Abstract
Purpose
Postoperative fatigue (POF) is an often underestimated problem after surgery. Studies on POF often report fatigue scores without relating this to the clinical relevance for the patients. The aim of this study was to define the cut-off point for clinically significant POF in three commonly applied fatigue scales; the Postoperative Fatigue Scale, Christensen’s Fatigue Scale, and the Chalder Fatigue Questionnaire. The identification of cut-off points will make it possible to indicate whether statistically significant findings of increased fatigue are of clinical relevance.
Methods
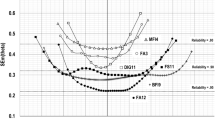
We combined data from day 0 (pre-operatively) and day 1, 3, 6, and 30 after surgery in two fatigue-related studies with 442 patients. In order to define clinically significant fatigue, a key question was added in each questionnaire; “Given your current description of fatigue, would you say it has been of considerable significance to you?”; “Yes/No”. We analysed each scale’s ability to identify clinically significant fatigue, by performing receiver-operating characteristics (ROC) analyses, and calculated the optimal cut-off point between Sensitivity and Specificity.
Results
The average weighted cut-off point for clinically significant POF when measured with the Postoperative Fatigue Scale was ≥ 50 (scale range 0–100), with Christensen’s Fatigue Scale ≥ 6 (scale range 1–10) and with the Chalder Fatigue Questionnaire ≥ 16 (scale range 0–33).
Conclusion
In three commonly used fatigue scales, we have identified cut-off points for clinically significant fatigue among patients recovering from surgery. This can be particularly valuable for diagnostic purposes and in treatment evaluation. Further, it may be possible to analyse and review data from earlier studies in light of clinical relevance.






Similar content being viewed by others
References
Loge, J. H., Ekeberg, O., & Kaasa, S. (1998). Fatigue in the general Norwegian population: normative data and associations. Journal of Psychosomatic Research, 45(1 Spec No), 53–65.
Pawlikowska, T., Chalder, T., Hirsch, S. R., Wallace, P., Wright, D. J., & Wessely, S. C. (1994). Population based study of fatigue and psychological distress. BMJ, 308(6931), 763–766.
Bennett, J. A., Stewart, A. L., Kayser-Jones, J., & Glaser, D. (2002). The mediating effect of pain and fatigue on level of functioning in older adults. Nursing Research, 51(4), 254–265.
Whitehead, L. (2009). The measurement of fatigue in chronic illness: A systematic review of unidimensional and multidimensional fatigue measures. Journal of Pain Symptom Management, 37(1), 107–128. https://doi.org/10.1016/j.jpainsymman.2007.08.019.
Zargar-Shoshtari, K., & Hill, A. G. (2009). Postoperative fatigue: A review. World Journal of Surgery, 33(4), 738–745. https://doi.org/10.1007/s00268-008-9906-0.
Rubin, G. J., Hardy, R., & Hotopf, M. (2004). A systematic review and meta-analysis of the incidence and severity of postoperative fatigue. Journal of Psychosomatic Research, 57(3), 317–326. https://doi.org/10.1016/S0022-3999(03)00615-9.
Bisgaard, T., Klarskov, B., Rosenberg, J., & Kehlet, H. (2001). Factors determining convalescence after uncomplicated laparoscopic cholecystectomy. Archives of Surgery, 136(8), 917–921.
Minig, L., Velez, J. I., Trimble, E. L., Biffi, R., Maggioni, A., & Jeffery, D. D. (2013). Changes in short-term health-related quality of life in women undergoing gynecologic oncologic laparotomy: An associated factor analysis. Support Care Cancer, 21(3), 715–726. https://doi.org/10.1007/s00520-012-1571-z.
DeCherney, A. H., Bachmann, G., Isaacson, K., & Gall, S. (2002). Postoperative fatigue negatively impacts the daily lives of patients recovering from hysterectomy. Obstetrics and Gynecology, 99(1), 51–57.
Dittner, A. J., Wessely, S. C., & Brown, R. G. (2004). The assessment of fatigue: A practical guide for clinicians and researchers. Journal of Psychosomatic Research, 56(2), 157–170. https://doi.org/10.1016/S0022-3999(03)00371-4.
