Abstract
This study builds on past research to examine whether the Medicaid expansion provision of the Affordable Care Act (ACA) affected cohabitation rates among adults ages 18–40. This provision of the ACA was designed to expand health insurance coverage for low-income individuals. The expansion has been demonstrated to have effects beyond increased access to health services, including effects on financial health, marriage, fertility, and child support payments. Nationally representative data from the 2007 to 2019 Current Population Surveys (N = 45,129–695,629) were used to estimate difference-in-difference models of the effect of the Medicaid expansion on cohabitation. Results indicate generally positive effects of the Medicaid expansion on cohabitation, but effects are primarily limited to states expanding in 2014 and are seen 2 years after expansion. Subgroup analyses indicate some heterogeneity by parenthood and race/ethnicity; results are robust to the exclusion of early and late expansion states and to a wider age range. Findings are consistent with behavior around eligibility notches and changes in non-economic factors post-expansion that may influence cohabitation decisions. As states continue to expand Medicaid coverage, such trends may be increasingly evident.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Affordable Care Act (ACA) was passed in 2010 and was designed, in part, to vastly increase health insurance coverage. Although the ACA had many provisions, this paper focuses on the Medicaid expansion that expanded Medicaid coverage to previously ineligible adults (KFF, 2013a) and has been theorized to have far-reaching impacts beyond simply improving access to health care.
Research indicates that the Medicaid expansion, which was implemented beginning in 2014, led to significant increases in health insurance coverage (Courtemanche et al., 2017; Sommers et al., 2015), as well as effects that go beyond health care access and coverage. For example, Miller et al. (2020) found the Medicaid expansion in Michigan was associated with better financial health, including fewer unpaid bills and improved credit scores; Bullinger (2021) found increases in child support payments resulting from the Medicaid expansion; Allen et al. (2017) found the Medicaid expansion in California was associated with reductions in payday borrowing; and Zewde & Wimer (2019) found the expansion was associated with reductions in the poverty rate.
In this study, I examine whether the Medicaid expansion affected rates of cohabitation among younger adults because cohabitation is a popular stage of family formation, financial constraints often influence decisions to cohabit (Sassler & Miller, 2017), recent studies have found the Medicaid expansion affected marriage and divorce (Chatterjee, 2022; Hampton & Lenhart, 2022; Potoms & Rosenberg, 2022; Slusky & Ginther, 2021), and the expansion was targeted to lower-income individuals (KFF, 2013a), who are more likely to cohabit than higher-income individuals (Edin & Kefalas, 2011; Sassler & Miller, 2017). Furthermore, a separate provision of the ACA, the dependent coverage provision, has been linked to marriage, cohabitation, and child bearing (Abramowitz, 2016; Heim et al., 2017).Footnote 1 Only a few studies have considered the role of the Medicaid expansion of the ACA for marriage (Chatterjee, 2022; Hampton & Lenhart, 2022; Potoms & Rosenberg, 2022) and none have considered how the Medicaid expansion may have affected cohabitation. Yet, given its target population, the ACA may have had a greater influence on cohabitation than marriage.
To study this relationship I use data from the 2007 to 2019 waves of the nationally representative Current Population Survey (CPS). After verifying parallel pre-treatment trends in cohabitation between expansion and non-expansion states, I estimate difference-in-difference (DiD) models to assess how the Medicaid expansion affected cohabitation, including DiD models that include an event study component. In addition, I estimate multinomial logistic regression models to compare singlehood, cohabitation, and marriage in the wake of the expansion. I conduct subgroup analyses and robustness checks to examine the consistency of results. I find a significant increase of 0.8–1.2 percentage points in the probability of cohabitation after expansion in the full sample, which appears to be driven by changes in 2014 expansion states that occurred two years after expansion. Multinomial logistic regression results demonstrate increases in cohabitation and marriage compared to singlehood, following the Medicaid expansion. Results are consistent across a number of subgroups and specifications.
Literature Review
ACA Medicaid Expansion
The Medicaid expansion was a response to the fact that most low-income adults were not eligible for Medicaid and thus also had very high levels of uninsurance (KFF, 2013a, 2013b). Coverage under Medicaid prior to the expansion was limited to specific low-income groups, such as the elderly, persons with disabilities, children, pregnant women, and in later years, some groups of parents (KFF, 2013a). The goal of the expansion was to extend health insurance coverage to all poor individuals, including those who were previously ineligible and those whose incomes were up to 138% of the federal poverty line (KFF, 2013b). The intention was for all states to adopt the expansion, but in 2012 the Supreme Court issued a decision allowing states to opt out of the expansion (KFF, 2013a). As of February 2021, 12 states had not expanded Medicaid coverage, and 38 states and Washington DC had adopted a coverage expansion (although some of these states expanded under a waiver program that includes additional restrictions, such as work requirements, and two states have not yet implemented the expansion) (https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/). The initial expansion went into effect in 2014, but several states did not expand Medicaid until later, and states are still continuing to make decisions about whether to expand Medicaid. The lack of a universal adoption allows for a natural experiment comparing family formation patterns in states that did not expand Medicaid and states that did expand Medicaid. In this study I compare cohabitation rates across these two types of states before and after the expansion period.
The underlying premise of this study is that improved access to health insurance has an effect on family formation decisions. The specific focus of this study is on cohabitation, which is a common first step in the family formation process; by age 25, 47 percent of young adults will have cohabited, and about 75 percent of all first unions are cohabitations, according to recent statistics (Brown, 2017). To understand how access to health insurance might lead to changes in family formation, it is necessary to think about reasons for cohabitation and the mechanisms through which health insurance could act on cohabitation.
