Abstract
Purpose
Measuring health-related quality of life (HRQoL) of children with suspected genetic conditions is important for understanding the effect of interventions such as genomic sequencing (GS). The Pediatric Quality of Life Inventory (PedsQL) is a widely used generic measure of HRQoL in pediatric patients, but its psychometric properties have not yet been evaluated in children undergoing diagnostic GS.
Methods
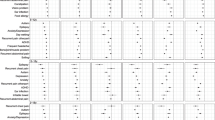
In this cross-sectional study, we surveyed caregivers at the time of their child’s enrollment into GS research studies as part of the Clinical Sequencing Evidence Generating Research (CSER) consortium. To evaluate structural validity of the PedsQL 4.0 Generic Core Scales and PedsQL Infant Scales parent proxy-report versions, we performed a confirmatory factor analysis of the hypothesized factor structure. To evaluate convergent validity, we examined correlations between caregivers’ reports of their child’s health, assessed using the EQ VAS, and PedsQL scores by child age. We conducted linear regression analyses to examine whether age moderated the association between caregiver-reported child health and PedsQL scores. We assessed reliability using Cronbach’s alpha.
Results
We analyzed data for 766 patients across all PedsQL age group versions (1–12 months through 13–18 years). Model fit failed to meet criteria for good fit, even after modification. Neither age group (categorical) nor age (continuous) significantly moderated associations between PedsQL scores and caregiver-reported child health. Cronbach’s alphas indicated satisfactory internal consistency for most PedsQL scales.
Conclusion
The PedsQL Generic Core Scales and Infant Scales may be appropriate to measure HRQoL in pediatric patients with suspected genetic conditions across a wide age range. While we found evidence of acceptable internal consistency and preliminary convergent validity in this sample, there were some potential problems with structural validity and reliability that require further attention.

Similar content being viewed by others
References
Vissers, L. E. L. M., van Nimwegen, K. J. M., Schieving, J. H., Kamsteeg, E.-J., Kleefstra, T., Yntema, H. G., et al. (2017). A clinical utility study of exome sequencing versus conventional genetic testing in pediatric neurology. Genetics in Medicine, 19, 1055. https://doi.org/10.1038/gim.2017.1
Meng, L., Pammi, M., Saronwala, A., Magoulas, P., Ghazi, A. R., Vetrini, F., et al. (2017). Use of exome sequencing for infants in intensive care units: Ascertainment of severe single-gene disorders and effect on medical management. JAMA Pediatrics, 171, e173438. https://doi.org/10.1001/jamapediatrics.2017.3438
Shickh, S., Mighton, C., Uleryk, E., Pechlivanoglou, P., & Bombard, Y. (2021). The clinical utility of exome and genome sequencing across clinical indications: A systematic review. Human Genetics, 140, 1403–1416. https://doi.org/10.1007/s00439-021-02331-x
Pal, D. K. (1996). Quality of life assessment in children: A review of conceptual and methodological issues in multidimensional health status measures. Journal of Epidemiology and Community Health, 50, 391–396. https://doi.org/10.1136/jech.50.4.391
Vivier, P. M., Bernier, J. A., & Starfield, B. (1994). Current approaches to measuring health outcomes in pediatric research. Current Opinion in Pediatrics, 6, 530–537. https://doi.org/10.1097/00008480-199410000-00005
Varni, J. W., Seid, M., & Rode, C. A. (1999). The PedsQL™: Measurement model for the pediatric quality of life inventory. Medical Care, 37, 126–139. https://doi.org/10.1097/00005650-199902000-00003
