Abstract
Over 30% of veterans treated for psychiatric disorders in the Veterans Health Administration (VHA) are diagnosed with Post-Traumatic Stress Disorder (PTSD), with most receiving treatment for war-zone stress they experienced decades previously. We examined psychiatric multimorbidity among these patients and consider its implications for treatment and research. Using national VHA data from Fiscal Year 2012 on all veterans diagnosed with PTSD, we compared those with PTSD only to those with one, two, and three or more concurrent (non-substance use) psychiatric disorders. Comparisons of these four groups on sociodemographic characteristics, medical and substance use co-morbidities, health service use, and psychotropic prescription fills were conducted using bi-variate and ordinal logistic regression methods. Of 638,451 veterans diagnosed with PTSD in FY2012, only 29.8% had PTSD alone; 36.7% had one concurrent psychiatric diagnosis, 21.3% had two, and 12.2% had three or more. Anxiety disorder and major depressive disorder were the most common concurrent diagnoses. Veterans with higher levels of multimorbidity were younger, had greater likelihood of recent homelessness, substance use disorder, and diverse medical diagnoses, along with increased mental health and medical service use and greater psychotropic medication use. Psychiatric multimorbidity is highly prevalent among VHA patients diagnosed with PTSD, and may represent an underappreciated and poorly understood clinical complication that poses unique challenges to effective treatment. Clinical attention and both epidemiological and interventional research on multimorbidity in PTSD patients are needed in order to better understand and treat this common but understudied phenomenon.
Similar content being viewed by others
References
Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. Dec. 1995;52(12):1048–60.
Prigerson HG, Maciejewski PK, Rosenheck RA. Population attributable fractions of psychiatric disorders and behavioral outcomes associated with combat exposure among US men. Am J Public Health. Jan. 2002;92(1):59–63.
Steinert C, Hofmann M, Leichsenring F, Kruse J. The course of PTSD in naturalistic long-term studies: high variability of outcomes. A systematic review. Nord J Psychiatry. 2015;69(7):483–96.
A. J. Rosellini et al., Recovery from DSM-IV post-traumatic stress disorder in the WHO world mental health surveys, Psychol Med, pp. 1–14, Jul. 2017.
Koenen KC, Stellman JM, Stellman SD, Sommer JF. Risk factors for course of posttraumatic stress disorder among Vietnam veterans: a 14-year follow-up of American legionnaires. J Consult Clin Psychol. Dec. 2003;71(6):980–6.
Weiss DS, Marmar CR, Schlenger WE, Fairbank JA, Kathleen Jordan B, Hough RL, et al. The prevalence of lifetime and partial post-traumatic stress disorder in Vietnam theater veterans. J Trauma Stress. Jul. 1992;5(3):365–76.
Marmar CR, Schlenger W, Henn-Haase C, Qian M, Purchia E, Li M, et al. Course of posttraumatic stress disorder 40 years after the Vietnam war: findings from the National Vietnam Veterans Longitudinal Study. JAMA Psychiat. Sep. 2015;72(9):875–81.
Corry N, Kulka R, Fairbank J, Schlenger WE. Forty years after the war: how are Vietnam veterans doing today? PTSD Res Q Adv Sci Promot Underst Trauma Stress. 2016;27(1):1–11.
Hermes EDA, Rosenheck RA, Desai R, Fontana AF. Recent trends in the treatment of posttraumatic stress disorder and other mental disorders in the VHA. Psychiatr Serv Wash DC. 2012;63(5):471–6.
Hermes EDA, Hoff R, Rosenheck RA. Sources of the increasing number of Vietnam era veterans with a diagnosis of PTSD using VHA services. Psychiatr Serv Wash DC. Jun. 2014;65(6):830–2.
Schnurr PP, Lunney CA, Sengupta A, Spiro A. A longitudinal study of retirement in older male veterans. J Consult Clin Psychol. Jun. 2005;73(3):561–6.
King DW, King LA, Foy DW, Keane TM, Fairbank JA. Posttraumatic stress disorder in a national sample of female and male Vietnam veterans: risk factors, war-zone stressors, and resilience-recovery variables. J Abnorm Psychol. Feb. 1999;108(1):164–70.
U.S. Military entrance processing command, FY2009, 2009.
Office of the Under Secretary of Defense, Personnel and Readiness, Population Representation in the Military Services: Fiscal Year 2015. Appendix D: Historical Data Tables. Figure 18: Years of completed service for AC enlisted personnel and commissioned officers, FY74-FY14., 2016.