Reasons for Cohabitation
Young adults enter into cohabitations for a wide variety of reasons. Cohabitation provides many of the benefits of marriage, such as living with an intimate partner and pooling resources, and for some young adults it is a stage in the process from dating to marriage (Brown, 2017). The literature identifies several reasons for cohabitation, comprehensively summarized in Sassler & Miller’s Cohabitation Nation (2017). Although some of these reasons include spending more time together, the convenience of cohabitation, or having a “trial marriage,” other reasons are explicitly related to economics or housing needs, especially for economically vulnerable young adults for whom income pooling may constitute an essential improvisational response to austerity (Sassler & Miller, 2017). For example, many respondents in Sassler and Miller’s study (2017) described financial necessity and economic rationality as underlying reasons for entering into a cohabiting relationship. In the case of economic rationality, a common argument was that living together made good financial sense even if respondents could afford to live alone. However, financial necessity, which refers to more dire financial circumstances, led some cohabitors to live together even when they would rather not, because of situations such as job loss, not earning enough money to cover rent, and so forth (Sassler & Miller, 2017). Although health care costs were not explicitly mentioned by respondents as one of the drivers of financial necessity, health-related costs can be significant, so one can imagine that they could play a contributing role.
Furthermore, cohabitation is often the family formation step chosen by young adults who are reluctant to marry without financial security. Financial security usually refers to having a good job, accumulating some savings, and perhaps owning both a car and a house (Edin & Kefalas, 2011; Sassler & Miller, 2017; Smock et al., 2005). It has become increasingly difficult for young adults to achieve this security, especially less educated young adults, which is a likely driver for higher rates of cohabitation now than in the past (Brown, 2017). Sassler and Miller (2017) note that the decision to cohabit reflects “larger social and economic forces that contribute to the growing gap in the well-being of young adults from more and less advantaged backgrounds” (p. 14).
Possible Mechanisms of Health Insurance on Cohabitation
There are three commonly discussed economic mechanisms for how health insurance may drive changes in individuals’ lives beyond improved access to health care that I focus on, although it is not entirely clear that all would affect cohabitation. These mechanisms are the following: (1) financial protection; (2) cash value; and (3) behavior around eligibility notches. In addition, health insurance may relate to family formation through non-economic pathways.
First, insurance can provide financial protection from significant health expenses (e.g., Yu et al., 2008). Recent research suggests the Medicaid expansion has improved financial well-being in several ways, including by reducing medical debt, payday borrowing, and poverty rates; improving credit scores; and increasing child support payments (Allen et al., 2017; Bullinger, 2021; Miller et al., 2020; Zewde & Wimer, 2019). Prior to the ACA there was evidence of individuals marrying for health insurance reasons, with financial protection being a driving factor (Montez et al., 2009). Thus, if the Medicaid expansion reduced the likelihood of marrying for health insurance specifically, the type of individuals who would have married for health insurance may choose to substitute cohabitation instead, thus increasing cohabitation rates (Abramowitz, 2016). On the other hand, if individuals are cohabiting with the intent to marry (one motivation for cohabitation but not the only reason (Lundberg & Pollak, 2014)), and marriage becomes less likely after the expansion is implemented, then individuals may opt out of cohabitation along with marriage, potentially lowering cohabitation rates (Abramowitz, 2016). Further, greater protection from significant health expenditures may allow individuals more flexibility around decisions about whether to cohabit at all and/or reduce the need to cohabit out of financial necessity.
Second, insurance potentially has a cash value, allowing an insured person to spend money on something else, which is often referred to as an income effect (Buchmueller & Valletta, 1999; Currie & Madrian, 1999). For example, Gruber & Yelowitz (1999) found an increase in consumption following the Medicaid expansions of the 1980s and early 1990s. Similarly, Leininger et al. (2010) found that greater eligibility for the State Children’s Health Insurance Program improved family financial well-being, increasing expenditures in a number of areas, including retirement savings. Thus, the ACA Medicaid expansion might also provide an income effect that could contribute to changes in cohabitation. The cash value mechanism of insurance might mean that newly insured individuals are less likely to cohabit primarily out of financial necessity (Raley et al., 2007; Sassler & Miller, 2017; Smock et al., 2008) because they may be able to reallocate money that they would have otherwise needed for health care.
Third, there can be behavioral changes around eligibility cutoffs (Gruber & Yelowitz, 1999), such as people deciding to work more or less to be eligible for a program. Past research, across a number of social welfare programs, has found that individuals at the margins of eligibility for a program may reduce their work hours, stay single versus marrying, and engage in other behaviors that allow them to obtain/retain eligibility for the program. For example, a recent study on the Earned Income Tax Credit (EITC), which also has strict income cutoffs, indicated that single mothers who expect to lose EITC benefits when they marry are less likely to marry and more likely to cohabit than single mothers for whom marriage would either not change or would increase their EITC benefit (Michelmore, 2018). Based on this study one could posit there might be similar calculations occurring around the eligibility cutoff for the Medicaid expansion that would potentially increase rates of cohabitation. Newly eligible individuals may be particularly concerned about losing this eligibility if they marry (because of the way eligibility is calculated) (Moffitt et al., 1998; Sassler & Miller, 2017), and thus substitute cohabitation for marriage. There is some evidence of this in the literature for pre-ACA Medicaid specifically (e.g., Sassler & Miller, 2017).