Smith, H. S., Ferket, B. S., Gelb, B. D., Hindorff, L., Ferar, K. D., Norton, M. E., et al. (2023). Parent-reported clinical utility of pediatric genomic sequencing. Pediatrics, 152, e2022060318. https://doi.org/10.1542/peds.2022-060318
Krantz, I. D., Medne, L., Weatherly, J. M., Wild, K. T., Biswas, S., NICUSeq Study Group, et al. (2021). Effect of whole-genome sequencing on the clinical management of acutely ill infants with suspected genetic disease: A randomized clinical trial. JAMA Pediatrics, 175, 1218–1226. https://doi.org/10.1001/jamapediatrics.2021.3496
Perry, J., Redfield, S., Oza, A., Rouse, S., Stewart, C., Khela, H., et al. (2022). Exome sequencing expands the genetic diagnostic spectrum for pediatric hearing loss. The Laryngoscope. https://doi.org/10.1002/lary.30507
Haviland, I., Daniels, C. I., Greene, C. A., Drew, J., Love-Nichols, J. A., Swanson, L. C., et al. (2023). Genetic diagnosis impacts medical management for pediatric epilepsies. Pediatric Neurology, 138, 71–80. https://doi.org/10.1016/j.pediatrneurol.2022.10.006
Ayres, S., Gallacher, L., Stark, Z., & Brett, G. R. (2019). Genetic counseling in pediatric acute care: Reflections on ultra-rapid genomic diagnoses in neonates. Journal of Genetic Counseling, 28, 273–282. https://doi.org/10.1002/jgc4.1086
Smith, H. S., Swint, J. M., Lalani, S. R., Yamal, J.-M., de Oliveira Otto, M. C., Castellanos, S., et al. (2019). Clinical application of genome and exome sequencing as a diagnostic tool for pediatric patients: A scoping review of the literature. Genetics in Medicine, 21, 3–16. https://doi.org/10.1038/s41436-018-0024-6
Callahan, K. P., Mueller, R., Flibotte, J., Largent, E. A., & Feudtner, C. (2022). Measures of utility among studies of genomic medicine for critically ill infants: A systematic review. JAMA Network Open, 5, e2225980–e2225980. https://doi.org/10.1001/jamanetworkopen.2022.25980
Grosse, S. D., & Khoury, M. J. (2006). What is the clinical utility of genetic testing? Genetics in Medicine, 8, 448–450. https://doi.org/10.1097/01.gim.0000227935.26763.c6
Foster, M. W., Mulvihill, J. J., & Sharp, R. R. (2009). Evaluating the utility of personal genomic information. Genetics in Medicine, 11, 570–574.
Hayeems, R. Z., Luca, S., Ungar, W. J., Venkataramanan, V., Tsiplova, K., Bashir, N. S., et al. (2022). The clinician-reported genetic testing utility InDEx (C-GUIDE): Preliminary evidence of validity and reliability. Genetics in Medicine, 24, 430–438. https://doi.org/10.1016/j.gim.2021.10.005
Hayeems, R. Z., Dimmock, D., Bick, D., Belmont, J. W., Green, R. C., Lanpher, B., et al. (2020). Clinical utility of genomic sequencing: A measurement toolkit. NPJ Genomic Medicine, 5, 1–11.
Green, R. C., Shah, N., Genetti, C. A., Yu, T., Zettler, B., Uveges, M. K., et al. (2023). Actionability of unanticipated monogenic disease risks in newborn genomic screening: Findings from the BabySeq Project. American Journal of Human Genetics, 110, 1034–1045. https://doi.org/10.1016/j.ajhg.2023.05.007
Linder, J. E., Tao, R., Chung, W. K., Kiryluk, K., Liu, C., Weng, C., et al. (2023). Prospective, multi-site study of healthcare utilization after actionable monogenic findings from clinical sequencing. American Journal of Human Genetics, 110, 1950–1958. https://doi.org/10.1016/j.ajhg.2023.10.006
Kohler, J. N., Turbitt, E., Lewis, K. L., Wilfond, B. S., Jamal, L., Peay, H. L., et al. (2017). Defining personal utility in genomics: A Delphi study. Clinical Genetics, 92, 290–297. https://doi.org/10.1111/cge.12998
