Abstract
Purpose
Black dialysis patients report better health-related quality of life (HRQOL) than White patients, which may be explained if Black and White patients respond systematically differently to HRQOL survey items.
Methods
We examined differential item functioning (DIF) of the Kidney Disease Quality of Life 36-item (KDQOLTM-36) Burden of Kidney Disease, Symptoms and Problems with Kidney Disease, and Effects of Kidney Disease scales between Black (n = 18,404) and White (n = 21,439) dialysis patients. We fit multiple group confirmatory factor analysis models with increasing invariance: a Configural model (invariant factor structure), a Metric model (invariant factor loadings), and a Scalar model (invariant intercepts). Criteria for invariance included non-significant χ2 tests, > 0.002 difference in the models’ CFI, and > 0.015 difference in RMSEA and SRMR. Next, starting with a fully invariant model, we freed loadings and intercepts item-by-item to determine if DIF impacted estimated KDQOLTM-36 scale means.
Results
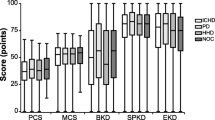
ΔCFI was 0.006 between the metric and scalar models but was reduced to 0.001 when we freed intercepts for the burdens and symptoms and problems of kidney disease scales. In comparison to standardized means of 0 in the White group, those for the Black group on the Burdens, Symptoms and Problems, and Effects of Kidney Disease scales were 0.218, 0.061, and 0.161, respectively. When loadings and thresholds were released sequentially, differences in means between models ranged between 0.001 and 0.048.
Conclusion
Despite some DIF, impacts on KDQOLTM-36 responses appear to be minimal. We conclude that the KDQOLTM-36 is appropriate to make substantive comparisons of HRQOL between Black and White dialysis patients.
Similar content being viewed by others
Abbreviations
- AV:
-
Arteriovenous
- CFA:
-
Confirmatory factor analysis
- CFI:
-
Comparative fit index
- CMS:
-
Centers for Medicare and Medicaid Services
- DIF:
-
Differential item functioning
- DOPPS:
-
Dialysis outcomes and practice patterns study
- ESRD:
-
End-stage renal disease
- HRQOL:
-
Health-related quality of life
- KDCS:
-
Kidney Disease Component Summary
- KDQOL-36:
-
Kidney Disease Quality of Life 36-item survey
- KDQOL-SF:
-
KDQOL-short form
- MCS:
-
Mental Component Summary
- PCS:
-
Physical Component Summary
- PD:
-
Peritoneal dialysis
- RMSEA:
-
Root mean squared error of approximation
- SRMR:
-
Standardized root mean square residual
- US:
-
United States
- WLSMV:
-
Weighted least squares with mean and variance adjustment
References
United States Renal Data System. (2017). 2017 USRDS annual data report: Epidemiology of kidney disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases.
Hertz, R. P., Unger, A. N., Cornell, J. A., & Saunders, E. (2005). Racial disparities in hypertension prevalence, awareness, and management. Archives of Internal Medicine, 165(18), 2098–2104.
Centers for Disease Control and Prevention. (2017). National Diabetes Statistics Report, 2017. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Dept of Health and Human Services.
Hays, R. D., Cunningham, W. E., Sherbourne, C. D., Wilson, I. B., Wu, A. W., Cleary, P. D., McCaffrey, D. F., Fleishman, J. A., Crystal, S., Collins, R., Eggan, F., Shapiro, M. F., & Bozzette, S. A. (2000). Health-related quality of life in patients with human immunodeficiency virus infection in the United States: Results from the HIV cost and services utilization study. The American Journal of Medicine, 108(9), 714–722.
Sledge, R. (2010). KDQOL-36 and the interdisciplinary team. Nephrology News & Issues, 24(7), 36–38.
Peipert, J. D., Bentler, P. M., Klicko, K., & Hays, R. D. (2017). Psychometric properties of the kidney disease quality of life 36-item short-form survey (KDQOL-36) in the United States. American Journal of Kidney Diseases. https://doi.org/10.1053/j.ajkd.2017.07.020.
Hays, R. D., Kallich, J. D., Mapes, D. L., Coons, S. J., & Carter, W. B. (1994). Development of the kidney disease quality of life (KDQOL) instrument. Quality of Life Research, 3(5), 329–338.