Finally, considering non-economic pathways, if health insurance leads to better health or more stable employment, individuals with health insurance might be more attractive partners for cohabitation or marriage. Research indicates the ACA Medicaid expansion improved glucose monitoring among those with diabetes (Mazurenko et al., 2018), control of hypertension (Mazurenko et al., 2018), and self-rated health (Margerison et al., 2020; Mazurenko et al., 2018; Tipirneni et al., 2019). Furthermore, it led to reductions in poor mental health (Mazurenko et al., 2018; Tipirneni et al., 2019) and heavy drinking (Margerison et al., 2020) in some populations. Although few studies examine the role of health for transitions to cohabitation, one study of older adults found better self-rated health linked to increased odds of cohabitation, in comparison to remaining single, especially for women (Brown et al., 2012). Better health has also been associated with the transition to marriage among cohabitors (Wagner, 2019), and there is limited evidence to support a similar relationship for the transition from singlehood to cohabitation among younger adults (Musick & Bumpass, 2012). Thus, healthier individuals may be more likely to transition to cohabitation and marriage, and access to health insurance may help facilitate better health. Additionally, individuals benefiting from the Medicaid expansion appear to experience increases in labor force participation (Callison & Sicilian, 2018; Tipirneni et al., 2020), and, in Michigan, individuals reported improvements in their ability to search for a job or complete their work (Tipirneni et al., 2019). Such changes may have important implications for entry into cohabitation (and marriage); research from France and the UK indicates individuals who are unemployed are much less likely to enter into cohabitation (Borooah, 2002; Ekert-Jaffe & Solaz, 2001), and those with stable employment are more likely to enter into cohabitation (Landaud, 2021). This may result in part from a lack of confidence in the future among the unemployed and their potential partners (Ekert-Jaffe & Solaz, 2001), feelings of uncertainty and inability to make long-term commitments (Landaud, 2021), and a perceived inability of unemployed individuals to provide for a family (Borooah, 2002). Thus, we might see an increase in cohabitation rates due to improvements in stable employment and reduced unemployment after the expansion.
Overall, the evidence suggests there are reasons cohabitation could have increased or decreased with the implementation of the Medicaid expansion, and it is possible that both occurred: cohabitation may have increased for some groups while decreasing for others.
Prior Research on Health Insurance and Family Formation
There is limited research related to how health insurance may impact cohabitation but a larger literature about changes in marriage (and divorce, as a measure of family dissolution) based in a similar theoretical framework. With regard to cohabitation, among older adults, women with private health insurance are less likely to cohabit than women without such insurance (Brown et al., 2012), but little is known about whether this translates to the younger adult population, given that those in their late teens and early 20s (for example) appear to cohabit primarily for economic reasons or convenience (Raley et al., 2007), which may not be the case for older women.
Abramowitz (2016) found the dependent coverage provision of the ACA was associated with decreases in the likelihood of cohabitation and marriage for those affected by the provision using American Community Survey (ACS) data. Enactment and implementation were associated with declines in the probability of cohabitation for those ages 23–25 by between 0.62 and 1.42 percentage points, which corresponded to decreases in cohabitation rates of 4.3% to 9.8% compared to before provision enactment (Abramowitz, 2016). Using tax data, Heim et al. (2017) also examined the dependent coverage provision and found it was associated with a decline in marriage among 24–25 year olds, but they were unable to examine cohabitation.
Research on pre-ACA Medicaid expansions and marriage found mixed results. Yelowitz (1998) found an earlier Medicaid expansion to increase the probability of marriage. Yet, Decker (2000) found prior Medicaid expansions to be associated with an increased probability of singlehood among mothers, suggesting a reduction in the likelihood of marriage. Thus, the literature on prior Medicaid expansions does not provide a clear expected effect of the ACA Medicaid expansion on cohabitation.
To date no studies appear to have examined the role of the ACA Medicaid expansion for cohabitation, and only a couple of studies examined the role for marriage (Chatterjee, 2022; Hampton & Lenhart, 2022; Potoms & Rosenberg, 2022), while another has studied the impact on birth rates (Palmer, 2020), and a few have examined the role of the expansion for divorce (Chatterjee, 2022; Hampton & Lenhart, 2022; Potoms & Rosenberg, 2022; Slusky & Ginther, 2021). Hampton & Lenhart (2022) used ACS data to study the effect of the Medicaid expansion on marriage and divorce decisions. They found reductions in the stock of married people and the likelihood of having married in the prior year, which they attributed to less reliance on health insurance coverage through one’s spouse on the one hand and foregoing marriage to meet eligibility restrictions for Medicaid on the other (Hampton & Lenhart, 2022). Similarly, Chatterjee (2022), also using ACS data, found post-expansion reductions in the newly married population suggestive of substitution away from spousal health insurance coverage, and Potoms & Rosenberg (2022, p. 49) attribute post-expansion reductions in marriage to “individuals being pickier about the (non-pecuniary) quality of a match, and choosing to forego marriages otherwise,” suggesting the potential for cohabitation occurring in place of marriage. These findings suggest we could see increases in cohabitation that are related to shifts in marriage behaviors.
Contributions
The main contribution of this paper is to examine the short- to medium-term effects of the Medicaid expansion on cohabitation using a nationally representative sample and examining differences across important subgroups. I ask whether cohabitation increased or decreased in relation to marriage and singlehood following the Medicaid expansion in states enacting the provision. I use the Current Population Survey (CPS), which is the optimal nationally representative data set for studying changes in cohabitation. Manning (2015) has noted that measuring household relationships in terms of relation to the household head (as in the ACS) provides a limited understanding of family relationships and reduces accurate measurements of non-traditional families. By comparison, the CPS captures cohabitation more broadly within the household, allowing for analysis of cohabiting couples that are not heads of household.