Smith, H. S., Brothers, K. B., Knight, S. J., Ackerman, S. L., Rini, C., Veenstra, D. L., et al. (2021). Conceptualization of utility in translational clinical genomics research. American Journal of Human Genetics. https://doi.org/10.1016/j.ajhg.2021.08.013
Smith, H. S., Morain, S. R., Robinson, J. O., Canfield, I., Malek, J., Rubanovich, C. K., et al. (2022). Perceived utility of genomic sequencing: Qualitative analysis and synthesis of a conceptual model to inform patient-centered instrument development. Patient - Patient-Centered Outcomes Research, 15, 317–328. https://doi.org/10.1007/s40271-021-00558-4
Turbitt, E., Kohler, J. N., Angelo, F., Miller, I. M., Lewis, K. L., Goddard, K. A. B., et al. (2023). The PrU: Development and validation of a measure to assess personal utility of genomic results. Genetics in Medicine, 25, 100356. https://doi.org/10.1016/j.gim.2022.12.003
Buchanan, J., & Wordsworth, S. (2019). Evaluating the outcomes associated with genomic sequencing: A roadmap for future research. PharmacoEconomics - Open, 3, 129–132. https://doi.org/10.1007/s41669-018-0101-4
Ow, N., & Mayo, N. E. (2020). Health-related quality of life scores of typically developing children and adolescents around the world: A meta-analysis with meta-regression. Quality of Life Research, 29, 2311–2332. https://doi.org/10.1007/s11136-020-02519-0
Pinquart, M. (2020). Health-related quality of life of young people with and without chronic conditions. Journal of Pediatric Psychology, 45, 780–792. https://doi.org/10.1093/jpepsy/jsaa052
Varni, J. W., Seid, M., & Kurtin, P. S. (2001). PedsQLTM 4.0: Reliability and validity of the pediatric quality of life InventoryTM Version 4.0 generic core scales in healthy and patient populations. Medical Care, 39, 800–812. https://doi.org/10.1097/00005650-200108000-00006
Varni, J. W., Limbers, C. A., Neighbors, K., Schulz, K., Lieu, J. E. C., Heffer, R. W., et al. (2011). The PedsQL™ Infant Scales: Feasibility, internal consistency reliability, and validity in healthy and ill infants. Quality of Life Research, 20, 45–55. https://doi.org/10.1007/s11136-010-9730-5
Desai, A. D., Zhou, C., Stanford, S., Haaland, W., Varni, J. W., & Mangione-Smith, R. M. (2014). Validity and responsiveness of the pediatric quality of life inventory (PedsQL) 4.0 generic core scales in the pediatric inpatient setting. JAMA Pediatrics, 168, 1114. https://doi.org/10.1001/jamapediatrics.2014.1600
Varni, J. W., Burwinkle, T. M., Seid, M., & Skarr, D. The PedsQL* 4.0 as a pediatric population health measure: Feasibility, reliability, and validity. Ambul Pediatr n.d.
Varni, J. W., Limbers, C. A., & Burwinkle, T. M. (2007). How young can children reliably and validly self-report their health-related quality of life? An analysis of 8,591 children across age subgroups with the PedsQLTM 4.0 Generic Core Scales. Health and Quality of Life Outcomes, 5, 1. https://doi.org/10.1186/1477-7525-5-1
Varni, J. W., Limbers, C. A., & Burwinkle, T. M. (2007). Parent proxy-report of their children’s health-related quality of life: An analysis of 13,878 parents’ reliability and validity across age subgroups using the PedsQLTM 4.0 Generic Core Scales. Health and Quality of Life Outcomes, 5, 2. https://doi.org/10.1186/1477-7525-5-2
Splinter, K., Niemi, A.-K., Cox, R., Platt, J., Shah, M., Enns, G. M., et al. (2016). Impaired health-related quality of life in children and families affected by methylmalonic acidemia. Journal of Genetic Counseling, 25, 936–944.
Vanz, A. P., van de Sande, L. J., Pinheiro, B., Zambrano, M., Brizola, E., da Rocha, N. S., et al. (2018). Health-related quality of life of children and adolescents with osteogenesis imperfecta: A cross-sectional study using PedsQL™. BMC Pediatrics, 18, 95.
