Abstract
Background
Only one pilot value set (UK) is currently available for the EQ Health and Wellbeing Instrument short version (EQ-HWB-S). As an alternative to preference-weighted scoring, we examined whether a level summary score (LSS) is appropriate for the EQ-HWB-S using Mokken scaling analyses.
Methods
Data from patients, carers and the general population collected during the developmental phase of the EQ-HWB-S in Australia, US and UK were used, noting 3 of 9 items have since undergone revision. EQ-HWB-S data fit was examined using R package Mokken scaling’s monotone homogeneity model, utilizing the automated item selection procedure (AISP) as well as Loevinger’s scaling coefficients for items and the scale (HS). Manifest monotonicity was assessed by examining whether the cumulative probability for responses at or above each response level did not decrease across the summary score.
Results
EQ-HWB-S data were available for 3340 respondents: US = 903, Australia = 514 and UK = 1923. Mean age was 50 ± 18 and 1841 (55%) were female. AISP placed all 9 items of the EQ-HWB-S on a single scale when the lower bound was set to < 0.448. Strong scalability (HS = 0.561) was found for the EQ-HWB-S as a single scale. Stronger scales were formed by separating the psychosocial items (n = 6, HS = 0.683) and physical sensation items (n = 3, HS = 0.713). No violations of monotonicity were found except for the items mobility and daily activities for the subgroups with long-term conditions and UK subjects, respectively.
Discussion
As EQ-HWB-S items formed a strong scale and subscales based on Mokken analysis, LSS is a promising weighting-free approach to scoring.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The EQ health and wellbeing (EQ-HWB) is a self-reported measure intended to inform resource allocation across health and social care settings [1,2,3]. Its development was motivated by the need to include domains relevant to well-being in the context of health and social care which may not be covered by existing health-related quality of life measures [2,3,4,5]. The instrument was developed using qualitative and quantitative methods and its short version, the EQ-HWB-S, comprises 9 items. Preference-based scoring, which involve eliciting values from country-specific populations [6], are under development for the EQ-HWB-S but currently, only a pilot preference value set (for UK [7]) is available and there is no non-preference based scoring.
A simple method to provide a summary score for the EQ suite of instruments is to sum the ordinal response levels of items [8]. This approach, sometimes called the “equally weighted” score [9], “unweighted” scoring approach [10, 11], or “level sum score” (LSS) [12], can be applied when preference-based scoring is not possible or available. The appeal of the LSS is its simplicity and that it is the same across countries and populations [13, 14]. Previous investigations revealed substantial agreement and similar psychometric properties between the LSS and utility weighted scores [9,10,11]. A recent paper found support for ordering respondents on the EQ-5D-5L using the LSS [8]. Whether the LSS is an appropriate method for scoring the EQ-HWB-S remains unclear.
Item response theory (IRT) is a family of models that assess the relationship between a latent (not directly observable) construct (theta θ) and the manifest (observable) response patterns of a set of items. The probability of endorsing a particular response level on items of a scale is dependent on the respondent’s level of θ. Non-parametric item response theory (NP-IRT) approaches do not make strict assumptions about the patterns of response probabilities [15]. Mokken scaling, the most well-known NP-IRT approach, does not estimate the exact level of θ but rather examines whether respondents can be ordered along the θ, and whether items can be ordered using the mean item scores given the response patterns of a dataset [15, 16]. If the LSS is a proxy for θ, then ordering of respondents along the LSS should reflect the ordering of persons along θ.
The aim of this study was to investigate if EQ-HWB-S data fits Mokken scaling models, which would support the use of the LSS. The LSS would allow for scoring of the EQ-HWB-S when no preference-based value set is available and also for comparisons across populations.
Methods
The EQ-HWB-S
The EQ-HWB-S is a short version of the 25-item EQ-HWB [17, 18] and comprises 9 items covering mobility, daily activities, coping (control), concentrating/thinking, anxiety, depression (sad), loneliness, fatigue, and pain. Response levels indicate frequency, level of difficulty, or severity: all use five-level ordinal response format covering the same recall period (the last 7 days), making the instruments ideal for LSS and Mokken scaling approaches [1, 4, 5]. In lieu of a set of commonly agreed upon labels for the items, we use abbreviations in this manuscript as described in Appendix B.