Tell, G. S., Mittelmark, M. B., Hylander, B., Shumaker, S. A., Russell, G., & Burkart, J. M. (1995). Social support and health-related quality of life in black and white dialysis patients. ANNA Journal, 22(3), 301–308; discussion 309–310.
Lopes, A. A., Bragg-Gresham, J. L., Satayathum, S., McCullough, K., Pifer, T., Goodkin, D. A., Mapes, D. L., Young, E. W., Wolfe, R. A., Held, P. J., & Port, F. K. (2003). Health-related quality of life and associated outcomes among hemodialysis patients of different ethnicities in the United States: The Dialysis Outcomes and Practice Patterns Study (DOPPS). American Journal of Kidney Diseases, 41(3), 605–615.
Mapes, D. L., Bragg-Gresham, J. L., Bommer, J., Fukuhara, S., McKevitt, P., Wikstrom, B., & Lopes, A. A. (2004). Health-related quality of life in the Dialysis Outcomes and Practice Patterns Study (DOPPS). American Journal of Kidney Diseases, 44(5 Suppl 2), 54–60.
Muthén, L. K., & Muthén, B. O. (2017). Mplus user’s guide. Los Angeles, CA.
Sass, D. A., Schmitt, T. A., & Marsh, H. W. (2014). Evaluating model fit with ordered categorical data within a measurement invariance framework: A comparison of estimators. Structural Equation Modeling-a Multidisciplinary Journal, 21(2), 167–180.
Hu, L. T., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling-a Multidisciplinary Journal, 6(1), 1–55.
Bentler, P. M. (2006). EQS 6 Structural Equations Program Manual. Encino, CA: Multivariate Software, Inc.
Meade, A. W., Johnson, E. C., & Braddy, P. W. (2008). Power and sensitivity of alternative fit indices in tests of measurement invariance. Journal of Applied Psychology, 93(3), 568–592.
Chen, F. F. (2007). Sensitivity of goodness of fit indexes to lack of measurement invariance. Structural Equation Modeling: A Multidisciplinary Journal, 14(3), 464–504.
Yoon, M., & Millsap, R. E. (2007). Detecting violations of factorial invariance using data-based specification searches: A Monte Carlo study. Structural Equation Modeling: A Multidisciplinary Journal, 14(3), 435–463.
Wu, H., & Estabrook, R. (2016). Identification of confirmatory factor analysis models of different levels of invariance for ordered categorical outcomes. Psychometrika, 81(4), 1014–1045.
Asparouhov, T., & Muthen, B. (2010). Simple second order chi-square correction. Los Angeles, CA: Muthén and Muthén.
Fischer, F., Gibbons, C., Coste, J., Valderas, J. M., Rose, M., & Leplege, A. (2018). Measurement invariance and general population reference values of the PROMIS Profile 29 in the UK, France, and Germany. Quality of Life Research. https://doi.org/10.1007/s11136-018-1785-8.
Asparouhov, T., & Muthen, B. (2006). Robust chi square difference testing with mean and variance adjusted test statistics. Los Angeles, CA: Mplus.
Saban, K. L., Bryant, F. B., Reda, D. J., Stroupe, K. T., & Hynes, D. M. (2010). Measurement invariance of the kidney disease and quality of life instrument (KDQOL-SF) across veterans and non-veterans. Health and Quality of Life Outcomes, 8(1), 120.
Unruh, M., Miskulin, D., Yan, G., Hays, R. D., Benz, R., Kusek, J. W., Meyer, K. B., & HEMO Study Group. (2004). Racial differences in health-related quality of life among hemodialysis patients. Kidney International, 65(4), 1482–1491.
Kutner, N. G., & Devins, G. M. (1998). A comparison of the quality of life reported by elderly whites and elderly blacks on dialysis. Geriatric Nephrology and Urology, 8(2), 77–83.
Acknowledgements
We are grateful to Dori Schatell and Ryne Estabrook for their insightful suggestions on this manuscript. There was no direct financial support for the research reported in this manuscript.
Funding
This study was not funded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Ethical approval
This article does not contain any studies with human subjects performed by any of the authors.
Rights and permissions
About this article
Cite this article
Peipert, J.D., Bentler, P., Klicko, K. et al. Negligible impact of differential item functioning between Black and White dialysis patients on the Kidney Disease Quality of Life 36-item short form survey (KDQOLTM-36). Qual Life Res 27, 2699–2707 (2018). https://doi.org/10.1007/s11136-018-1879-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-018-1879-3