Needham, M., Packman, W., Quinn, N., Rappoport, M., Aoki, C., Bostrom, A., et al. (2015). Health-related quality of life in patients with MPS II. Journal of Genetic Counseling, 24, 635–644. https://doi.org/10.1007/s10897-014-9791-7
Murali, C. N., Lalani, S. R., Azamian, M. S., Miyake, C. Y., & Smith, H. S. (2022). Quality of life, illness perceptions, and parental lived experiences in TANGO2-related metabolic encephalopathy and arrhythmias. European Journal of Human Genetics, 30, 1044–1050. https://doi.org/10.1038/s41431-022-01127-5
Nutakki, K., Varni, J. W., & Swigonski, N. L. (2018). PedsQL Neurofibromatosis Type 1 Module for children, adolescents and young adults: Feasibility, reliability, and validity. Journal of Neuro-oncology, 137, 337–347. https://doi.org/10.1007/s11060-017-2723-2
Iannaccone, S. T., Hynan, L. S., Morton, A., Buchanan, R., Limbers, C. A., & Varni, J. W. (2009). The PedsQL™ in pediatric patients with spinal muscular atrophy: Feasibility, reliability, and validity of the Pediatric Quality of Life Inventory™ Generic Core Scales and Neuromuscular Module. Neuromuscular Disorders, 19, 805–812. https://doi.org/10.1016/j.nmd.2009.09.009
Uzark, K., King, E., Cripe, L., Spicer, R., Sage, J., Kinnett, K., et al. (2012). Health-related quality of life in children and adolescents with Duchenne muscular dystrophy. Pediatrics, 130, e1559-1566. https://doi.org/10.1542/peds.2012-0858
Kourtidou, S., Slee, A. E., Bruce, M. E., Wren, H., Mangione-Smith, R. M., & Portman, M. A. (2018). Kawasaki disease substantially impacts health-related quality of life. Journal of Pediatrics, 193, 155-163.e5. https://doi.org/10.1016/j.jpeds.2017.09.070
Amendola, L. M., Berg, J. S., Horowitz, C. R., Angelo, F., Bensen, J. T., Biesecker, B. B., et al. (2018). The clinical sequencing evidence-generating research consortium: Integrating genomic sequencing in diverse and medically underserved populations. American Journal of Human Genetics, 103, 319–327. https://doi.org/10.1016/j.ajhg.2018.08.007
Goddard, K. A., Angelo, F. A., Ackerman, S. L., Berg, J. S., Biesecker, B. B., Danila, M. I., et al. (2020). Lessons learned about harmonizing survey measures for the CSER consortium. Journal of Clinical and Translational Science, 4(6), 537–546. https://doi.org/10.1017/cts.2020.41
Staley, B. S., Milko, L. V., Waltz, M., Griesemer, I., Mollison, L., Grant, T. L., et al. (2021). Evaluating the clinical utility of early exome sequencing in diverse pediatric outpatient populations in the North Carolina Clinical Genomic Evaluation of Next-generation Exome Sequencing (NCGENES) 2 study: A randomized controlled trial. Trials, 22, 395. https://doi.org/10.1186/s13063-021-05341-2
Odgis, J. A., Gallagher, K. M., Suckiel, S. A., Donohue, K. E., Ramos, M. A., Kelly, N. R., et al. (2021). The NYCKidSeq project: Study protocol for a randomized controlled trial incorporating genomics into the clinical care of diverse New York City children. Trials, 22, 56. https://doi.org/10.1186/s13063-020-04953-4
Find Shortage Areas by Address n.d. https://data.hrsa.gov/tools/shortage-area/by-address (accessed March 4, 2023).
Wille, N., Badia, X., Bonsel, G., Burström, K., Cavrini, G., Devlin, N., et al. (2010). Development of the EQ-5D-Y: A child-friendly version of the EQ-5D. Quality of Life Research, 19, 875–886.
Bentler, P. M. (1980). Multivariate analysis with latent variables: Causal modeling. Annual Review of Psychology, 31, 419–456.
Kline, R. B. (1998). Structural equation modeling. N Y Guilford.
Hu, L., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6, 1–55.