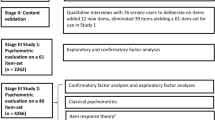
EQ-HWB psychometric study
Secondary data was available: as part of the development of the EQ-HWB instruments, a large multi-country psychometric study was conducted to test more than 60 candidate items [3, 4]. We limited these analyses to the English language version of the EQ-HWB-S—data from Australia (AUS), United Kingdom (UK) and the United States of America (US)—in order to limit cross-linguistic differences which can affect measurement properties. The psychometric survey was conducted using both face-to-face and online methods, and described in detail in Peasgood et al. [3]. The general population, carer, and specific patient groups were recruited for each country: US cancer patients, UK patients with cancer, depression, diabetes, arthritis, heart conditions, irritable bowel syndrome/Crohn’s disease, and AUS patients with mental and physical health problems and/or those experiencing pain. Respondents completed a battery of health status, well-being, social care measures, alongside the EQ-HWB item pool.
Because no new data were collected for this study, no additional ethical approval was required beyond the approvals gained in each country for the data collection. Permission to share the data with research groups was given in the initial consent obtained during the psychometric study. Data management was handled in Microsoft Excel while statistical analyses were conducted using Stata SE 16 [19] and the statistical language and environment R [20]. Mokken analyses were conducted using van der Ark’s package “mokken” [21, 22] and the corresponding R script is available in Appendix A.
Descriptive analysis
Simple descriptive analysis was conducted on socio-demographic and health-related variables avaliable in the dataset. We used mean and standard deviations to describe continuous, and count and percentages to describe categorical variables. Descriptive analysis was conducted for the complete data set as well as stratified by countries. The EQ-5D-5L was scored using both the LSS approach [8] and using the US value set [23].
Item preparation
Some candidate items included in the EQ-HWB psychometric study were further refined after the study concluded. Therefore, several items did not match the exact wording of the current (2023) experimental version of the EQ-HWB-S (See Monteiro et al. Table 1, for current item wording [24]). Three “control” items were included in the psychometric study: the negative control item without examples exhibited the best performance and was selected for analysis. Three EQ-HWB-S items underwent substantive revisions and therefore no equivalent item was included in the psychometric study: (1) mobility inside/outside, (2) concentrating/thinking, and (3) feeling sad/depressed (the text of these items as worded for the psychometric study and their wording in the current version of the EQ-HWB-S can be found in Appendix C).
The psychometric study included items about difficulty “to get around” (1) inside and (2) outside, as well as items about problems with (3) concentrating and (4) thinking clearly. Using a similar strategy as earlier work that combined two items into a single dimension [25], we created the composite items “mobility” and “concentrating/thinking” by combining items (1) and (2), and items (3) and (4), respectively. Responses of the pairs of items were used to create new composite variables as detailed in Fig. 1. The four original items as well as the two composites were tested in models.
The UK and US psychometric studies contained an item asking about sadness but not depression: therefore a composite “feeling sad/depressed” could not be created. However, a “depression” item (using the same response format as the “sad” item) was included in the AUS study as it was found to have face validity in previous qualitative work. A subgroup analysis specifically addressing the composite “feeling sad/depressed” item was carried out using the AUS dataset.
Mokken scale analysis
Mokken scaling is a set of non-parametric item response theory-based tools, consisting mainly of two nested models that can elucidate the ordinal location of respondents and items along a latent trait θ: the monotone homogeneity (MHM) and double monotonicity (DMM) models [26, 27]. Individuals are ordered according to the unweighted summary scores of their responses and items are ordered according to mean scores [15, 26, 27]. The polytomous MHM, which test model assumptions at the item and at the rating scale levels, was used [28, 29].
The monotone homogeneity model (MHM) and scalability
The three assumptions of the MHM are:
-
1.
Unidimensionality (items within the scale measure the same underlying latent trait);
-
2.
Local independence (correlations between responses to scale items are influenced only by the level of θ); and
-
3.
Monotonicity (the probability of endorsing particular response levels is monotonically non-decreasing as θ increases).