Because states continued to implement the Medicaid expansion after the initial enactment period in 2014, and because there may have been a lag between the time the policy went into effect and changes in individual behaviors, I estimate models using data through 2019. The financial protection and behavior around eligibility notch mechanisms, coupled with recent studies about how the Medicaid expansion has led to reductions in marriage, suggest cohabitation is likely to have increased as newly eligible individuals in Medicaid expansion states find themselves with more flexibility to forego marriage for health insurance reasons on the one hand, and find themselves protective of their eligibility status on the other hand. This leads me to the first two hypotheses:
Hypothesis 1 (H1)
The Medicaid expansion will have a positive effect on cohabitation in the overall sample.
Hypothesis 2 (H2):
Given reduced incentives to marry for health insurance and potential risks of losing Medicaid eligibility with marriage, cohabitation will increase compared to marriage.
Greater financial protection from significant health expenditures, and the “cash value” of health insurance from Medicaid coverage, may allow individuals more flexibility with regard to whether they enter into a cohabitation, especially if they would have otherwise cohabited for financial reasons. Thus, I expect a different pattern for cohabitation compared to singlehood than for cohabitation compared to marriage:
Hypothesis 3 (H3)
Given possible reductions in the necessity to cohabit for financial reasons after Medicaid expansion, cohabitation will decrease in comparison to remaining single.
I first estimate a model for the full sample to test H1. I then compare cohabitation with marriage and singlehood to examine whether individuals are trading off cohabitation for marriage (or vice versa) after the expansion and/or whether they are trading off cohabitation for singlehood (or vice versa). This allows me to test H2 and H3. I assess whether results hold for different subgroups, given variation in cohabitation-related behaviors across demographic characteristics including: sex (Sassler & Miller, 2017), parenthood status (Horowitz et al., 2019), race/ethnicity (Horowitz et al., 2019), school enrollment (Thornton et al., 1995), and age (Horowitz et al., 2019).
Data/Methods
To assess whether the ACA has affected cohabitation patterns, I estimate DiD models and multinomial logistic regression models using data from the CPS. DiD models are useful in situations like this where we expect omitted variable bias to be operating at the state and year level when we assess the effects of policy changes. Furthermore, they include a treatment–control comparison that is ideal for this type of study (Angrist & Pischke, 2008). The intuition is a comparison of two groups before and after a treatment went into effect where only one group receives the treatment. I describe the sample and variables, and then provide additional technical details for the models, including a conceptual diagram for the DiD methodology.
Sample
Data come from the 2007 to 2019 rounds of the Annual Social and Economic Supplement (ASEC) of the CPS, obtained from IPUMS (Flood et al., 2020). The sample includes civilians ages 18–40 because the focus is on younger adult experiences of cohabitation; active duty military members are not included in the sample because their health insurance is provided through the military. The sample is further limited to US citizens because non-citizens may not be eligible for Medicaid, depending on status. Recipients of SSI are excluded because SSI receipt usually provides automatic eligibility for Medicaid (Miller et al., 2021). Finally, in some models the analytic sample is limited to those with incomes below 100% of the federal poverty line (FPL) to avoid contamination from marketplace subsidies in non-expansion states that became available to low-income individuals (with incomes above 100% FPL) around the time of the Medicaid expansion (Johnston et al., 2018). The total sample size varies from 45,129 to 695,629.
Dependent Variable
The primary dependent variable is a binary indicator of the respondent being in a cohabiting relationship compared to another relationship state at the time of the survey. The secondary dependent variable is a binary indicator of the respondent being married compared to another relationship type. Both same-sex and opposite-sex partnerships are included in the analysis. I provide an analysis comparing cohabitation to all other marital statuses and, separately, within the sample of unmarried individuals in the subgroup analyses to assess changes in cohabitation compared to other unmarried states. In the multinomial logistic regression models the categories of cohabitation and marriage are compared to the singlehood category.
Independent Variables
The key independent variable is a dummy variable equal to one to indicate residence in a Medicaid expansion state in a year after which Medicaid was expanded in that state (= 0 otherwise). For example, California expanded Medicaid in 2014. Prior to 2014 the value of this variable for California would be equal to 0 because the Medicaid expansion had not yet occurred. But in 2014, and all subsequent years, the value for California would be 1. Thirty four “treated” states are compared to 17 “non-treated” states. Of the 34 expanded states, 27 expanded in 2014 (with six having some form of expansion prior to 2014 and being defined as early expansion states (Buchmueller et al., 2019)), three expanded in 2015, two in 2016, and two in 2019. The two states that expanded in 2020 are considered untreated in this analysis because they expanded after the last year of CPS data included here.
Controls
The main models control for a linear measure of age; an indicator of female sex; a five-category race/ethnicity variable (Non-Hispanic White, Non-Hispanic Black, Non-Hispanic Asian/Pacific Islander, Non-Hispanic Another Race/Ethnicity, and Hispanic Ethnicity); an indicator for being a parent (= 1 if parent and 0 otherwise); an indicator of school enrollment (= 1 if respondent states they are enrolled in school and 0 otherwise), state fixed effects, and year fixed effects.
Analytic Strategy
The analytic strategy to test Hypothesis 1 is to estimate DiD models of the effect of the Medicaid expansion on cohabitation. Figure 1 shows the conceptual model. As the figure indicates, in the pre-treatment period we are looking for parallel trends for the two comparison groups, one of which will eventually be treated. We track these trends over time. Then the treatment occurs (in this study the implementation of the Medicaid expansion), and we examine trends in cohabitation after the treatment occurs. The assumption is that the control group continues along the same trajectory, but the treatment group may experience an increase or decrease in response to the policy change. This increase or decrease is captured in the DiD model.
