Abstract
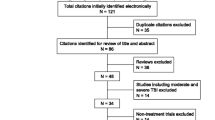
(i) To describe an integrated model of psychiatric care for the treatment of posttraumatic stress disorder (PTSD) in veterans with mild traumatic brain injury (mTBI). (ii) To evaluate access to and engagement in psychiatric care among veterans with comorbid PTSD and mTBI after implementation of an Integrated Care (IC) model compared to the previous Usual Care (UC). 100 randomly selected charts, 50 from each of UC and IC were reviewed in this non-concurrent case- control study. Polytrauma Network Site (PNS), an outpatient rehabilitation clinic, for veterans who suffered from brain and other traumatic injuries at an urban VA Polytrauma Rehabilitation Center. Veterans receiving treatment for mTBI symptoms by the rehabilitation team were referred for medication management for PTSD to UC and IC. Co-located access to psychiatric care for medication management as part of the interdisciplinary team with the goal of expediting rehabilitation and functional recovery. Number of consults for psychiatric care for medication management scheduled and completed within 30 days, and number of veterans offered, initiating, and completing evidence-based psychotherapies for PTSD in UC compared to IC. After implementation of IC there were significant improvements in timely completion of consults and patient engagement with a psychiatrist. There also were improvements in number of referrals, initiation, and completion of evidence-based psychotherapies for the treatment of PTSD. IC within the PNS shows promise as an effective care model for increasing access and engagement in care for veterans with comorbid PTSD/mTBI. Future research is needed to examine the utility of this model in other sites.


Similar content being viewed by others
References
Swanson TM, Isaacson BM, Cyborski CM, French LM, Tsao JW, Pasquina PF. Traumatic brain injury incidence, clinical overview, and policies in the US military health system since 2000. Public Health Rep (Washington, DC : 1974). 2017;132:251–9.
Carroll LJ, Cassidy JD, Peloso PM, Borg J, von Holst H, Holm L, et al. Prognosis for mild traumatic brain injury: results of the WHO collaborating Centre task force on mild traumatic brain injury. J Rehabil Med. 2004;36:84–105.
Ishibe N, Wlordarczyk RC, Fulco C. Overview of the institute of medicine's committee search strategy and review process for gulf war and health: long-term consequences of traumatic brain injury. J Head Trauma Rehabil. 2009;24:424–9.
Iverson GL, Lange RT. Examination of "postconcussion-like" symptoms in a healthy sample. Appl Neuropsychol. 2003;10:137–44.
Kraus J, Schaffer K, Ayers K, Stenehjem J, Shen H, Afifi AA. Physical complaints, medical service use, and social and employment changes following mild traumatic brain injury: a 6-month longitudinal study. J Head Trauma Rehabil. 2005;20:239–56.
Cohen BE, Gima K, Bertenthal D, Kim S, Marmar CR, Seal KH. Mental health diagnoses and utilization of VA non-mental health medical services among returning Iraq and Afghanistan veterans. J Gen Intern Med. 2010;25:18–24.
Tsan JY, Zeber JE, Stock EM, Sun F, Copeland LA. Primary care-mental health integration and treatment retention among Iraq and Afghanistan war veterans. Psychol Serv. 2012;9:336–48.
Fulton JJ, Calhoun PS, Wagner HR, Schry AR, Hair LP, Feeling N, et al. The prevalence of posttraumatic stress disorder in Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) veterans: a meta-analysis. J Anxiety Disord. 2015;31:98–107.
Ramchand R, Schell TL, Karney BR, Osilla KC, Burns RM, Caldarone LB. Disparate prevalence estimates of PTSD among service members who served in Iraq and Afghanistan: possible explanations. J Trauma Stress. 2010;23:59–68.
Chew E, Zafonte RD. Pharmacological management of neurobehavioral disorders following traumatic brain injury--a state-of-the-art review. J Rehabil Res Dev. 2009;46:851–79.
Kessler RC. Posttraumatic stress disorder: the burden to the individual and to society. J Clin Psychiatry. 2000;61(Suppl 5):4–12 discussion 13-14.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed.). Arlington; 2013.
Treatment of posttraumatic stress disorder in military and veteran populations: Final assessment. Washington, DC, USA, Committee on the Assessment of Ongoing Efforts in the Treatment of Posttraumatic Stress Disorder, Board on the Health of Select Populations, Institute of Medicine. 2014;
Asnis GM, Kohn SR, Henderson M, Brown NL. SSRIs versus non-SSRIs in post-traumatic stress disorder: an update with recommendations. Drugs. 2004;64:383–404.
Krystal JH, Davis LL, Neylan TC, AR M, Schnurr PP, Stein MB, et al. It is time to address the crisis in the pharmacotherapy of posttraumatic stress disorder: a consensus statement of the PTSD psychopharmacology working group. Biol Psychiatry. 2017;82:e51–9.
Berger W, Mendlowicz MV, Marques-Portella C, Kinrys G, Fontenelle LF, Marmar CR, et al. Pharmacologic alternatives to antidepressants in posttraumatic stress disorder: a systematic review. Prog Neuro-Psychopharmacol Biol Psychiatry. 2009;33:169–80.