Loevinger’s homogeneity coefficients H were used to assess scalability of the EQ-HWB-S items. We examined H on the item (Hi) and scale (HS) levels. Where the ‘rest score’ was the summary score minus the score of the item of interest, Hi was the normed covariance between item and rest scores while HS was the weighted mean of Hi [15, 21]. The closer Hi is to 1, the better an item can discriminate subjects along θ within a scale. Negative Hi indicates a violation of MHM. The commonly accepted rules of thumb for HS were used: HS < 0.3 was unacceptable, HS 0.3–0.4 indicated a weak scale, HS 0.4–0.5 was interpreted as moderate and HS ≥ 0.5 as strong ([30], pp. 60–61).
Automated item selection procedure (AISP) is a standard feature of the R package ‘mokken’ which identifies items that order persons well in a scale or scales [21]. Although the lower bound of Hi > 0.3 has been suggested for accepting items within a scale, Sijtsma and van der Ark suggested exploring different lower bound values smaller and larger than 0.3 [15, 21]. We executed AISP 12 times with the lower bound set between 0.1 and 0.6, increasing in steps of 0.05 (results are presented in steps of 0.1). The level of Hi at which one scale was no longer appropriate was identified by adjusting the lower bound using steps of 0.001. For this analysis, we made no assumptions about the structure of the EQ-HWB (i.e. if items belonged to different subscales or if all items can be scaled together).
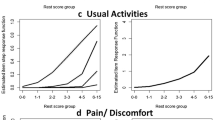
Monotonicity is the property that as the level of the latent trait θ increases, the probability for endorsing at least a certain response level in an item does not decrease (i.e. the probability either remains stable or increases) [26, 27]. Latent monotonicity generally implies manifest monotonicity, which is observable in the data [21]. Manifest monotonicity was assessed by examining whether the cumulative probability for an item-level rating at or above each item-level rating was not decreasing as rest score increased (as defined by rest-score groups). Rest score groups were created automatically based on minimum sample size requirements for each group and only violations greater than the default minimum (minvi > 0.03) were reported [21, 22]. Item step response functions (ISRFs) plot the probability for endorsing a response level or higher across the latent variable and the item response function (IRF) for polytomous items is the sum of items’ ISRFs. IRFs were visually inspected for monotonicity.
Invariant item ordering
The DMM model has the additional assumption that the IRF/ISRF of items do not intersect and is generally not meaningful for scales with polytomous items [31]. Instead of examining DMM, we assessed manifest invariant item ordering (MIIO) as suggested by Ligtvoet et al. [32, 33]. If items can be ordered along θ, then that order can facilitate interpretations for the EQ-HWB-S LSS [15, 21, 22, 31]. MIIO was implemented in the R package “mokken” using the check.iio function which ordered items by their conditional mean scores and checked each item pair for violations of ordering in rest score groups. Violations exceeding the default minimum value (number of ISRFs times 0.03) are reported [22, 33]. We also examined coefficient HT which indicated the degree to which the sample data followed item ordering. The rules of thumb for HT were used: HT < 0.3 as items cannot be ordered, HT 0.3 to 0.4 as low, HT 0.4 to 0.5 as accurate and HT > 0.5 as highly accurate [33].
Exploratory factor analysis (EFA)
While not the focus of this study, EFA was undertaken to support the dimensional structure identified by AISP. EFA was conducted using the principal-factor method and oblique (oblimin) rotation. We also examined the standardized residuals of item-pair correlations.
Known group analysis
Scales that demonstrated sufficient scaling properties were examined across subgroups hypothesized to differ in their level of health and well-being: being a carer and having a long-term illness. The LSS was calculated by assigning a numerical value to each response level (1 for least severe to 5 for the most severe response), and these are summed across the items of the scales. The scales were transformed into a 0 to100 score to allow for comparability across scales as well as with the EQ VAS. The LSS were compared across these subgroups using non-parametric rank-sum tests. Multivariate linear regression was used to examine these variables controlling for age, gender and race.
Robustness of results
All scaling analyses were stratified by country, carer status, having a long-term condition, gender, and age groups. The sample size of all subgroups exceeded n = 500, therefore the standard rules for determining rest-score groups were consistent.
Results
In total, 3340 respondents were included in the psychometric study from the US (n = 903), AUS (n = 514) and the UK (n = 1923). Just over half were women and the average age was 50 years (Table 1). The majority (73.5%) self-reported having one or more long-term condition(s). The average EQ VAS (66.55) was low as compared to general population norms [34,35,36]; nearly 30% self-identified as a carer.
