Abstract
Purpose
To assess oral health-related quality of life (OHRQoL) in patients requiring orthognathic surgery, and evaluate if depression, temporomandibular disorders (TMD), and genetic polymorphisms in interleukin-6 (IL6) influence their OHRQoL.
Methods
A total of 132 individuals included in three different groups. Two groups were composed by patients with dentofacial deformity (DFD) Class II (n = 44) or Class III (n = 44) malocclusions, requiring orthognathic surgery. The control group (n = 44) included individuals without DFD. Patients from all groups were evaluated in preoperative appointments to assessOHRQoL, TMD, and genetic polymorphisms in IL6. OHRQoL was assessed using the 14-item Oral Health Impact Profile (OHIP-14). TMD and depression were assessed using Research Diagnostic Criteria for Temporomandibular Disorders protocol. The genetic polymorphisms rs1800795 and rs1800796 in IL6 were assessed through genomic DNA using real-time polymerase chain reaction.
Results
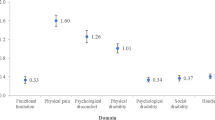
OHIP-14 scores were increased in patients with depression, myofascial pain, and inflammatory temporomandibular joint alterations in the right side, regardless of sex and DFD group. Individual homozygous CC in rs1800795 had increased values in domains “social disability” and “handicap” of the OHIP-14 compared with those who were homozygous GG. Individual heterozygous CG in the rs1800796 demonstrated increased values in domain “psychological discomfort” compared with those homozygous for CC and GG.
Conclusion
In individuals requiring orthognathic surgery, depression, TMD, and genetic polymorphisms in IL6 contribute to negative impact on OHRQoL. These physical and emotional conditions, together with biological pathways, should receive more attention in treatment plans, in order to improve the patients’ quality of life.

Similar content being viewed by others
References
Proffit, W. R., & White, R. P. (1991). The need for surgical-orthodontic treatment. In W. R. Proffit & R. P. White (Eds.), Surgical-orthodontic treatment (pp. 2–23). St. Louis: Mosby.
Choi, S., Kim, B., Cha, J., & Hwang, C. (2015). Impact of malocclusion and common oral diseases on oral health-related quality of life in young adults. American Journal of Orthodontics Dentofacial Orthopedics, 147(5), 587–595.
Sun, H., Shang, H. T., He, L. S., Ding, M. C., Su, Z. P., & Shi, Y. L. (2018). Assessing the quality of life in patients with dentofacial deformities before and after orthognathic surgery. Journal of Oral and Maxillofacial Surgery, 76(10), 2192–2201.
Catt, S. L., Ahmad, S., Collyer, J., Hardwick, L., Shah, N., & Winchester, L. (2018). Quality of life and communication in orthognathic treatment. Journal of Orthodontics, 45(2), 65–70.
Corso, P., Oliveira, F., Costa, D., Kluppel, L., Rebellato, N., & Scariot, R. (2016). Evaluation of the impact of orthognathic surgery on quality of life. Brazilian Oral Research, 30(1), 4.
Silva, I., Cardemil, C., Kashani, H., Bazargani, F., Tarnow, P., Rasmusson, L., et al. (2016). Quality of life in patients undergoing orthognathic surgery: A two-centered Swedish study. Journal of Cranio-Maxillo-Facial Surgery, 44(8), 973–978.
Rusanen, J., Silvola, A. S., Tolvanen, M., Pirttiniemi, P., Lahti, S., & Sipila, K. (2012). Pathways between temporomandibular disorders, occlusal characteristics, facial pain, and oral health-related quality of life among patients with severe malocclusion. European Journal of Orthodontics, 34(4), 512–517.
Al-Moraissi, E. A., Perez, D., & Ellis, E., 3rd. (2017). Do patients with malocclusion have a higher prevalence of temporomandibular disorders than controls both before and after orthognathic surgery? A systematic review and meta-analysis. Journal of Cranio-Maxillo-Facial Surgery, 45(10), 1716–1723.
Mladenović, I., Jović, N., Čutović, T., Mladenović, G., & Kozomara, R. (2013). Temporomandibular disorders after orthognathic surgery in patients with mandibular prognathism with depression as a risk factor. Acta Odontologica Scandinavica, 71(1), 57–64.
Yao, S., Zhou, J., & Li, Z. (2014). Psychologic health status of patients undergoing orthognathic surgery. Journal of Craniofacial Surgery, 25(6), e540–e543.
Slade, G. D. (1997). Derivation and validation of a short-form oral health impact profile. Community Dentistry and Oral Epidemiology, 25(4), 284–290.
Dworking, S. F., & LeResche, L. (1992). Research diagnostic criteria for temporomandibular disorders: Review, criteria, examinations and specifications, critique. Journal of Craniomandibular Disorders, 6(4), 301–355.
Naini, F. B. (2014). Estética Facial: Conceitos e Diagnosticos clinicos (1st ed.). Rio de Janeiro: Elsevier.