I first estimate a basic DiD model, sequentially adding controls, controls plus state fixed effects, controls plus year fixed effects, controls plus stateXyear fixed effects, and controls plus state and year fixed effects. In addition, I estimate the model with controls using the didregress command in Stata 17.0, which is a streamlined approach to estimation. I estimate subgroup analyses and robustness checks, as described later.
Second, I examine to what extent newer DiD methods provide additional information about the treatment effects. I estimate a Bacon decomposition (Goodman-Bacon et al., 2022) on data collapsed to the state levelFootnote 2 to identify how much of the effect comes from differences between expansion states and non-expansion states versus differences within the expansion states (shown in Supplemental Fig. 2). I then estimate the average treatment effect on the treated (ATT) using the csdid estimator (Callaway & Sant’Anna, 2021), which is a DiD-with-multiple-time-periods estimator, using never-treated units as controls.Footnote 3 This method has the advantage of addressing the potential bias in effect estimates that can result under conditions of heterogeneous treatment effects. Additionally, it provides us with insight about which treatment periods yield significant effects and when the effects are seen in terms of time since treatment. Event-history plots were generated using eventdd, which provides estimates from a panel data event study approach to DiD models with a series of lags and leads (Clarke & Tapia Schythe, 2021).
Implementing DiD requires demonstrating that the trends in cohabitation are parallel across treatment and control groups before the implementation of the provision, as noted above (Angrist & Pischke, 2008). Trends in cohabitation are reported in more detail in the results section. To demonstrate parallel trends, I estimate a model using Eq. 1 below, with one change: instead of the key coefficient of interest being residence in an expansion state after expansion I examine an interaction between Medicaid expansion and year in a model limited to the pre-treatment period (pre-2014). In this model the lack of a significant interaction indicates we cannot reject the hypothesis of parallel trends in cohabitation across expansion and non-expansion states (see Supplemental Table 4), whether using the full sample or the sample of respondents with incomes below the poverty line.
Equation 1 represents the Medicaid expansion DiD model. B1 is the coefficient of interest, referring to residence in an expansion state in a year after the expansion was implemented. B2–B3 represent state and year fixed effects, respectively. B4 represents coefficients on the control variables. Standard errors are clustered at the state level, and analyses are weighted to be representative of the population using the person-level ASEC weights.
To test Hypotheses 2 and 3, I estimate multinomial logistic regression models to examine changes in patterns of cohabitation, marriage, and singlehood in the same model. The outcome variable is a tri-level marital status variable taking values of singlehood (omitted comparison category), cohabitation, and marriage. The independent variable is the Medicaid expansion variable used in the DiD models. All multinomial logistic regression models include the same control variables as the DiD models, including state and year fixed effects. Standard errors are clustered at the state level.
Results
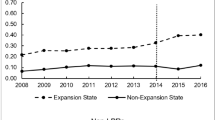
Trends in Cohabitation
The trends in cohabitation prior to the enactment of the Medicaid expansion are not significantly different between expansion and non-expansion states. The test of parallel trends described above (results in Supplemental Table 4) indicate we cannot reject the null hypothesis of parallel trends.
Descriptive Statistics
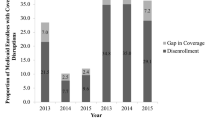
Descriptive statistics for the full sample are shown in Table 1. These are presented separately for expansion and non-expansion states and pre- and post-expansion. Across all states and periods, approximately 11–12% of the sample is cohabiting. About 70% of observations were subject to the Medicaid expansion. About 50% of the sample is female, with higher percentages in the non-expansion states. Non-expansion states also have a higher percentage of Non-Hispanic Blacks, with lower percentages of other Non-Hispanic racial and ethnic groups. Rates of parenthood are slightly higher in the non-expansion states, and rates of school enrollment are slightly lower. For both types of states, parenthood and school enrollment are less common post-expansion, and cohabitation is more common.
Difference-in-Difference Model Results for Hypothesis 1
I first tested the hypothesis that the Medicaid expansion would have a positive effect on cohabitation (H1). Table 2 shows the results of the models, starting with the reduced-form model and subsequently adding the controls and fixed effects. In models that include all marital statuses, there is a significant increase in the probability of cohabitation of 0.8–1.2 percentage points, depending on the model. Results for the models including state X year fixed effects have the opposite sign, which suggests bias in these models, given the consistency of positive results across multiple specifications and methods. The model estimated using didregress command indicates increases in cohabitation of 1.2–1.3 percentage points across income levels, with a 2.4 percentage point increase for those with incomes below the poverty level. Thus, the results support H1 providing evidence that the Medicaid expansion had a positive effect on cohabitation.
The results in Table 3 provide a more complete picture of these effects, taking into account the timing of expansion and the time since expansion. The overall ATT ranges from a 0.8 (with controls) percentage point increase to a 1.0 (without controls) percentage point increase. Furthermore, the results demonstrate the effects are significant only for the group of states that expanded in 2014, and the effects appear to be concentrated in 2016, two years after expansion occurred. Figure 2 depicts the estimates across the pre-treatment and post-treatment periods as estimated using eventdd with the Eq. 1 model specification. There are up to 12 periods before Medicaid expansion and up to five periods after expansion, depending on when the states expanded. Zero represents the expansion year, and cohabitation rates are compared to the year prior to expansion (− 1 in the figure). The point estimates in the figure represent the coefficients estimated by the model, and the 95% confidence intervals are shown. The figure shows relatively small differences in cohabitation rates over time. The eventdd model is estimated slightly differently than the event-history models in Table 3, and the treatment effect for two years post-implementation is only marginally significant (p = 0.069). However, the figure provides a helpful visual representation of the pattern, depicting the effect concentration at two years post-implementation.