AISP and monotonicity
Table 2 shows the AISP results with the lower bound set from 0.1 to 0.6. When the lower bound was set at 0.448, the physical items (n = 3) and psychosocial items (n = 6) were placed on different scales (Table 2). We tested AISP using the items get around inside, get around outside, concentrating and thinking clearly as individual (non-composite) items, and results did not substantively differ from AISP that used the composite items. Therefore, we used the composite items in further analyses.
When the EQ-HWB-S was modeled as a single scale, its HS indicated a strong scale at 0.561. The items “pain severity”, “daily activities” and “mobility” were moderately scalable (Hi 0.396–0.496) while the rest of the items were strongly scalable (Hi 0.590–0.626). When modeled as two subscales, the physical (HS = 0.683) and psychosocial (HS = 0.713) components had stronger scalability and strong Hi for all items (Table 3).
No violations of monotonicity were identified: Crit values of all items were zero, showing no misfit of the MHM. We used selected item-pair results from the ‘check.restscore’ function to visualize the IRF of multiple items in one figure (Fig. 2). The IRF figures for the EQ-HWB-S subscales visually illustrate that as the rest score increased, the sum of items’ ISRFs did not decrease. The full set of ISRF and IRF figures available in Appendix D.
Fit of MIIO
As a single scale, violations of MIIO were observed for every item, with backward item selection removing the No Control (7 violations, Crit 245) and Pain (16 violations, Crit 385) items (Table 3). No violations were observed for the psychosocial subscale but violations were found for all items of the physical subscale, seemingly due to the Pain item (2 violations, Crit 322). HT indicated that items could not be ordered or the order to have low accuracy for all scales and subgroups (Table 4).
Stratified analysis across subgroups
Scaling coefficients were strong to very strong and did not differ substantively across most of the sub-populations (country, gender, age categories, having a self-reported long-term health condition, being a carer, Table 4).
As a single scale, statistically significant violations of monotonicity were found for those with long-term conditions (mobility), and the UK population (mobility and daily activities), indicating that those items did not discriminate well for those sub-populations. No violations of monotonicity were found for the subscales across all subgroups. See Appendices E1 and E2 for detailed monotonicity results.
In terms of MIIO, the items of the single scale for those without a long-term condition and the physical subscale for subgroups US, AUS, those without a long-term condition and aged 51 to 65 could be ordered but with low accuracy. Only the single scale for the subgroup aged ≤ 35 had an HT larger than 0.4, indicating moderate accuracy of item order.
Lastly, we used the Australian data to examine the items “feel sad” and “feel depressed”: the items were combined in the same way as concentrating/thinking and mobility inside/outside. Models using the composite sad/depressed item were similar to models using the sad item, with slightly better scaling properties for the combined item.
EFA results
Eigenvalues were larger than 1 for two factors. With an Eigenvalue value of 4.80, a dominant first factor was extracted while the Eigenvalue for factor 2 was just over the threshold of 1.0 (Appendix F). Standardized residual correlations tended to be large for item pairs that include the physical items for the 1-factor solution, while all but one (item pair “pain” and “exhausted”) standardized residuals were adequately small for the 2-factor solution.
Descriptive analysis of the EQ-HWB-S LSS
The reliability was excellent for the single scale and psychosocial subscale (alpha and lambda > 0.9) and good for the physical subscale (alpha and lambda > 0.8). The LSS was calculated for all 9 items of the EQ-HWB-S, the 6 psychosocial items and the 3 physical sensation items: all were moderately correlated with EQ VAS with rho of − 0.55 to − 0.62 (Fig. 3). Distribution of items responses and scale/subscale scores did not reveal problematic skews or irregular response patterns.
Only 176 (5.41%) respondents reported the lowest score (or no problems on all items), at the scale level, while 346 (10.53%) reported the lowest score for the psychosocial subscale and 676 (20.54%) for the physical sensations subscale. No respondents reported the highest possible score on the full EQ-HWB-S LSS while 79 (2.40%) reported the highest score on the psychosocial subscale and 3 (0.09%) on the physical sensations subscale. Of those reporting the top score (11111) on the EQ-5D-5L (589, 17.85%), 159 (27.27%) also reported the lowest EQ-HWB-S, 188 (32.14%) psychosocial, and 415 (71.06%) physical sensations LSS, showing a similarity between the physical subscale and the EQ-5D-5L. Of those without a long-term condition, 110 (12.64%) reported the lowest score for the overall LSS and 156 (17.91%) on the psychosocial subscale. However, 383 (43.87%) reported the lowest score on the physical sensations subscale.
