Abstract
Purpose
Physicians and caregivers rate patient quality of life (QOL) lower than patients rate their own QOL. This study investigated discrepancies between self-assessments of patient QOL by adults with HIV and their surrogate decision-makers.
Methods
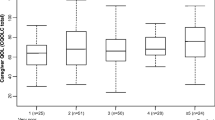
We collected baseline data from 223 adult dyads in the FAmily-CEntered (FACE) Advance Care Planning (ACP) clinical trial, consisting of HIV positive patients and their chosen surrogates. Participants independently completed the Medical Outcome Study-HIV Survey (MOS-HIV) and the Palliative care Outcome Scale (POS). We used Wilcoxon Signed-Rank Test to assess differences in overall patient–surrogate means. We used Prevalence Adjusted Bias Adjusted Kappa (PABAK) statistics to assess dyadic agreement, with surrogate HIV status and cohabitation status as grouping variables.
Results
Patients were 56.1% male, 86.1% Black/African-American, aged 22–77 (mean = 50.83, SD = ± 12.33). Surrogates were 43.8% male, 84.1% Black/African-American, aged 18–82 (mean = 49.73, SD = ± 14.22). 46.2% of surrogates lived with the patient. 64.6% of surrogates reported negative HIV status. Surrogates were more likely to state patients were ill, p = 0.032. Among patient–surrogate dyads, most QOL assessments showed poor (0.00–0.39) or fair (0.40–0.59) agreement and agreement tended to be even poorer among patient–surrogate dyads where the surrogate had a shared HIV diagnosis.
Conclusions
QOL discrepancies are said to arise from healthy surrogates overestimating the effects of chronic illness. In this novel assessment, many surrogates had a shared HIV diagnosis, without increased agreement. These findings highlight the challenge of accurately assessing patient QOL by surrogates, even when there is a shared HIV diagnosis. Improved communication is needed between patients and surrogates about the patients’ representation of illness.
National Clinical Trial Number: NCT01775436.
Similar content being viewed by others
References
Schouten, J., Ferdinand, W. W., Stolte, I. G., Kootstra, N., van der Valk, M., & Geerlings, S. G. (2014). Cross-sectional comparison of the prevalence of age-associated comorbidities and their risk factors between HIV-infected and uninfected individuals: The AGE IV cohort study. Clinical Infectious Diseases. https://doi.org/10.1093/cid/ciu701.
Henderson, W. A., Schlenk, E. A., Kim, K. H., Hadigan, C. M., Martino, A. C., & Sereika, S. M. (2010). Validation of the MOS-HIV as a measure of health-related quality of life in persons living with HIV and liver disease. AIDS Care, 22(4), 483–490.
Wegner, N. S., Kanouse, D. E., Collins, R. L., Liu, H., Schuster, M. A., & Gifford, A. L. (2001). End-of-life discussions and preferences among persons with HIV. JAMA, 285(22), 2880–2890.
Ubel, P. A., Schwarz, N., Loewenstein, G., & Smith, D. (2005). Misimagining the unimaginable: The disability paradox and health care decision making. Health Psychology, 24(4S), S57–S62.
Krug, R., Karus, D., Selwyn, P. A., & Raveis, V. H. (2010). Late-stage HIV/AIDS patients’ and their familial caregivers’ agreement on the palliative care outcome scale. Journal of Pain and Symptom Management, 39(1), 23–32.
Higginson, I. J., & Gao, W. (2008). Caregiver assessment of patients with advanced cancer: Concordance with patients, effect of burden and positivity. Health and Quality of Life Outcomes, 6(1), 42–49.
Li, Y., & Rapkin, B. (2009). Classification and regression tree uncovered hierarchy of psychosocial determinants underlying quality-of-life response shift in HIV/AIDS. Journal of Clinical Epidemiology, 62(11), 1138–1147.
Albrecht, G. L., & Devlieger, P. J. (1999). The disability paradox: High quality of life against all odds. Social Science & Medicine, 48(8), 977–988.