Hill, A. G., Finn, P., & Schroeder, D. (1993). Postoperative fatigue after laparoscopic surgery. Australian and New Zealand Journal of Surgery, 63(12), 946–951.
Christensen, T., Hougard, F., & Kehlet, H. (1985). Influence of pre- and intra- operative factors on the occurrence of postoperative fatigue. British Journal of Surgery, 72(1), 63–65.
Rubin, G. J., & Hotopf, M. (2002). Systematic review and meta-analysis of interventions for postoperative fatigue. British Journal of Surgery, 89(8), 971–984. https://doi.org/10.1046/j.1365-2168.2002.02138.x.
Aarons, H., Forester, A., Hall, G., & Salmon, P. (1996). Fatigue after major joint arthroplasty: relationship to preoperative fatigue and postoperative emotional state. Journal of Psychosomatic Research, 41(3), 225–233.
Hall, G. M., & Salmon, P. (2002). Physiological and psychological influences on postoperative fatigue. Anesthesia Analgesia, 95(5), 1446–1450.
Rubin, G. J., Cleare, A., & Hotopf, M. (2004). Psychological factors in postoperative fatigue. Psychosomatic Medicine, 66(6), 959–964. https://doi.org/10.1097/01.psy.0000143636.09159.f1.
Chalder, T., Berelowitz, G., Pawlikowska, T., Watts, L., Wessely, S., Wright, D., et al. (1993). Development of a fatigue scale. Journal of Psychosomatic Research, 37(2), 147–153.
Michielsen, H. J., De Vries, J., & Van Heck, G. L. (2003). Psychometric qualities of a brief self-rated fatigue measure: The Fatigue Assessment Scale. Journal of Psychosomatic Research, 54(4), 345–352.
Hewlett, S., Dures, E., & Almeida, C. (2011). Measures of fatigue: Bristol Rheumatoid Arthritis Fatigue Multi-Dimensional Questionnaire (BRAF MDQ), Bristol Rheumatoid Arthritis Fatigue Numerical Rating Scales (BRAF NRS) for severity, effect, and coping, Chalder Fatigue Questionnaire (CFQ), Checklist Individual Strength (CIS20R and CIS8R), Fatigue Severity Scale (FSS), Functional Assessment Chronic Illness Therapy (Fatigue) (FACIT-F), Multi-Dimensional Assessment of Fatigue (MAF), Multi-Dimensional Fatigue Inventory (MFI), Pediatric Quality Of Life (PedsQL) Multi-Dimensional Fatigue Scale, Profile of Fatigue (ProF), Short Form 36 Vitality Subscale (SF-36 VT), and Visual Analog Scales (VAS). Arthritis Care Research (Hoboken), 63 Suppl(11), 263–286. https://doi.org/10.1002/acr.20579.
Aaronson, N. K., Ahmedzai, S., Bergman, B., Bullinger, M., Cull, A., Duez, N. J., et al. (1993). The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. Journal of National Cancer Institute, 85(5), 365–376.
Ware, J. E. Jr., & Sherbourne, C. D. (1992). The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care, 30(6), 473–483.
Nostdahl, T., Bernklev, T., Raeder, J., Sandvik, L., & Fredheim, O. (2016). Postoperative fatigue; translation and validation of a revised 10-item short form of the Identity-Consequence Fatigue Scale (ICFS). Journal of Psychosomatic Research, 84, 1–7. https://doi.org/10.1016/j.jpsychores.2016.03.002.
Christensen, T., Bendix, T., & Kehlet, H. (1982). Fatigue and cardiorespiratory function following abdominal surgery. British Journal of Surgery, 69(7), 417–419.
Nostdahl, T., Fredheim, O. M., Bernklev, T., Doksrod, T. S., Mohus, R. M., & Raeder, J. (2017). A randomised controlled trial of propofol vs. thiopentone and desflurane for fatigue after laparoscopic cholecystectomy. Anaesthesia, 72(7), 864–869. https://doi.org/10.1111/anae.13909.
Paddison, J. S., Booth, R. J., Hill, A. G., & Cameron, L. D. (2006). Comprehensive assessment of peri-operative fatigue: development of the Identity-Consequence Fatigue Scale. Journal of Psychosomatic Research, 60(6), 615–622. https://doi.org/10.1016/j.jpsychores.2005.08.008.