For comparison, the results of DiD models with marriage as the outcome are shown in the right-hand columns of Table 3. Unlike the estimates for cohabitation, the estimates for marriage are not statistically significant. The results from the DiD with multiple time periods indicate support for H1 as well but suggest the positive effect on cohabitation was limited to certain states and a certain post-expansion time period. I consider this further in the Discussion.
Multinomial Logistic Regression Model Results for Hypothesis 2 and Hypothesis 3
To test H2 that given reduced incentives to marry for health insurance and potential risks of losing Medicaid eligibility with marriage, cohabitation will increase compared to marriage, and to test H3 that given possible reductions in the necessity to cohabit for financial reasons after Medicaid expansion, cohabitation will decrease compared to remaining single, I estimated multinomial logistic regression models, varying the base outcome. There was no evidence of a significant difference in the probability of marriage compared to cohabitation, and these results are not shown. Thus, there was no evidence for H2. However, compared to being single, the Medicaid expansion was associated with increased odds of both cohabitation and marriage in the full sample, and cohabitation in the sample with incomes below the poverty line (see Table 4). Thus, I find no support for H3; on the contrary I see increases in cohabitation compared to singlehood, rather than decreases.
Subgroup Analyses
As indicated in the background section, the likelihood of entering into cohabitation varies by a number of factors, including sex, race/ethnicity, school enrollment, and so forth. I examined subgroups across each of these domains (results in Table 5): males, females, parents, nonparents, Non-Hispanic Whites, Non-Hispanic Blacks, Non-Hispanic Asian/Pacific Islanders, Non-Hispanic Another Race/Ethnicity, Hispanic Ethnicity, Enrolled in School, and Not Enrolled in School. There was some heterogeneity in the subgroup analysis for H1, but the sample sizes are reduced, which may play a role in explaining some of the null results. In the full sample, results for males and females are relatively consistent with the main model results, though the coefficient for males in the never married model is not statistically significant. Looking at race/ethnicity, increases appear to pertain primarily to Non-Hispanic Whites. School enrollment is not a particularly distinguishing factor in terms of the effect of the expansion on cohabitation. Only one effect is statistically significant in the sample limited to those with incomes below the poverty line; there is a 3.6 percentage point increase for Non-Hispanic Whites when all marital statuses are included.
Robustness Checks
I tested the robustness of the results in a few ways, given the range of samples and cutoff values used in the existing literature. First, I estimated models with different age groups: 18–64 (working age), 25–54 (prime working age), 27–64 (working age and not subject to the dependent coverage provisions), and 18–30 (young adults). The results of the age group analyses are shown at the bottom of Table 5. The estimates for the 18–64 sample are very similar to those for the 18–40 sample, with percentage point increases of 1.0–2.0. For the 25–54 and 27–64 samples the Medicaid expansion is not significantly associated with cohabitation, and this is also true when the sample is limited to young adults, ages 18–30.
Second, I estimated models with different cutoff values indicative of lower income/lower socioeconomic status: income less than 200% of the FPL (instead of < 100% of the FPL), and education of high school diploma or less. Similar measures were used in other recent studies (e.g., Chatterjee, 2022). The results of these models are shown at the top of Table 5. The magnitude of the coefficients in the model with < 200% of the poverty line is nearly identical to the main models, but the estimates are not statistically significant. The coefficients in the model limited to those with a high school diploma or less are a bit smaller in magnitude and not statistically significant.
Third, I excluded the six early expansion states (Buchmueller et al., 2019) and the late expansion states. The concern addressed by these robustness checks is that early expansion and late expansion states might be different from “on-time” expansion states in ways that may also be correlated with the likelihood of cohabitation, for example political liberalness or conservativeness. Results shown in Supplemental Table 3 indicate the exclusion of the early expansion states and late expansion states changes the effect of the Medicaid expansion slightly, increasing the coefficients.
Conclusion
Discussion
This study used data from the CPS to test three hypotheses: H1: The Medicaid expansion will have a positive effect on cohabitation in the overall sample; H2: Given reduced incentives to marry for health insurance and potential risks of losing Medicaid eligibility with marriage, cohabitation will increase in comparison to marriage; H3: Given possible reductions in the necessity to cohabit for financial reasons after Medicaid expansion, cohabitation will decrease in comparison to remaining single.
The study results indicate the Medicaid expansion was associated with increases in cohabitation in the population broadly, supporting H1. However, the effects appear to be driven by states expanding in 2014, suggesting heterogeneity in the outcomes. In an attempt to better understand the patterns of changes in cohabitation, marriage, and singlehood across states from the pre-expansion to post-expansion time periods, I estimated simple t-tests on state-level rates of cohabitation, marriage, and singlehood. The results in Supplemental Table 1 indicate there is not a single pattern being experienced by all expansion states. For example, Washington, D.C., appears to experience increases in cohabitation and marriage in the post-expansion period, and increases in cohabitation (compared to singlehood) are also seen for Indiana. By contrast, Nevada appears to experience decreases in cohabitation (with individuals remaining single) after the expansion. Consistent with the event-history results, most changes are seen for states that expanded in 2014. Across these states there were decreases in marriage and increases in singlehood on the one hand but also decreases in marriage and increases in cohabitation on the other. Thus, these descriptive results suggest that the increases in cohabitation come from both declines in marriage and in singlehood, depending on the state.