The differences in LSS across carers/non-carers, those with and those without long-term conditions were statistically significant (Table 5) with higher full scale and subscales scores (reporting more symptoms and problems) for those who are carers and those with long-term condition(s). These results did not differ substantively across country subgroups (Fig. 4) nor after adjusting for age, gender and race (results not shown).
Discussion
Items of the EQ-HWB-S formed a strong Mokken scale, giving support for use of LSS either at the overall scale or subscale levels. Scalability was strong both for the single scale and the two subscales (6 psychosocial and 3 physical items). No violations of manifest monotonicity were found for the combined datasets, suggesting that the LSS ordered respondents along the latent trait. Therefore, the LSS of the EQ-HWB-S, scale or subscales, can generally order respondents along the latent trait: as θ increases, respondents are more likely to choose increasingly more severe response levels. These results empirically demonstrate that the summary score ordered respondents by their levels of health and well-being. Scaling results were robust across sub-populations (not weaker for healthier subgroups as previously found for the EQ-5D-5L [8]). Overall, scalability results are comparable with previous Mokken investigations of the EQ-5D-5L and the SF-36 [8, 37].
Although no violations of monotonicity were found for subscales across all investigated subgroups, violations were identified for the single scale for sub-populations, showing some items (mobility, daily activities) to not discriminate well for respondents from the UK and those with a long-term health condition. Items could not be ordered along the LSS of these scales.
The early development phases of the EQ-HWB included qualitative research and stakeholder input [2, 5] which largely informed the first psychometric investigations and theoretical dimensional structure of candidate items (see Peasgood et al. for a full exploration of that dimensional structure [1, 3]). While the theory driven model informs the conceptual model for the EQ-HWB, our goal was to provide support for a pragmatic method of summarizing the short-form using a data-driven approach. When the theoretical dimensional structure was not imposed on the data, EFA of the full set of 60 + EQ-HWB candidate items identified only three factors [3], which is similar to our finding that the 9-item instrument can be described using two subscales. This, along with the sufficiently large sample size and robustness of results across subgroups of our study lends confidence that the strong scalability was not a spurious finding. However, AISP may yield a dimensionality structure differing from more conventional techniques, such as EFA: a simulation study found that AISP may not adequately identify appropriate number of dimensions when the factors are strongly correlated [38].
Adding EFA in this investigation provides additional support for the dimensionality as EFA and AISP revealed similar structures in the data: a two-factor solution with a physical and a psychosocial domain had the strongest scalability and most reasonable residual correlation results, and therefore would best describe the structure of the 9 items. Yet, given the dominant first factor (based on eigenvalue, factor loadings and scalability results), adopting a simpler solution for scoring the 9 items may be acceptable. These results may indicate a second-order structure, with a physical and a psychosocial domain both belonging to an overall “well-being” scale. New methods were recently developed to test multidimensionality and higher-order monotone factor models [39]. However, this new methodology has only been developed for binary data, needs further refinement and testing, and is not yet available in software. Clarifying this higher-order structure should be conducted in future studies.
We interpret the results of the Mokken analysis and supporting EFA that using the physical and psychosocial subscales would best reflect the structure underlying the EQ-HWB-S, while using a single score would also be acceptable. Using subscales may be more sensitive to specific patient populations and interventions. Practically, a single score is a powerful generic measure which allows for comparison across patient groups, but loses dimension specificity and interpreting at the subscale level. The physical subscale has slightly poorer scalability and MIIO results than the psychosocial subscale.
Although we were limited in known group comparisons as the dataset was not originally collected for such analyses, we were able to show the EQ-HWB-S scale and subscales differentiated across important subgroups such as those with and without long-term illness. Although scores were statistically different across age groups, older age groups tended to have better EQ-HWB-S scores than younger age groups, as was the case for the EQ-5D-5L health profile and EQ VAS. The counterintuitive results found for age reflect some other recent findings in population level surveys [40, 41].