Sprangers, M. A., Thong, M. S., Bartels, M., Barsevick, A., Ordonana, J., et al. (2014). Biological pathways, candidate genes and molecular markers associated with quality-of-life domains: An update. Quality of Life Research, 23(7), 1997–2013.
Kimbrel, N. A., Morissette, S. B., Meyer, E. C., Chrestman, R., Jamroz, R., Silvia, P. J., et al. (2015). Effect of the 5-HTTLPR polymorphism on posttraumatic stress disorder, depression, anxiety, and quality of life among Iraq and Afghanistan veterans. Anxiety Stress and Coping, 28(4), 456–466.
Furfari, A., Wan, B. A., Ding, K., Wong, A., Zhu, L., Bezjak, A., et al. (2017). Genetic biomarkers associated with changes in quality of life and pain following palliative radiotherapy in patients with bone metastases. Annals of Palliative Medicine, 6(2), S248–S256.
Dowlati, Y., Herrmann, N., Swardfager, W., Liu, H., Sham, L., Reim, E. K., et al. (2010). A meta-analysis of cytokines in major depression. Biological Psychiatry, 67(5), 446–457.
Ordonãna, J. R., Bartels, M., Boomsma, D. I., Cella, D., Mosing, M., Oliveira, J. R., et al. (2013). Biological pathways and genetic mechanisms involved in social functioning. Quality of Life Research, 22(6), 1189–1200.
Rausch, S. M., Clark, M. M., Patten, C., et al. (2010). Relationship between cytokine gene single nucleotide polymorphisms and symptom burden and quality of life in lung cancer survivors. Cancer, 116(17), 4103–4113.
Vieira, D. A., Da Cunha, L. R., Da Silva, C. B., Almeida, M. T. B., Gomes, A. D., Jr, D. F., et al. (2019). The combined polymorphisms of interleukin-6-174GG genotype and interleukin-10 ATA haplotype are associated with a poor quality of life in patients with chronic hepatitis C. Quality of Life Research, 28(6), 1531–1542.
Bower, J. E., Ganz, P. A., Irwin, M. R., et al. (2013). Cytokine genetic variations and fatigue among patients with breast cancer. Journal of Clinical Oncology, 31(13), 1656–1661.
Simon, N. M., McNamara, K., Chow, C. W., Maser, R. S., Papakostas, G. I., Pollack, M. H., et al. (2008). A detailed examination of cytokine abnormalities in Major Depressive Disorder. European Neuropsychopharmacology, 18(3), 230–233.
Silvola, A. S., Tolvanen, M., Rusanen, J., Sipila, K., Lahti, S., & Pirttiniemi, P. (2016). Do changes in oral health-related quality-of-life, facial pain and temporomandibular disorders correlate after treatment of severe malocclusion? Acta Odontologica Scandinavica, 74(1), 44–50.
Gomes, A. M. P., Garbin, C. A. S., Ferraz, F. W. S., Saliba, T. A., & Garbin, A. J. I. (2019). Dentofacial deformities and implications on quality of life: A presurgical multifactorial analysis in patients seeking orthognathic surgical treatment. Journal of Oral and Maxillofacial Surgery, 77(2), 409.
Little, J., Higgins, J. P., Ioannidis, J. P., Moher, D., Gagnon, F., Von Elm, E., et al. (2009). STrengthening the REporting of Genetic Association studies (STREGA): An extension of the STROBE statement. European Journal of Clinical Investigation, 39(4), 247–266.
Dean, A. G., Sullivan, K. M., Soe, M. M. (2018). OpenEpi: Open Source Epidemiologic Statistics for Public Health, Version. Retrieved Nov 2018 from www.openepi.com.
Almeida, A. M., Loureiro, C. A., & Araujo, V. E. (2015). Um estudo transcultural de valores de saúde bucal utilizando o instrumento OHIP-14 (Oral Health Impact Profile) na forma simplificada. Parte I: adaptação cultural e linguística. UFES Review Odontology, 6(1), 6–15.
Trevilatto, P. C., & Line, S. R. (2000). Use of buccal epithelial cells for PCR amplification of large DNA fragments. Journal of Forensic Odontostomatology, 18(1), 6–9.
Aidar, M., & Line, S. R. (2007). A simple and cost effective protocol for DNA isolation from buccal epithelial cells. Brazilian Dental Journal, 18(2), 148–152.
Oliveira, B. H., & Nadanovsky, P. (2005). Psychometric properties of the Brazilian version of the Oral Health Impact Profile-short form. Community Dentistry and Oral Epidemiology, 33(4), 307–314.
Frejman, M. W., Vargas, I. A., Rösing, C. K., & Closs, L. Q. (2013). Dentofacial deformities are associated with lower degrees of self-esteem and higher impact on oral health-related quality of life: Results from an observational study involving adults. Journal of Oral and Maxillofacial Surgery, 71(4), 763–767.