Peskind ER, Bonner LT, Hoff DJ, Raskind MA. Prazosin reduces trauma-related nightmares in older men with chronic posttraumatic stress disorder. J Geriatr Psychiatry Neurol. 2003;16:165–71.
Raskind MA, Peskind ER, Kanter ED, Petrie EC, Radant A, Thompson CE, et al. Reduction of nightmares and other PTSD symptoms in combat veterans by prazosin: a placebo-controlled study. Am J Psychiatry. 2003;160:371–3.
Raskind MA, Thompson C, Petrie EC, Dobie DJ, Rein RJ, Hoff DJ, et al. Prazosin reduces nightmares in combat veterans with posttraumatic stress disorder. J Clin Psychiatry. 2002;63:565–8.
Collett GA, Song K, Jaramillo CA, Potter JS, Finley EP, Pugh MJ. Prevalence of central nervous system polypharmacy and associations with overdose and suicide-related behaviors in Iraq and Afghanistan war veterans in VA care 2010-2011. Drugs-Real World Outcomes. 2016;3:45–52.
Jensen ML, Jorgensen ME, Hansen EH, Aagaard L, Carstensen B. Long-term patterns of adherence to medication therapy among patients with type 2 diabetes mellitus in Denmark: the importance of initiation. PLoS One. 2017;12:e0179546.
Kennedy JE, Leal FO, Lewis JD, Cullen MA, Amador RR. Posttraumatic stress symptoms in OIF/OEF service members with blast-related and non-blast-related mild TBI. NeuroRehabilitation. 2010;26:223–31.
Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, et al. Why don't physicians follow clinical practice guidelines? A framework for improvement. Jama. 1999;282:1458–65.
Duff J, Walker K, Omari A. Translating venous thromboembolism (VTE) prevention evidence into practice: a multidisciplinary evidence implementation project. Worldviews Evid-Based Nurs. 2011;8:30–9.
(DoD) VAVDoD: Managment of Posttraumatic Stress Disorder and Acute Stress Reaction (2017). in Clinical Practice Guidelines U.S. Department of Veterans Affairs 2017.
Corrigan PW, Wassel A. Understanding and influencing the stigma of mental illness. J Psychosoc Nurs Ment Health Serv. 2008;46:42–8.
Seal KH, Maguen S, Cohen B, Gima KS, Metzler TJ, Ren L, et al. Marmar CR. VA mental health services utilization in Iraq and Afghanistan veterans in the first year of receiving new mental health diagnoses. J Trauma Stress. 2010;23:5–16.
Fortney JC, Burgess JF Jr, Bosworth HB, Booth BM, Kaboli PJ. A re-conceptualization of access for 21st century healthcare. J Gen Intern Med. 2011;26(Suppl 2):639–47.
Mott JM, Mondragon S, Hundt NE, Beason-Smith M, Grady RH, Teng EJ. Characteristics of U.S. veterans who begin and complete prolonged exposure and cognitive processing therapy for PTSD. J Trauma Stress. 2014;27:265–73.
Shiner B, D'Avolio LW, Nguyen TM, Zayed MH, Young-Xu Y, Desai RA, et al. Measuring use of evidence based psychotherapy for posttraumatic stress disorder. Admin Pol Ment Health. 2013;40:311–8.
Jeffreys MD, Reinfeld C, Nair PV, Garcia HA, Mata-Galan E, Rentz TO. Evaluating treatment of posttraumatic stress disorder with cognitive processing therapy and prolonged exposure therapy in a VHA specialty clinic. J Anxiety Disord. 2014;28:108–14.
Imel ZE, Laska K, Jakupcak M, Simpson TL. Meta-analysis of dropout in treatments for posttraumatic stress disorder. J Consult Clin Psychol. 2013;81:394–404.
Tarrier N, Pilgrim H, Sommerfield C, Faragher B, Reynolds M, Graham E, et al. A randomized trial of cognitive therapy and imaginal exposure in the treatment of chronic posttraumatic stress disorder. J Consult Clin Psychol. 1999;67:13–8.
Finley EP, Noel PH, Mader M, Haro E, Bernardy N, Rosen CS, et al. Community clinicians and the veterans choice program for PTSD care: understanding provider interest during early implementation. Med Care. 2017;55(Suppl 7 Suppl 1):S61–s70.
Patricia A, Resick PD, Candice M, Monson PD, Kathleen M, Chard PD. Cognitive processing therapy: veterans/military version: Therapist's manual. Washington, DC: Department of Veterans's Affairs; 2014.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. We thank Eric A. Townsend and Edward A. Martinez for their help with accessing the data from electronic medical records. Dr. Baig’s salary was supported by the Department of Veterans Affairs.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
The review of patients’ charts were in accordance with the ethical standards of the Institutional Review Board (IRB) of the University of Texas Health Science Center at San Antonio (UTHSCSA) and STVHCS Research and Development Committee with the 1964 Helsinki declaration and its later amendments.
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
Informed consent from individual participants is not required for the retrospective chart review as no identifying information about participants is available in the article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Baig, M.R., Tapia, R.N., Meraj, A. et al. Enhancing Access to Psychiatric Care for Posttraumatic Stress Disorder in Veterans with Mild Traumatic Brain Injury through Integrated Services. Psychiatr Q 90, 815–827 (2019). https://doi.org/10.1007/s11126-019-09668-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11126-019-09668-7