C. S. North, E. S. Brown, and D. E. Pollio, Expanded conceptualization of multimorbidity to encompass substance use disorders and other psychiatric illness, Ann Clin Psychiatry Off J Am Acad Clin Psychiatr, vol. 28, no. 3, pp. 182–188, Aug. 2016.
M. E. Tinetti and J. Basu, Research on multiple chronic conditions: where we are and where we need to go, Med Care, vol 52 Suppl 3, pp. S3–S6, Mar. 2014.
Tinetti ME, Fried TR, Boyd CM. Designing health care for the most common chronic condition--multimorbidity. JAMA. Jun. 2012;307(23):2493–4.
U.S. Department of Defense Task Force on Mental Health, An achievable vision: Report of the Department of Defense Task Force on Mental Health., Defense Health Board, Falls Church, VA, 2007.
Breslau N, Davis GC, Andreski P, Peterson E. Traumatic events and posttraumatic stress disorder in an urban population of young adults. Arch Gen Psychiatry. Mar. 1991;48(3):216–22.
R. H. Pietrzak, R. B. Goldstein, S. M. Southwick, and B. F. Grant, Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: results from wave 2 of the National Epidemiologic Survey on alcohol and related conditions, J Anxiety Disord, vol. 25, no. 3, pp. 456–465, Apr. 2011.
Bowe A, Rosenheck R. PTSD and substance use disorder among veterans: characteristics, service utilization and pharmacotherapy. J Dual Diagn. 2015;11(1):22–32.
S. B. Norman and J. L. Hamblen, Promising directions for treating comorbid PTSD and substance use disorder, Alcohol Clin Exp Res, vol. 41, no. 4, pp. 708–710, Apr. 2017.
Outcalt SD, Hoen HM, Yu Z, Franks TM, Krebs EE. Does comorbid chronic pain affect posttraumatic stress disorder diagnosis and treatment? Outcomes of posttraumatic stress disorder screening in Department of Veterans Affairs primary care. J Rehabil Res Dev. 2016;53(1):37–44.
S. D. Outcalt, K. Kroenke, E. E. Krebs, N. R. Chumbler, J. Wu, Z. Yu, M. J. Bair, Chronic pain and comorbid mental health conditions: independent associations of posttraumatic stress disorder and depression with pain, disability, and quality of life, J Behav Med, vol. 38, no. 3, pp. 535–543, Jun. 2015.
M. M. Burg, C. Brandt, E. Buta, J. Schwartz, H. Bathulapalli, J. Dziura, D.E. Edmondson, S. Haskell, Risk for incident hypertension associated with posttraumatic stress disorder in military veterans and the effect of posttraumatic stress disorder treatment, Psychosom Med, vol. 79, no. 2, pp. 181–188, Mar. 2017.
K. C. Koenen, J. A. Sumner, P. Gilsanz, M. M. Glymour, A. Ratanatharathorn, E. B. Rimm, A. L. Roberts, A. Winning, L. D. Kubzansky, Post-traumatic stress disorder and cardiometabolic disease: improving causal inference to inform practice, Psychol Med, vol. 47, no. 2, pp. 209–225, Jan. 2017.
J. F. Kulas and R. A. Rosenheck, A comparison of veterans with post-traumatic stress disorder, with mild traumatic brain injury and with both disorders: understanding multimorbidity, Mil Med, vol. 183, no. 3–4, pp. e114–e122, Mar. 2018.
G. K. Wolf, G. J. Mauntel, T. Kretzmer, E. Crawford, C. Thors, T. Q. Strom, R. D. Vanderploeg, Comorbid posttraumatic stress disorder and traumatic brain injury: generalization of prolonged-exposure PTSD treatment outcomes to Postconcussive symptoms, cognition, and self-efficacy in veterans and active duty service members, J Head Trauma Rehabil, Sep. 2017, 1.
B. Stubbs, D. Vancampfort, N. Veronese, P. Schofield, P.Y. Lin, P.T. Tseng, M. Solmi, T. Thompson, A. F. Carvalho, A. Koyanagi, Multimorbidity and perceived stress: a population-based cross-sectional study among older adults across six low- and middle-income countries, Maturitas, vol. 107, pp. 84–91, Jan. 2018.
J. S. Williams and L. E. Egede, The association between multimorbidity and quality of life, health status and functional disability, Am J Med Sci, vol. 352, no. 1, pp. 45–52, Jul. 2016.