While we found preliminary support for an LSS approach based on empirical analysis of EQ-HWB-S data, the original scale is conceptually multidimensional and an analysis including additional items (e.g. from other measures of well-being) would provide greater clarity on scalability. Further research is needed as more data of the EQ-HWB become available. Another limitation of this study is that the datasets did not contain the similar wordings to the current experimental EQ-HWB-S instrument for three items: the analysis must be repeated using the most recent version of the EQ-HWB to obtain a more accurate assessment of scaling properties of the instrument. This is especially true for the “sad” item as Australia was the only sample which had sufficient data to examine the combined sad/depressed item. A third limitation is that only English versions of the EQ-HWB-S were analyzed: non-English EQ-HWB versions were included as a part of the psychometric study and extending these analyses to other languages and countries would be necessary. Lastly, given the strong scalability findings for the EQ-HWB (with items conceptually measuring different concepts), it is possible that similar groupings of health and well-being domains were observed as the survey sampled particular condition and population groups. This pattern (and the appropriateness of using the LSS) may differ for other patient populations. These results should be confirmed in a broader set of patient populations to examine whether two subscales for health and well-being can be justified more broadly.
Conclusion
LSS is a promising approach to scoring the psychosocial and physical subscales of the EQ-HWB-S. However, a study including a more representative sample and using the most up-to-date version of the EQ-HWB-S items is needed to further support LSS for the EQ-HWB-S.
Data availability
Contact the primary author regarding data use/data sharing.
References
Peasgood, T., Mukuria, C., Carlton, J., Connell, J., Devlin, N., Jones, K., Lovett, R., Naidoo, B., Rand, S., Rejon-Parrilla, J. C., Rowen, D., Tsuchiya, A., & Brazier, J. (2021). What is the best approach to adopt for identifying the domains for a new measure of health, social care and carer-related quality of life to measure quality-adjusted life years? Application to the development of the EQ-HWB? The European Journal of Health Economics. https://doi.org/10.1007/s10198-021-01306-z
Mukuria, C., Connell, J., Carlton, J., Peasgood, T., Scope, A., Clowes, M., Rand, S., Jones, K., & Brazier, J. (2022). Qualitative review on domains of quality of life important for patients, social care users, and informal carers to inform the development of the EQ health and wellbeing. Value in Health., 25, 492.
Peasgood, T., Mukuria, C., Brazier, J., Marten, O., Kreimeier, S., Luo, N., Mulhern, B., Greiner, W., Pickard, A. S., Augustovski, F., Engel, L., Gibbons, L., Yang, Z., Monteiro, A. L., Kuharic, M., Belizan, M., & Bjørner, J. (2022). Developing a new generic health and wellbeing measure: psychometric survey results for the EQ health and wellbeing. Value in Health. https://doi.org/10.1016/j.jval.2021.11.1361
Peasgood, T., Mukuria, C., Brazier, J., Marten, O., Kreimeier, S., Lou, N., Mulhern, B., Greiner, W., Pickard, S., Augustovski, F., Engel, L., Belizan, M., Yang, Z., & Monteiro, A. (2019). Developing a new generic classifier of quality of life: initial results from the Extending the QALY (E-QALY) psychometric surveys. EuroQol Plenary.
Brazier, J. (2018). Extending the QALY: Generating, selecting and testing items for a new generic measure of quality of life—preliminary results. EuroQol Plenary Meeting.
Stolk, E., Ludwig, K., Rand, K., van Hout, B., & Ramos-Goñi, J. M. (2019). Overview, update, and lessons learned from the international EQ-5D-5L valuation work: version 2 of the EQ-5D-5L valuation protocol. Value Health, 22(1), 23–30.
Mukuria, C., Peasgood, T., McDool, E., Norman, R., Rowen, D., & Brazier, J. (2023). Valuing the EQ health and wellbeing short using time trade-off and a discrete choice experiment: A feasibility study. Value in Health, 26(7), 1073–1084.
Feng, Y. S., Jiang, R., Pickard, A. S., & Kohlmann, T. (2022). Combining EQ-5D-5L items into a level summary score: Demonstrating feasibility using non-parametric item response theory using an international dataset. Quality of Life Research, 31(1), 11–23.