Carona, C., Pereira, M., Moreira, H., Silva, N., & Canavarro, M. C. (2013). The disability paradox revisited: Quality of life and family caregiving in pediatric cerebral palsy. Journal of Child and Family Studies, 22(7), 971–986.
Thompson, W. W., Zack, M. M., Krahn, G. L., Andresen, E. M., & Barile, J. P. (2012). Health-related quality of life among older adults with and without functional limitations. American Journal of Public Health, 102(3), 496–502.
Folkman, S., & Greer, S. (2000). Promoting psychological well-being in the face of serious illness: When theory, research and practice inform each other. Psychooncology, 9(1), 11–19.
Thompson, S. C., Sobolew-Shubin, A., Galbraith, M. E., Schwankovsky, L., & Cruzen, D. (1993). Maintaining perceptions of control: Finding perceived control in low-control circumstances. Journal of Personality and Social Psychology, 64(2), 293–304.
Tarakeshwar, N., Vanderwerker, L. C., Paulk, E., Pearce, M. J., Kasl, S. V., & Prigerson, H. G. (2006). Religious coping is associated with the quality of life of patients with advanced cancer. Journal of Palliative Medicine, 9(3), 646–657.
Pargament, K. I., Koenig, H. G., Tarakeshwar, N., & Hahn, J. (2001). Religious struggle as a predictor of mortality among medically ill elderly patients. Archives of Internal Medicine, 161(15), 1881–1885.
Lee, C. C., Czaja, S. J., & Schulz, R. (2010). The moderating influence of demographic characteristics, social support, and religious coping on the effectiveness of a multicomponent psychosocial caregiver intervention in three racial ethnic groups. Journals of Gerontology Series B, Psychological Sciences and Social Sciences. 65B(2),185–194.
Pargament, K. I., Koenig, H. G., Tarakeshwar, N., & Hahn, J. (2004). Religious coping methods as predictors of psychological, physical and spiritual outcomes among medically ill elderly patients: A two-year longitudinal study. Journal of Health Psychology, 9(6), 713–730.
Mercurio, M. R. (2007). An adolescent’s refusal of medical treatment: Implications of the Abraham Cheerix case. Pediatrics, 120, 1357–1358.
Fins, J., & Schiff, N. (2005). In brief: The afterlife of Terri Schiavo. The Hastings Center Report, 35, 8.
Wijngaards-de Meij, L., Stroebe, M., & Schut, H. (2008). Parents grieving the loss of their child: Interdependence in coping. British Journal of Clinical Psychology, 47(1), 31–42.
Hammes, B. J., Klevan, J., Kempf, M., & Williams, M. S. (2005). Pediatric advance care planning. Journal of Palliative Medicine, 8, 766–773.
Wissow, L. S., Hutton, N., & Kass, N. (2001). Preliminary study of a values-history advance directive interview in a pediatric HIV clinic. Journal of Clinical Ethics, 12(2), 161–172.
Hammes, B. J., & Briggs, L. (2007). Respecting choices: Advance care planning facilitator manual-revised. La Crosse: Gundersen Lutheran Medical Foundation.
O’Connor, A. M. (1995). Validation of a decisional conflict scale. Medical Decision Making, 15(1), 25–30.
Curtis, J. R., Patrick, D. L., Caldwell, E., Greenlee, H., & Collier, A. C. (1999). The quality of patient-doctor communication about end-of-life care: A study of patients with advanced AIDS and their primary care clinicians. AIDS, 13(9), 1123–1131.
Kimmel, A. L., Wang, J., Scott, R., Briggs, L., & Lyon, M. E. (2015). FAmily CEntered (FACE) advance care planning: Study design and methods for a patient-centered communication and decision-making intervention for patients with HIV/AIDS and their surrogate decision-makers. Contemporary Clinical Trials, 43(1), 172–178.