Z. Agha, R. P. Lofgren, J. V. VanRuiswyk, and P. M. Layde, Are patients at veterans affairs medical centers sicker? A comparative analysis of health status and medical resource use, Arch Intern Med, vol. 160, no. 21, pp. 3252–3257, Nov. 2000.
W. Yu, A. Ravelo, T. H. Wagner, C. S. Phibbs, A. Bhandari, S. Chen, P. G. Barnett, Prevalence and costs of chronic conditions in the VA health care system, Med Care Res Rev, vol. 60, no. 3_suppl, pp. 146S–167S, Sep. 2003.
M. A. Steinman, S. J. Lee, W. John Boscardin, Y. Miao, K. Z. Fung, K. L. Moore, J. B. Schwartz, Patterns of multimorbidity in elderly veterans, J Am Geriatr Soc, vol. 60, no. 10, pp. 1872–1880, Oct. 2012.
E. A. DiNapoli, A. D. Bramoweth, K. L. Whiteman, B. H. Hanusa, and J. Kasckow, Mood disorders in middle-aged and older veterans with multimorbidity, J Aging Health, vol. 29, no. 4, pp. 657–668, Jun. 2017.
Cohen BE, Gima K, Bertenthal D, Kim S, Marmar CR, Seal KH. Mental health diagnoses and utilization of VA non-mental health medical services among returning Iraq and Afghanistan veterans. J Gen Intern Med. Jan. 2010;25(1):18–24.
Hankin CS, Spiro A, Miller DR, Kazis L. Mental disorders and mental health treatment among U.S. Department of Veterans Affairs outpatients: the veterans health study. Am J Psychiatry. Dec. 1999;156(12):1924–30.
Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA. Mar. 2006;295(9):1023–32.
Stecker T, Fortney J, Owen R, McGovern MP, Williams S. Co-occurring medical, psychiatric, and alcohol-related disorders among veterans returning from Iraq and Afghanistan. Psychosomatics. Nov. 2010;51(6):503–7.
Hunter G, Yoon J, Blonigen DM, Asch SM, Zulman DM. Health care utilization patterns among high-cost VA patients with mental health conditions. Psychiatr Serv Wash DC. Sep. 2015;66(9):952–8.
Petrillo LA, Ritchie CS. The challenges of symptom management for patients with multimorbidity in research and practice: a thematic review. Prog Palliat Care. 2016;24(5):262–7.
Zulman DM, Pal Chee C, Wagner TH, Yoon J, Cohen DM, Holmes TH, et al. Multimorbidity and healthcare utilisation among high-cost patients in the US veterans affairs health care system. BMJ Open. Apr. 2015;5(4):e007771.
Leeman RF, Hefner K, Frohe T, Murray A, Rosenheck RA, Watts BV, et al. Exclusion of participants based on substance use status: findings from randomized controlled trials of treatments for PTSD. Behav Res Ther. Feb. 2017;89:33–40.
Franco S, et al. Generalizability of pharmacologic and psychotherapy clinical trial results for posttraumatic stress disorder to community samples. J Clin Psychiatry. Aug. 2016;77(8):975–81.
Friedman MJ, Marmar CR, Baker DG, Sikes CR, Farfel GM. Randomized, double-blind comparison of sertraline and placebo for posttraumatic stress disorder in a Department of Veterans Affairs setting. J Clin Psychiatry. May 2007;68(5):711–20.
Hertzberg MA, Feldman ME, Beckham JC, Kudler HS, Davidson JR. Lack of efficacy for fluoxetine in PTSD: a placebo controlled trial in combat veterans. Ann Clin Psychiatry Off J Am Acad Clin Psychiatr. Jun. 2000;12(2):101–5.
van der Kolk BA, et al. Fluoxetine in posttraumatic stress disorder. J Clin Psychiatry. Dec. 1994;55(12):517–22.
Brooks MS, Laditka SB, Laditka JN. Evidence of greater health care needs among older veterans of the Vietnam war. Mil Med. Aug. 2008;173(8):715–20.
Schlenger WE, Corry NH, Williams CS, Kulka RA, Mulvaney-Day N, DeBakey S, et al. A prospective study of mortality and trauma-related risk factors among a nationally representative sample of Vietnam veterans. Am J Epidemiol. Dec. 2015;182(12):980–90.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Barry DT, Sofuoglu M, Kerns RD, Wiechers IR, Rosenheck RA. Prevalence and correlates of co-prescribing psychotropic medications with long-term opioid use nationally in the veterans health administration. Psychiatry Res. Jun. 2015;227(2–3):324–32.