Wilke, C. T., Pickard, A. S., Walton, S. M., Moock, J., Kohlmann, T., & Lee, T. A. (2010). Statistical implications of utility weighted and equally weighted HRQL measures: An empirical study. Health Economics, 19(1), 101–110.
Lamu, A. N., Gamst-Klaussen, T., & Olsen, J. A. (2017). Preference weighting of health state values: what difference does it make, and why? Value Health, 20(3), 451–457.
Prieto, L., & Sacristan, J. A. (2004). What is the value of social values? The uselessness of assessing health-related quality of life through preference measures. BMC Medical Research Methodology, 4, 10.
Devlin, N., Parkin, D., & Janssen, B. (2020). Analysis of EQ-5D profiles. Methods for analysing and reporting EQ-5D data (pp. 23–49). Springer International Publishing.
Devlin, N. A. J. (2010). Getting the most out of proms Putting health outcomes at the heart of NHS decision-making. The King’s Fund.
Parkin, D., Rice, N., & Devlin, N. (2010). Statistical analysis of EQ-5D profiles: Does the use of value sets bias inference? Medical Decision Making, 30(5), 556–565.
Sijtsma, K., & van der Ark, L. A. (2017). A tutorial on how to do a Mokken scale analysis on your test and questionnaire data. British Journal of Mathematical and Statistical Psychology, 70(1), 137–158.
van der Ark, L. A., & Bergsma, W. P. (2010). A note on stochastic ordering of the latent trait using the sum of polytomous item scores. Psychometrika, 75(2), 272–279.
Carlton, J., Peasgood, T., Mukuria, C., Connell, J., Brazier, J., Ludwig, K., Marten, O., Kreimeier, S., Engel, L., Belizán, M., Yang, Z., Monteiro, A., Kuharic, M., Luo, N., Mulhern, B., Greiner, W., Pickard, S., & Augustovski, F. (2022). Generation, selection, and face validation of items for a new generic measure of quality of life: The EQ-HWB. Value in Health, 25(4), 512–524.
Brazier, J., Peasgood, T., Mukuria, C., Marten, O., Kreimeier, S., Luo, N., Mulhern, B., Pickard, A. S., Augustovski, F., Greiner, W., Engel, L., Belizan, M., Yang, Z., Monteiro, A., Kuharic, M., Gibbons, L., Ludwig, K., Carlton, J., Connell, J., … Rejon-Parrilla, J. C. (2022). The EQ-HWB: Overview of the development of a measure of health and wellbeing and key results. Value in Health, 25(4), 482–491.
StataCorp. (2013). Stata statistical software: Release 13. StataCorp LP.
Team RC. (2014). R: A language and environment for statistical computing. R Foundation for Statistical Computing.
van der Ark, L. A. (2007). Mokken scale analysis in R. Journal of Statistical Software, 20(11), 19.
van der Ark, L. A. (2012). New developments in mokken scale analysis in R. Journal of Statistical Software, 48(5), 27.
Pickard, A. S., Law, E. H., Jiang, R., Pullenayegum, E., Shaw, J. W., Xie, F., Oppe, M., Boye, K. S., Chapman, R. H., Gong, C. L., Balch, A., & Busschbach, J. J. V. (2019). United States valuation of EQ-5D-5L health states using an international protocol. Value in Health, 22(8), 931–941.
Monteiro, A. L., Kuharic, M., & Pickard, A. S. (2022). A comparison of a preliminary version of the EQ-HWB short and the 5-level version EQ-5D. Value in Health, 25(4), 534–543.
Brazier, J. E., Mulhern, B. J., Bjorner, J. B., Gandek, B., Rowen, D., Alonso, J., Vilagut, G., & Ware, J. E. (2020). Developing a new version of the SF-6D health state classification system from the SF-36v2: SF-6Dv2. Medical Care, 58(6), 557–565.
Sijtsma, K., & Molenaar, I. W. (2002). Introduction to nonparametric item response theory. SAGE Publications Inc.
van Schuur, W. H. (2003). Mokken scale analysis: Between the Guttman scale and parametric item response theory. Political Analysis, 11(2), 139–163.