Göelzer, J. G., Becker, O. E., Haas Junior, O. L., Scolari, N., Santos Melo, M. F., Heitz, C., et al. (2014). Assessing change in quality of life using the Oral Health Impact Profile (OHIP) in patients with different dentofacial deformities undergoing orthognathic surgery: A before and after comparison. International Journal of Oral and Maxillofacial Surgery, 43(11), 1352–1359.
Gava, E. C., Miguel, J. A., De Araújo, A. M., & De Oliveira, B. H. (2013). Psychometric properties of the Brazilian version of the Orthognathic Quality of Life Questionnaire. Journal of Oral and Maxillofacial Surgery, 71(10), 1762.e1–8.
Hescot, P. (2017). The new definition of oral health and relationship between oral health and quality of life. Chinese Journal of Dental Research, 20(4), 189–192.
Yıldız, T., & Selimen, D. (2015). The impact of facial aesthetic and reconstructive surgeries on patients' quality of life. The Indian Journal of Surgery, 77(3), 831–836.
Pace, M., Cioffi, I., Dantò, V., Valletta, A., Valletta, R., & Amato, M. (2018). Facial attractiveness of skeletal class I and class II malocclusion as perceived by laypeople, patients and clinicians. Minerva Stomatology, 67(3), 77–85. https://doi.org/10.23736/S0026-4970.18.04111-0.
Gerzanic, L., Jagsch, R., & Watzke, I. M. (2002). Psychologic implications of orthognathic surgery in patients with skeletal Class II or Class III malocclusion. International Journal of Adult and Orthodontics & Orthognathnic Surgery, 17(2), 75–81.
De Ávila, E. D., De Molon, R. S., Loffredo, L. C., Massucato, E. M., & Hochuli-Vieira, E. (2013). Health-related quality of life and depression in patients with dentofacial deformity. Oral Maxillofacial Surgery, 17(3), 187–191.
Canales, G. T., Guarda-Nardini, L., Rizzatti-Barbosa, C. M., Conti, P. C. R., & Manfredini, D. (2019). Distribution of depression, somatization and pain-related impairment in patients with chronic temporomandibular disorders. Journal of Applied Oral Science, 7(27), e20180210.
Da Fontoura, C. S., Miller, S. F., Wehby, G. L., Amendt, B. A., Holton, N. E., Southard, T. E., et al. (2015). Candidate gene analyses of skeletal variation in malocclusion. Journal of Dental Research, 94(7), 913–920.
Nicot, R., Vieira, A. R., Raoul, G., Delmotte, C., Duhamel, A., Ferri, J., et al. (2016). ENPP1 and ESR1 genotypes influence temporomandibular disorders development and surgical treatment response in dentofacial deformities. Journal of Cranio-Maxillo-Facial Surgery, 44(9), 1226–1237.
Park, H. C., Park, S., Choi, H. Y., Lee, J. E., Park, H. Y., Kim, S. H., et al. (2017). Association of serotonin 1A receptor polymorphism with variation in health-related quality of life in Korean Hemodialysis Patients. Psychiatry Investig, 14(4), 506–512.
Slavich, G. M., & Irwin, M. R. (2014). From stress to inflammation and major depressive disorder: A social signal transduction theory of depression. Psychological Bulletin, 140(3), 774–815.
Hernández, M. E., Mendieta, D., Martínez-Fong, D., Loría, F., Moreno, J., Estrada, I., et al. (2008). Variations in circulating cytokine levels during 52 week course of treatment with SSRI for major depressive disorder. European Neuropsychopharmacology, 18(12), 917–924.
Acknowledgement
This work was supported by individual scholarships (FAPESP – Fundação de Amparo à Pesquisa do Estado de São Paulo-2016/08149-1 and CAPES – Coordenação de Aperfeiçoamento de Pessoal de Nível Superior).
Funding
The work was supported by individual scholarships (FAPESP – Fundação de Amparo à Pesquisa do Estado de São Paulo- 2016/08149-1 and CAPES – Coordenação de Aperfeiçoamento de Pessoal de Nível Superior).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception. The study design was performed by [RS] and [AMS]. Material preparation and data collection were performed by [KMS], [RCC], and [MFP]. Data collection was supervision by [NLBR] and [LS]. Data analyses were performed by [ECK], [RS], and [AMS]. The first draft of the manuscript was written by [AMS] and [RS], the review and editing were performed by [LAAA] and [ECK]. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript. All authors effectively contributed to this work and are familiar with its contents; and assume the responsibility for its contents.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in study were in accordance with the ethical standards of the institutional research committee (Positivo University and Universidade Federal do Paraná: CAEE 69240817.7.0000.0093 and CAAE 69725317.5.0000.0102) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sebastiani, A.M., dos Santos, K.M., Cavalcante, R.C. et al. Depression, temporomandibular disorders, and genetic polymorphisms in IL6 impact on oral health-related quality of life in patients requiring orthognathic surgery. Qual Life Res 29, 3315–3323 (2020). https://doi.org/10.1007/s11136-020-02581-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-020-02581-8