the multiple-hypothesis testing, indicating that a cautious approach is warranted when interpreting the findings for male caregivers.
To elaborate, since our study focuses on co-residing caregivers, we are unable to examine the effects of the reform on caregivers who reside separately from recipients. On one hand, non-co-residing caregivers may be more vulnerable to reductions in formal care benefits due to the burden of commuting to provide care, potentially increasing the time constraint. On the other hand, co-residing caregivers may provide more time-elastic care than non-co-residing caregivers, making them more sensitive to the reduction in benefits. Depending on the magnitude of these competing impacts, our findings regarding co-residing informal caregivers may either underestimate or overestimate the overall impact of the reform on informal caregivers.
References
Agree, E. M., & Glaser, K. (2009). Demography of Informal Caregiving. In International Handbook of Population Aging (pp. 647–668). Springer Netherlands. https://doi.org/10.1007/978-1-4020-8356-3_29.
Becker, G. S. (1965). A Theory of the Allocation of Time. The Economic Journal, 75(299), 493–517.
Bom, J., Bakx, P., Schut, F., & Van Doorslaer, E. (2019). The Impact of Informal Caregiving for Older Adults on the Health of Various Types of Caregivers: A Systematic Review. The Gerontologist, 59(5), e629–e642. https://doi.org/10.1093/GERONT/GNY137.
Bonsang, E. (2009). Does informal care from children to their elderly parents substitute for formal care in Europe? Journal of Health Economics, 28(1), 143–154. https://doi.org/10.1016/J.JHEALECO.2008.09.002.
Bremer, P., Challis, D., Hallberg, I. R., Leino-Kilpi, H., Saks, K., Vellas, B., Zwakhalen, S. M. G., & Sauerland, D. (2017). Informal and formal care: Substitutes or complements in care for people with dementia? Empirical evidence for 8 European countries. Health Policy (Amsterdam, Netherlands), 121(6), 613–622. https://doi.org/10.1016/J.HEALTHPOL.2017.03.013.
Brown, R. M., & Brown, S. L. (2014). Informal Caregiving: A Reappraisal of Effects on Caregivers. Social Issues and Policy Review, 8(1), 74–102. https://doi.org/10.1111/sipr.12002.
Campbell, J. C., Ikegami, N., & Gibson, M. J. (2010). Lessons From Public Long-Term Care Insurance In Germany And Japan. Health Affairs, 29(1), 87–95. https://doi.org/10.1377/HLTHAFF.2009.0548.
Carmichael, F., & Charles, S. (2003). The opportunity costs of informal care: does gender matter? Journal of Health Economics, 22(5), 781–803. https://doi.org/10.1016/S0167-6296(03)00044-4.
Cohen, C. A., Colantonio, A., & Vernich, L. (2002). Positive aspects of caregiving: Rounding out the caregiver experience. International Journal of Geriatric Psychiatry, 17(2), 184–188. https://doi.org/10.1002/GPS.561.
Collins, N. L., & Feeney, B. C. (2000). A safe haven: An attachment theory perspective on support seeking and caregiving in intimate relationships. Journal of Personality and Social Psychology, 78(6), 1053–1073. https://doi.org/10.1037/0022-3514.78.6.1053.
Colombo, F., Llena-Nozal, A., Mercier, J., & Tjadens, F. (2011). Help Wanted? Providing and Paying for Long-Term Care. OECD Publishing. https://doi.org/10.1787/9789264097759-en.
De La Maisonneuve, C., & Martins, J. O. (2013). Public spending on health and long-term care: a new set of projections. https://www.oecd-ilibrary.org/content/paper/5k44t7jwwr9x-en?crawler=true.
De Zwart, P. L., Bakx, P., & Van Doorslaer, E. K. A. (2017). Will you still need me, will you still feed me when I’m 64? The health impact of caregiving to one’s spouse. Health Economics, 26, 127–138.
Do, Y. K., Norton, E. C., Stearns, S. C., & Van Houtven, C. H. (2015). Informal care and caregiver’s health. Health economics, 24(2), 224–237.
Dong, J., Pollack, H., & Konetzka, R. T. (2019). Effects of long‐term care setting on spousal health outcomes. Health Services Research, 54(1), 158–166. https://doi.org/10.1111/1475-6773.13053.
Di Novi, C., Jacobs, R., & Migheli, M. (2015). The quality of life of female informal caregivers: from Scandinavia to the Mediterranean Sea. European journal of population, 31, 309–333.
Fu, R., Iizuka, T., & Noguchi, H. (2023). Long-Term Care in Japan. NBER Working Paper, (w31829).
Fu, R., & Noguchi, H. (2019). Moral hazard under zero price policy: evidence from Japanese long-term care claims data. European Journal of Health Economics, 20(6), 785–799. https://doi.org/10.1007/s10198-019-01041-6.