Molenaar, I. (1997). Nonparametric models for polytomous responses. In W. J. van der Linden & R. K. Hambleton (Eds.), Handbook of modern item response theory (pp. 369–380). Springer.
Wind, S. A. (2017). An instructional module on mokken scale analysis. Educational Measurement-Issues and Practice, 36(2), 50–66.
Sijtsma, K., & Molenaar, I. W. (2002). The monotone homogeneity model: scalability coefficients. Introduction to nonparametric item response theory (pp. 49–64). SAGE Publications Inc.
Sijtsma, K., Meijer, R., & van der Ark, A. (2011). Mokken scale analysis as time goes by: An update for scaling practitioners. Personality and Individual Differences, 50, 31–37.
Ligtvoet, R., van der Ark, A., Bergsma, W., & Sijtsma, K. (2011). Polytomous latent scales for the investigation of the ordering of items. Psychometrika, 76, 200–216.
Ligtvoet, R., van der Ark, L. A., te Marvelde, J. M., & Sijtsma, K. (2010). Investigating an invariant item ordering for polytomously scored items. Educational and Psychological Measurement, 70(4), 578–595.
McCaffrey, N., Kaambwa, B., Currow, D. C., & Ratcliffe, J. (2016). Health-related quality of life measured using the EQ-5D-5L: South Australian population norms. Health and Quality of Life Outcomes, 14(1), 133.
Janssen, M. F., Pickard, A. S., & Shaw, J. W. (2021). General population normative data for the EQ-5D-3L in the five largest European economies. The European Journal of Health Economics, 22(9), 1467–1475.
Jiang, R., Janssen, M. F. B., & Pickard, A. S. (2021). US population norms for the EQ-5D-5L and comparison of norms from face-to-face and online samples. Quality of Life Research, 30(3), 803–816.
Meijer, R. R., & Egberink, I. J. L. (2012). Investigating invariant item ordering in personality and clinical scales: Some empirical findings and a discussion. Educational and Psychological Measurement, 72(4), 589–607.
Smits, I. A. M., Timmerman, M. E., & Meijer, R. R. (2012). Exploratory mokken scale analysis as a dimensionality assessment tool: Why scalability does not imply unidimensionality. Applied Psychological Measurement, 36(6), 516–539.
Ellis, J. L., & Sijtsma, K. (2023). A test to distinguish monotone homogeneity from monotone multifactor models. Psychometrika, 88(2), 387–412.
Long, D., Bonsel, G. J., Lubetkin, E. I., Yfantopoulos, J. N., Janssen, M. F., & Haagsma, J. A. (2022). Health-related quality of life and mental well-being during the COVID-19 pandemic in five countries: A one-year longitudinal study. Journal of Clinical Medicine, 11(21), 6467.
Spronk, I., Haagsma, J. A., Lubetkin, E. I., Polinder, S., Janssen, M. F., & Bonsel, G. J. (2021). Health inequality analysis in Europe: Exploring the potential of the EQ-5D as outcome. Frontiers in Public Health, 9, 744405.
Acknowledgements
We thank Emeritus Professor John E Brazier (School of Health and Related Research (ScHARR) at the University of Sheffield) for all of his support during this project. All authors are members of the EuroQol group.
Funding
Open Access funding enabled and organized by Projekt DEAL. EuroQol Research Foundation funded this project (Grant ID EQ Project 127-2020RA). The submitted manuscript was not censored or directed by the foundation.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Obtaining secondary data, material preparation and analysis were performed by YSF. The first draft of the manuscript was written by YSF and all authors contributed to revisions on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
All authors on this manuscript are members of the EuroQol group, and have received funding for travel as well as grant support from the EuroQol Research Foundation, a registered not-for-profit Dutch Charity.
Ethical approval
This paper only used secondary data and did not contain human or animal data collection performed by any of the authors. Permissions to use the data were obtained with the principal investigators of the EQ-HWB psychometric study. The EQ-HWB psychometric study conducted data collection aligned with their institutions’ ethics approvals.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Feng, YS., Kohlmann, T., Peasgood, T. et al. Scoring the EQ-HWB-S: can we do it without value sets? A non-parametric item response theory analysis. Qual Life Res 33, 1211–1222 (2024). https://doi.org/10.1007/s11136-024-03601-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-024-03601-7