Tabachnick, B. G., Fidell, L. S., & Ullman, J. B. (2013). Using multivariate statistics (Vol. 6). Pearson.
American Educational Research Association, American Psychological Association, National Council on Measurement in Education. (2014). Standards for educational and psychological testing. American Educational Research Association.
Cohen, J. (1992). A power primer. Psychological Bulletin, 112, 155–159. https://doi.org/10.1037/0033-2909.112.1.155
Cronbach, L. J. (1951). Coefficient alpha and the internal structure of tests. Psychometrika, 16, 297–334.
Jones, K. M., O’Grady, G., Rodrigues, M. J., Ranta, A., Roxburgh, R. H., Love, D. R., et al. (2018). Impacts for children living with genetic muscle disorders and their parents: Findings from a population-based study. Journal of Neuromuscular Diseases, 5, 341–352. https://doi.org/10.3233/JND-170287
Smith, H., Hickingbotham, M. R., Deloge, R. B., Khan, F., & Hanmer, J. (2023). PCR128 measurement of health-related quality of life in pediatric genetic conditions: A scoping review. Value Health, 26, S335. https://doi.org/10.1016/j.jval.2023.03.1904
Brown, T. A. (2006). Confirmatory factor analysis for applied research. The Guilford Press.
Bollen, K., & Lennox, R. (1991). Conventional wisdom on measurement: A structural equation perspective. Psychological Bulletin, 110, 305–314. https://doi.org/10.1037/0033-2909.110.2.305
Kelly, C. B., Soley-Bori, M., Lingam, R., Forman, J., Cecil, L., Newham, J., et al. (2023). Mapping PedsQL™ scores to CHU9D utility weights for children with chronic conditions in a multi-ethnic and deprived metropolitan population. Quality of Life Research, 32, 1909–1923. https://doi.org/10.1007/s11136-023-03359-4
Jiao, B., Hankins, J. S., Devine, B., Barton, M., Bender, M., & Basu, A. (2022). Application of validated mapping algorithms between generic PedsQL scores and utility values to individuals with sickle cell disease. Quality of Life Research, 31, 2729–2738. https://doi.org/10.1007/s11136-022-03167-2
Shafie, A. A., Chhabra, I. K., Wong, J. H. Y., & Mohammed, N. S. (2021). Mapping PedsQL™ Generic Core Scales to EQ-5D-3L utility scores in transfusion-dependent thalassemia patients. The European Journal of Health Economics, 22, 735–747. https://doi.org/10.1007/s10198-021-01287-z
Xiong, X., Dalziel, K., Huang, L., Mulhern, B., & Carvalho, N. (2023). How do common conditions impact health-related quality of life for children? Providing guidance for validating pediatric preference-based measures. Health and Quality of Life Outcomes, 21, 8. https://doi.org/10.1186/s12955-023-02091-4
Funding
The Clinical Sequencing Evidence-Generating Research (CSER) consortium is funded by the National Human Genome Research Institute (NHGRI) with co-funding from the National Institute on Minority Health and Health Disparities (NIMHD) and the National Cancer Institute (NCI), supported by U01HG006487 (UNC), U01HG007292 (KPNW), U01HG009610 (Mt Sinai), U01HG006485 (Baylor), U01HG009599 (UCSF), U01HG007301 (HudsonAlpha), and U24HG007307 (Coordinating Center). HSS is supported by an NHGRI career development award (K99HG011491). The contents of this paper are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. More information about CSER can be found at https://cser-consortium.org/.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data analysis was performed by ML. The first draft of the manuscript was written by HSS and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Smith reports receiving consulting income from Illumina, Inc. unrelated to this work. The other authors declare no competing interests.
Ethics approval
Institutional Review Board approval was obtained for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Smith, H.S., Leo, M., Goddard, K. et al. Measuring health-related quality of life in children with suspected genetic conditions: validation of the PedsQL proxy-report versions. Qual Life Res (2024). https://doi.org/10.1007/s11136-024-03623-1
Accepted:
Published:
DOI: https://doi.org/10.1007/s11136-024-03623-1