Fu, R., Noguchi, H., Kawamura, A., Takahashi, H., & Tamiya, N. (2017). Spillover effect of Japanese long-term care insurance as an employment promotion policy for family caregivers. Journal of Health Economics, 56. https://doi.org/10.1016/j.jhealeco.2017.09.011.
Gonçalves, J., von Hafe, F., & Filipe, L. (2021). Formal home care use and spousal health outcomes. Social Science & Medicine, 287, 114373 https://doi.org/10.1016/J.SOCSCIMED.2021.114373.
Heitmueller, A., & Inglis, K. (2007). The earnings of informal carers: Wage differentials and opportunity costs. Journal of Health Economics, 26(4), 821–841. https://doi.org/10.1016/J.JHEALECO.2006.12.009.
Ishibashi, T., & Ikegami, N. (2010). Should the provision of home help services be contained?: validation of the new preventive care policy in Japan. BMC Health Services Research, 10, 1–7.
Ito, T., Mori, T., Takahashi, H., Shimafuji, N., Iijima, K., Yoshie, S., & Tamiya, N. (2021). Prevention services via public long-term care insurance can be effective among a specific group of older adults in Japan. BMC Health Services Research, 21, 1–10.
Kumagai, N. (2017). Distinct impacts of high intensity caregiving on caregivers’ mental health and continuation of caregiving. Health Economics Review, 7(1), 1–14. https://doi.org/10.1186/S13561-017-0151-9/TABLES/6.
Lazarus, R. S., & Folkman, S. (1984). Stress, appraisal, and coping. New York: Springer.
Lawrence, R. H., Tennstedt, S. L., & Assmann, S. F. (1998). Quality of the caregiver–care recipient relationship: Does it offset negative consequences of caregiving for family caregivers? Psychology and Aging, 13(1), 150.
Le, D. D. & Ibuka, Y. (2023). Understanding the effects of informal caregiving on health and well-being: Heterogeneity and mechanisms.Social Science & Medicine, 317, 115630.
Marino, V. R., Haley, W. E., & Roth, D. L. (2017). Beyond hedonia: A theoretical reframing of caregiver well-being. Translational Issues in Psychological Science, 3(4), 400–409. https://doi.org/10.1037/TPS0000134.
McEwen, B. S. (1998). Protective and Damaging Effects of Stress Mediators. New England Journal of Medicine, 338(3), 171–179. https://doi.org/10.1056/NEJM199801153380307.
MHLW. (2004). Report on long-term care insurance. https://www.mhlw.go.jp/toukei/saikin/hw/kaigo/service04/kekka3.html.
Ministry of Health, L. and W. (2019). Report on long-term care insurance. https://www.mhlw.go.jp/toukei/list/84-1.html.
Ministry of Health Labour and Welfare. (2014). Results of the Comprehensive survey of living Conditions FY 2013. In Ministry of Health, Labour, and Welfare.
Miyawaki, A., Kobayashi, Y., Noguchi, H., Watanabe, T., Takahashi, H., & Tamiya, N. (2020). Effect of reduced formal care availability on formal/informal care patterns and caregiver health: A quasi-experimental study using the Japanese long-term care insurance reform. BMC Geriatrics, 20(1), 1–11. https://doi.org/10.1186/S12877-020-01588-7/TABLES/3.
Niimi, Y. (2016). The “Costs” of informal care: an analysis of the impact of elderly care on caregivers’ subjective well-being in Japan. Review of Economics of the Household, 14(4), 779–810. https://doi.org/10.1007/S11150-016-9333-1/TABLES/6.
OECD. (2017). Long-term care expenditure. In Health at a Glance 2017: OECD Indicators. OECD Publishing, Paris. https://doi.org/10.1787/health_glance-2017-81-en
Pearlin, L. I. (2010). The life course and the stress process: some conceptual comparisons. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 65B(2), 207–215. https://doi.org/10.1093/GERONB/GBP106.
Pearlin, L., Mullan, J., Semple, S. J., & Skaff, M. M. (1990). Caregiving and the Stress Process: An Overview of Concepts and Their Measures. The Gerontologist, 30(5), 583–594. https://doi.org/10.1093/geront/30.5.583.
Penning, M. J., & Wu, Z. (2016). Caregiver Stress and Mental Health: Impact of Caregiving Relationship and Gender. The Gerontologist, 56(6), 1102–1113. https://doi.org/10.1093/GERONT/GNV038.
Pinquart, M., & Sörensen, S. (2006). Gender Differences in Caregiver Stressors, Social Resources, and Health: An Updated Meta-Analysis. The Journals of Gerontology: Series B, 61(1), P33–P45. https://doi.org/10.1093/GERONB/61.1.P33.
Puhani, P. A. (2012). The treatment effect, the cross difference, and the interaction term in nonlinear “difference-in-differences” models. Economics Letters, 115(1), 85–87. https://doi.org/10.1016/J.ECONLET.2011.11.025.
Ranci, C., & Pavolini, E. (2013). Reforms in Long-Term Care Policies in Europe. New York: Springer. (C. Ranci & E. Pavolini (eds.))10.1007/978-1-4614-4502-9.