In the multinomial logit models, there was no support for H2; the probability of cohabitation was not shown to increase compared to marriage. There was also no support for H3; the probability of cohabitation was instead demonstrated to increase compared to remaining single.
Drawing from studies of prior Medicaid expansions (pre-ACA), research on changes to the EITC, and recent research about change in marriage post-Medicaid expansion, one might have expected that individuals would substitute cohabitation for marriage to preserve eligibility for Medicaid in light of eligibility being expanded to all income-qualifying adults. Surprisingly, the multinomial logit models do not provide any indication of substitution of cohabitation in place of marriage. However, the descriptive state-by-state analysis suggests this may be true for residents of some states (e.g., Colorado and Michigan). In other words, there appears to be heterogeneity across states in how the expansion affects cohabitation and marriage. The increase in cohabitation post-expansion also suggests that non-economic factors may be influential in the relationship between the expansion and decisions about family formation. We cannot rule out the notion that better health and improved labor force attachment may have made some individuals more attractive partners for cohabitation. Indeed, the event-history results indicate a lag between the expansion and increases in cohabitation, which could be attributable in part to these types of health and employment changes.
The multinomial logistic regression models show an increase in marriage post-expansion, compared to singlehood, rather than a decrease (although the DiD with multiple time periods does not show this increase), which is inconsistent with prior studies of the ACA Medicaid expansion and marriage but not unprecedented in the Medicaid expansion and marriage literature. A pre-ACA Medicaid expansion was demonstrated to increase the probability of marriage (Yelowitz, 1998). Additionally, I focus on a younger sample (18–40 years of age) than other recent studies, and I use more years of data (starting 2007 and continuing through 2019).
Limitations
The models used in this study allowed me to examine the effects of the ACA Medicaid expansion on cohabitation at the population level. This is an important contribution to the literature. However, the results do not provide insight regarding those who actually took up the Medicaid expansion compared to those who were eligible but did not take up the provisions. Additionally, longitudinal data would be useful to examine how different types of individuals might change their behaviors in response to the provision, including making changes to labor force participation and experiencing changes in health.
Conclusion
Overall, this study demonstrates positive effects of the Medicaid expansion on cohabitation rates for the sample as a whole. Based on theory and prior research, it seems likely that these results are driven by a combination of behavior around eligibility notches (i.e., cohabiting in place of marriage to maintain Medicaid eligibility) and non-economic attributes that were improved through the Medicaid expansion (e.g., better health, and improved employment). Although further research is needed, results of this and prior studies (e.g., Abramowitz, 2016; Chatterjee, 2022; Hampton & Lenhart, 2022; Heim et al., 2017; Potoms & Rosenberg, 2022) suggest that in general the implementation of the Medicaid expansion (and the dependent coverage provision as well) has allowed adults, especially young adults, more flexibility in terms of decisions related to cohabitation and marriage. It will be important for future research to examine trajectories of young adult relationships over time, with a specific eye toward the possibility that the Medicaid expansion may have allowed some young adults to be more selective about entry into marriage or, alternatively, to have felt more confident about the future and thus ready to enter into a co-residential relationship. In addition, as the Medicaid expansion continues to spread to new states, more research is needed to examine whether the effects of the expansion differ across state policy contexts and what implications such differences might have for cohabitation rates nationally.
Data Availability
Data for this study are available through IPUMS CPS (https://cps.ipums.org/cps/).
Code Availability
Model code can be made available upon request.
Notes
See also the unpublished manuscript by Ma (2015), available at https://jiema.weebly.com/uploads/2/2/7/1/22714530/ma_jie_jobmkt_11_07.pdf
Collapsing the data to the state level was recommended by Austin Nichols (in a personal communication), one of the authors of the bacondecomp command in Stata, because the data in this analysis are repeated cross sections rather than panel data.
The Bacon decomposition indicates expansion versus non-expansion states is the key comparison, rather than the comparison between early expansion and late expansion states.