Wu, A. W., Revicki, D. A., Jacobson, D., & Malitz, F. E. (1997). Evidence for reliability, validity and usefulness of the Medical Outcomes Study HIV Health Survey (MOS-HIV). Quality of Life Research, 6(6), 481–493.
Aspinal, F., Hughes, R., Higginson, I., Chidgey, J., Drescher, U., & Thompson, M. (2002). A user’s guide to the Palliative care Outcome Scale (p. 10). London: Palliative Care and Policy Publications.
Hearn, J., & Higginson, I. J. (1999). Development and validation of a core outcome measure for palliative care: The Palliative care Outcome Scale. Palliative Care Core Audit Project Advisory Group. British Medical Journal of Quality & Safety, 8(4), 219–227.
SAS Institute Inc. (2008). SAS® 9.2 enhanced logging facilities. Cary: SAS Institute Inc.
Cicchetti, D. V. (1994). Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychological Assessment, 6, 284–290.
Drum, C. E., Horner-Johnson, W., & Krahn, G. L. (2008). Self-rated health and health days: Examining the “disability paradox”. Disability and Health Journal, 1(2), 71–78.
Graham, C. D., Weinman, J., Sadjadi, R., Chalder, T., Petty, R., & Hanna, M. G. (2014). A multicentre postal survey investigating the contribution of illness perceptions, coping and optimism to quality of life and mood in adults with muscle disease. Clinical Rehabilitation, 28(5), 508–519.
Ashton, E., Vosvick, M., & Chesney, M. (2005). Social support and maladaptive coping as predictors of change in physical health symptoms among persons living with HIV/AIDS. AIDS Patient Care STDs, 19(9), 587–598. https://doi.org/10.1089/apc.2005.19.587.
Holt-Lunstad, J., Smith, T. B., & Layton, J. B. (2010). Social relationships and mortality risk: A meta-analytic review. PLoS Med, 7(7), 1–20. https://doi.org/10.1371/journal.pmed.1000316.
Lyon, M. E., Squires, L., D’Angelo, L., Benator, D., Scott, R., Tanjutco, P., et al. (2017, September 6–8). Advance care planning needs of persons living with HIV/AIDS in Washington, DC: A racial comparison. In Poster 6th international advance care planning end of life conference, Banff, Alberta.
Detering, K. M., Hancock, A. D., Reade, M. C., & Silvester, W. (2010). The impact of advance care planning on end of life care in elderly patients: Randomized controlled trial. British Medical Journal. https://doi.org/10.1136/bmj.c1345.
Song, M. K., Ward, S. E., Denne, H., Happ, M. B., Piraino, B., Donovan, H. S., et al. (2009). Randomized controlled trial of SPIRIT: An effective approach to preparing African-American dialysis patients and families for end-of-life. Research in Nursing & Health, 32(3), 260–273.
Acknowledgements
We thank the study participants for their contributions to the success of this study.
Funding
This research is supported by the National Institute of Nursing Research at the National Institute of Health Award Number R01NR014-052-05; National Institute of Health National Center for Advancing Translational Sciences CTSI-CN UL1RR031988. These institutions were not involved in the present analysis, the interpretation of the data, the writing of the manuscript, or the decision to submit for publication. This content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institute of Health.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare there are no conflicts of interest to report.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This research was approved by the IRB at Children’s National (coordinating center) and at all participating study sites. The Children’s National Medical Center IRB’s Federal Wide Assurance (FWA) number is FWA00004487. The institutional organization number is IORG0000245.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Our study sites were: Children’s National Health System, MedStar Health Research Institute/Washington Hospital Center, MedStar Georgetown University Hospital, The George Washington Medical Faculty Associates and the Washington DC Veterans Affairs Medical Center/Institute for Clinical Research, Inc.
Rights and permissions
About this article
Cite this article
Curtin, K.B., Cheng, Y.I., Wang, J. et al. Quality of life of persons living with HIV and congruence with surrogate decision-makers. Qual Life Res 28, 47–56 (2019). https://doi.org/10.1007/s11136-018-2002-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-018-2002-5