Roth, D. L., Fredman, L., & Haley, W. E. (2015). Informal Caregiving and Its Impact on Health: A Reappraisal From Population-Based Studies. The Gerontologist, 55(2), 309–319. https://doi.org/10.1093/geront/gnu177.
Rotter, J. B. (1966). Generalized expectancies for internal versus external control of reinforcement. Psychological Monographs, 80(1), 1–28. http://www.ncbi.nlm.nih.gov/pubmed/5340840.
Ruppanner, L., & Bostean, G. (2014). Who Cares? Caregiver Well-being in Europe. European Sociological Review, 30(5), 655–669. https://doi.org/10.1093/esr/jcu065.
Schmitz, H., & Stroka, M. A. (2013). Health and the double burden of full-time work and informal care provision — Evidence from administrative data. Labour Economics, 24, 305–322. https://doi.org/10.1016/J.LABECO.2013.09.006.
Schmitz, H., & Westphal, M. (2015). Short- and medium-term effects of informal care provision on female caregivers’ health. Journal of Health Economics, 42, 174–185. https://doi.org/10.1016/J.JHEALECO.2015.03.002.
Sharma, N., Chakrabarti, S., & Grover, S. (2016). Gender differences in caregiving among family - caregivers of people with mental illnesses. World Journal of Psychiatry, 6(1), 7–17. https://doi.org/10.5498/wjp.v6.i1.7.
Simes, R. J. (1986). An improved Bonferroni procedure for multiple tests of significance. Biometrika, 73(3), 751–754. https://doi.org/10.1093/BIOMET/73.3.751.
Suanet, B., Van Groenou, M. B., & Van Tilburg, T. (2012). Informal and formal home-care use among older adults in Europe: can cross-national differences be explained by societal context and composition? Ageing and Society, 32(3), 491–515. https://doi.org/10.1017/S0144686X11000390.
Smith, J. A., & Todd, P. E. (2005). Does matching overcome LaLonde’s critique of nonexperimental estimators? Journal of Econometrics, 125(1-2), 305–353.
Tamiya, N., Noguchi, H., Nishi, A., Reich, M. R., Ikegami, N., Hashimoto, H., Shibuya, K., Kawachi, I., & Campbell, J. C. (2011). Population ageing and wellbeing: lessons from Japan’s long-term care insurance policy. The Lancet, 378(9797), 1183–1192. https://doi.org/10.1016/S0140-6736(11)61176-8.
Uccheddu, D., Gauthier, A. H., Steverink, N., & Emery, T. (2019). The pains and reliefs of the transitions into and out of spousal caregiving. A cross-national comparison of the health consequences of caregiving by gender. Social Science and Medicine, 240, 112517. https://doi.org/10.1016/j.socscimed.2019.112517.
Van den Broek, T., & Grundy, E. (2020). Does long-term care coverage shape the impact of informal care-giving on quality of life? A difference-in-difference approach. Ageing & Society, 40(6), 1291–1308.
Van Houtven, C. H., Coe, N. B., & Skira, M. M. (2013). The effect of informal care on work and wages. Journal of Health Economics, 32(1), 240–252. https://doi.org/10.1016/J.JHEALECO.2012.10.006.
Verbakel, E. (2014). Informal caregiving and well-being in Europe: What can ease the negative consequences for caregivers? Journal of European Social Policy, 24(5), 424–441. https://doi.org/10.1177/0958928714543902.
Verbakel, E., Metzelthin, S. F., & Kempen, G. I. J. M. (2016). Caregiving to Older Adults: Determinants of Informal Caregivers’ Subjective Well-being and Formal and Informal Support as Alleviating Conditions. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, gbw047. https://doi.org/10.1093/geronb/gbw047.
Wagner, M., & Brandt, M. (2015). Loneliness among informal caregivers aged 50+. In A. Börsch-Supan, T. Kneip, H. Litwin, M. Myck, & G. Weber (Eds.), Ageing in Europe - Supporting Policies for an Inclusive Society (pp. 179–188). De Gruyter.
Acknowledgements
This paper uses the confidential data provided by the Ministry of Health Labour and Welfare (MHLW) (Approval number: 2020-0727-3). The data can be obtained by applying to the MHLW (https://www.mhlw.go.jp/toukei/sonota/chousahyo.html). The authors were financially supported by the Open Research Area for the Social Sciences program (ORA) of the Japan Society for the Promotion of Science (JPJSJRP20181403). Institutional Review Board approval was not required since the authors used secondary data.
Author contributions
Rong FU conducted the empirical estimations; wrote the main manuscript text; and prepared figures and tables. All authors reviewed the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fu, R., Le, D.D. & Ibuka, Y. The impact of reducing formal care benefits on caregivers’ well-being: evidence from Japan. Rev Econ Household (2024). https://doi.org/10.1007/s11150-024-09699-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11150-024-09699-5