Hefner K, Sofuoglu M, Rosenheck R. Concomitant cannabis abuse/dependence in patients treated with opioids for non-cancer pain. Am J Addict. Sep. 2015;24(6):538–45.
Gardner MJ, Altman DG. Confidence intervals rather than P values: estimation rather than hypothesis testing. Br Med J (Clin Res Ed). Mar. 1986;292(6522):746–50.
Ferguson CJ. An effect size primer: a guide for clinicians and researchers. Prof Psychol Res Pract. 2009;40(5):532–8.
J. Cohen, Statistical Power Analysis for the Behavioral Sciences, 2 edition. Hillsdale, N.J: Routledge, 1988.
G. D. Garson, Logistic Regression: Binary & Multinomial: 2016 Edition, 2016 edition. Statistical Associates Publishers, 2014.
Reynolds K, Pietrzak RH, Mackenzie CS, Chou KL, Sareen J. Post-traumatic stress disorder across the adult lifespan: findings from a nationally representative survey. Am J Geriatr Psychiatry Off J Am Assoc Geriatr Psychiatry. Jan. 2016;24(1):81–93.
Lenzenweger MF. Epidemiology of personality disorders. Psychiatr Clin North Am. Sep. 2008;31(3):395–403.
Chapman C, Mills K, Slade T, McFarlane AC, Bryant RA, Creamer M, et al. Remission from post-traumatic stress disorder in the general population. Psychol Med. Aug. 2012;42(8):1695–703.
Zlotnick C, Rodriguez BF, Weisberg RB, Bruce SE, Spencer MA, Culpepper L, et al. Chronicity in posttraumatic stress disorder and predictors of the course of posttraumatic stress disorder among primary care patients. J Nerv Ment Dis. Feb. 2004;192(2):153–9.
Yoon J, Zulman D, Scott JY, Maciejewski ML. Costs associated with multimorbidity among VA patients. Med Care, vol 52 Suppl. Mar. 2014;3:S31–6.
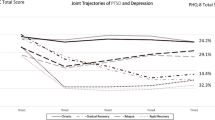
Pietrzak RH, Feder A, Singh R, Schechter CB, Bromet EJ, Katz CL, et al. Trajectories of PTSD risk and resilience in world trade center responders: an 8-year prospective cohort study. Psychol Med. Jan. 2014;44(1):205–19.
Cornell JE, Pugh JA, Williams JW Jr, Kazis L, Lee AFS, Parchman ML, et al. Multimorbidity clusters: clustering binary data from multimorbidity clusters: clustering binary data from a large administrative medical database. Appl Multivar Res. Jan. 2009;12(3):163–82.
P. H. Noël, M. L. Parchman, J. W. Williams Jr, J. E. Cornell, L. Shuko, J. E. Zeber, L. E. Kazis, A. F. S. Lee, J. A. Pugh, The challenges of multimorbidity from the patient perspective, J Gen Intern Med, vol. 22 Suppl 3, pp. 419–424, Dec. 2007.
Zivin K, Pfeiffer PN, Szymanski BR, Valenstein M, Post EP, Miller EM, et al. Initiation of primary care-mental health integration programs in the VA health system: associations with psychiatric diagnoses in primary care. Med Care. Sep. 2010;48(9):843–51.
Wray LO, Szymanski BR, Kearney LK, McCarthy JF. Implementation of primary care-mental health integration services in the veterans health administration: program activity and associations with engagement in specialty mental health services. J Clin Psychol Med Settings. Mar. 2012;19(1):105–16.
O’Connell M, Kasprow W, Rosenheck RA. National dissemination of supported housing in the VA: model adherence versus model modification. Psychiatr Rehabil J. 2010;33(4):308–19.
Funding
This work was funded by the VA New England Mental Illness Research, Education and Clinical Center (MIRECC), which had no role in the study design, data collection, analysis, or interpretation, writing of the report or decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in the present study were in accordance with the ethical standards of the VA Connecticut IRB and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hefner, K., Rosenheck, R. Multimorbidity among Veterans Diagnosed with PTSD in the Veterans Health Administration Nationally. Psychiatr Q 90, 275–291 (2019). https://doi.org/10.1007/s11126-019-09632-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11126-019-09632-5