Cella, M., & Chalder, T. (2010). Measuring fatigue in clinical and community settings. Journal of Psychosomatic Research, 69(1), 17–22. https://doi.org/10.1016/j.jpsychores.2009.10.007.
Fluss, R., Faraggi, D., & Reiser, B. (2005). Estimation of the Youden Index and its associated cutoff point. Biometrical Journal, 47(4), 458–472.
Youden, W. J. (1950). Index for rating diagnostic tests. Cancer, 3(1), 32–35.
Husted, J. A., Cook, R. J., Farewell, V. T., & Gladman, D. D. (2000). Methods for assessing responsiveness: A critical review and recommendations. Journal of Clinical Epidemiology, 53(5), 459–468.
Crosby, R. D., Kolotkin, R. L., & Williams, G. R. (2003). Defining clinically meaningful change in health-related quality of life. Journal of Clinical Epidemiology, 56(5), 395–407.
Oliveira, M., Oliveira, G., Souza-Talarico, J., & Mota, D. (2016). Surgical oncology: Evolution of postoperative fatigue and factors related to its severity. Clinical Journal of Oncology Nursing, 20(1), E3–E8. https://doi.org/10.1188/16.CJON.E3-E8.
Schroeder, D., & Hill, G. L. (1993). Predicting postoperative fatigue: Importance of preoperative factors. World Journal of Surgery, 17(2), 226–231.
Hosmer, D., & Lemeshow, S. (2000). Applied logistic regression (2ed.). New York: Wiley.
Paddison, J. S., Sammour, T., Kahokehr, A., Zargar-Shoshtari, K., & Hill, A. G. (2011). Development and validation of the Surgical Recovery Scale (SRS). Journal of Surgical Research, 167(2), e85–e91. https://doi.org/10.1016/j.jss.2010.12.043.
Calman, K. C. (1984). Quality of life in cancer patients–an hypothesis. Journal of Medical Ethics, 10(3), 124–127.
Rapkin, B. D., & Schwartz, C. E. (2004). Toward a theoretical model of quality-of-life appraisal: Implications of findings from studies of response shift. Health and Quality of Life Outcomes, 2, 14. https://doi.org/10.1186/1477-7525-2-14.
Schwartz, C. E., & Rapkin, B. D. (2004). Reconsidering the psychometrics of quality of life assessment in light of response shift and appraisal. Health and Quality of Life Outcomes, 2, 16. https://doi.org/10.1186/1477-7525-2-16.
Jansen, S. J., Stiggelbout, A. M., Nooij, M. A., Noordijk, E. M., & Kievit, J. (2000). Response shift in quality of life measurement in early-stage breast cancer patients undergoing radiotherapy. Quality of Life Research, 9(6), 603–615.
Schwartz, C. E., Bode, R., Repucci, N., Becker, J., Sprangers, M. A., & Fayers, P. M. (2006). The clinical significance of adaptation to changing health: A meta-analysis of response shift. Quality of Life Research, 15(9), 1533–1550. https://doi.org/10.1007/s11136-006-0025-9.
Coste, J., Quinquis, L., Audureau, E., & Pouchot, J. (2013). Non response, incomplete and inconsistent responses to self-administered health-related quality of life measures in the general population: patterns, determinants and impact on the validity of estimates—A population-based study in France using the MOS SF-36. Health and Quality of Life Outcomes, 11, 44. https://doi.org/10.1186/1477-7525-11-44.
Peyre, H., Coste, J., & Leplege, A. (2010). Identifying type and determinants of missing items in quality of life questionnaires: Application to the SF-36 French version of the 2003 Decennial Health Survey. Health and Quality of Life Outcomes, 8, 16. https://doi.org/10.1186/1477-7525-8-16.
Funding
Telemark Hospital Trust, Department of Research and Development has been the sole funding source, providing a partial buy-out from consultant practice for Torkjell Nøstdahl.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any conflict of interests to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
See Tables 6, 7, 8, and 9 and Figs. 7 and 8.
Christensen Fatigue Scale (ChrFS) [23]
Rights and permissions
About this article
Cite this article
Nøstdahl, T., Bernklev, T., Fredheim, O.M. et al. Defining the cut-off point of clinically significant postoperative fatigue in three common fatigue scales. Qual Life Res 28, 991–1003 (2019). https://doi.org/10.1007/s11136-018-2068-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-018-2068-0