References
Abramowitz, J. (2016). Saying, “I Don’t”: The effect of the affordable care act young adult provision on marriage. Journal of Human Resources, 51(4), 933–960. https://doi.org/10.3368/jhr.51.4.0914-6643R2
Allen, H., Swanson, A., Wang, J., & Gross, T. (2017). Early medicaid expansion associated with reduced payday borrowing in California. Health Affairs, 36(10), 1769–1776. https://doi.org/10.1377/hlthaff.2017.0369
Angrist, J. D., & Pischke, J.-S. (2008). Mostly harmless econometrics. Princeton University Press. https://doi.org/10.1515/9781400829828/html
Borooah, V. K. (2002). Does unemployment make men less “marriageable”? Applied Economics, 34(12), 1571–1582. https://doi.org/10.1080/00036840110108044
Brown, S. L. (2017). Families in America. University of California Press. https://doi.org/10.1525/9780520961241/html
Brown, S. L., Bulanda, J. R., & Lee, G. R. (2012). Transitions Into and out of cohabitation in later life. Journal of Marriage and Family, 74(4), 774–793. https://doi.org/10.1111/j.1741-3737.2012.00994.x
Buchmueller, T. C., Levy, H. G., & Valletta, R. G. (2019). Medicaid Expansion and the Unemployed. http://www.nber.org/papers/w26553. Accessed 5 June 2022
Buchmueller, T. C., & Valletta, R. G. (1999). The effect of health insurance on married female labor supply. The Journal of Human Resources, 34(1), 42–70. https://doi.org/10.2307/146302
Bullinger, L. R. (2021). Child support and the affordable care act’s medicaid expansions. Journal of Policy Analysis and Management, 40(1), 42–77. https://doi.org/10.1002/pam.22238
Callaway, B., & Sant’Anna, P. H. C. (2021). Difference-in-differences with multiple time periods. Journal of Econometrics, 225(2), 200–230. https://doi.org/10.1016/j.jeconom.2020.12.001
Callison, K., & Sicilian, P. (2018). Economic freedom and the affordable care act: Medicaid expansions and labor mobility by race and ethnicity. Public Finance Review, 46(2), 301–324. https://doi.org/10.1177/1091142116668254
Chatterjee, C. (2022). Impact of the affordable care act medicaid expansions on marriage and divorce decisions. The Center for Growth and Opportunity. https://www.thecgo.org/research/impact-of-the-affordable-care-act-medicaid-expansions-on-marriage-and-divorce-decisions/. Accessed 5 June 2022
Clarke, D., & Tapia Schythe, K. (2021). EVENTDD: Stata module to panel event study models and generate event study plots. https://econpapers.repec.org/software/bocbocode/s458737.htm. Accessed 10 Feb 2023
Courtemanche, C., Marton, J., Ukert, B., Yelowitz, A., & Zapata, D. (2017). Early impacts of the affordable care act on health insurance coverage in medicaid expansion and non-expansion states. Journal of Policy Analysis and Management : [The Journal of the Association for Public Policy Analysis and Management], 36(1), 178–210. https://doi.org/10.1002/pam.21961
Currie, J., & Madrian, B. C. (1999). Chapter 50 health, health insurance and the labor market. Handbook of labor economics (Vol. 3, pp. 3309–3416). Elsevier. https://doi.org/10.1016/S1573-4463(99)30041-9
Decker, S. L. (2000). Medicaid, AFDC and family formation. Applied Economics, 32(15), 1947–1956. https://doi.org/10.1080/00036840050155878
Edin, K., & Kefalas, M. (2011). Promises I Can Keep. University of California Press. https://www.ucpress.edu/ebook.php?isbn=9780520950689. Accessed 7 Sept 2021
Ekert-Jaffe, O., & Solaz, A. (2001). Unemployment, marriage, and cohabitation in France. The Journal of Socio-Economics, 30(1), 75–98. https://doi.org/10.1016/S1053-5357(01)00088-9
Flood, S., King, M., Rodgers, R., Ruggles, R. & Warren, J. R. (2020). Integrated Public Use Microdata Series, Current Population Survey: Version 8.0 [dataset]. Minneapolis, MN: IPUMS. https://doi.org/10.18128/D030.V8.0. Accessed 7 Sept 2021
Goodman-Bacon, A., Goldring, T., & Nichols, A. (2022). BACONDECOMP: Stata module to perform a Bacon decomposition of difference-in-differences estimation. https://econpapers.repec.org/software/bocbocode/s458676.htm. Accessed 10 Feb 2023
Gruber, J., & Yelowitz, A. (1999). Public health insurance and private savings. Journal of Political Economy, 107(6), 1249–1274. https://doi.org/10.1086/250096
Hampton, M., & Lenhart, O. (2022). The effect of the affordable care act medicaid expansion on marriage. Economic Inquiry, 60(2), 568–591. https://doi.org/10.1111/ecin.13052
Heim, B., Lurie, I., & Simon, K. (2017). The impact of the affordable care act young adult provision on childbearing, marriage, and tax filing behavior: Evidence from tax data (No w23092; p w23092). National Bureau of Economic Research. https://doi.org/10.3386/w23092
Horowitz, J. M., Graf, N., & Livingston, G. (2019, November 6). The state of marriage and cohabitation in the U.S. Pew Research Center’s Social & Demographic Trends Project. https://www.pewresearch.org/social-trends/2019/11/06/the-landscape-of-marriage-and-cohabitation-in-the-u-s/. Accessed 7 Sept 2021
Johnston, E. M., Strahan, A. E., Joski, P., Dunlop, A. L., & Adams, E. K. (2018). Impacts of the affordable care act’s medicaid expansion on women of reproductive age: Differences by parental status and state policies. Women’s Health Issues, 28(2), 122–129. https://doi.org/10.1016/j.whi.2017.11.005. Accessed 7 Sept 2021
KFF. (2013a). The ACA medicaid expansion fills current gaps in coverage. https://www.kff.org/health-reform/slide/the-aca-medicaid-expansion-fills-current-gaps-in-coverage/. Accessed 9 Sept 2021
KFF. (2013b). Summary of the affordable care act. https://www.kff.org/health-reform/fact-sheet/summary-of-the-affordable-care-act/. Accessed 9 Sept 2021
Landaud, F. (2021). From employment to engagement? Stable jobs, temporary jobs, and cohabiting relationships. Labour Economics, 73, 102077. https://doi.org/10.1016/j.labeco.2021.102077
Leininger, L., Levy, H., & Schanzenbach, D. (2010). Consequences of SCHIP Expansions for Household Well-Being. Forum for Health Economics & Policy. https://doi.org/10.2202/1558-9544.1201
Lundberg, S., & Pollak, R. A. (2014). Cohabitation and the uneven retreat from marriage in the United States, 1950–2010. University of Chicago Press. https://doi.org/10.7208/9780226163925-009/html
Manning, W. D. (2015). Family formation processes: Assessing the need for a new nationally representative household panel survey in the United States. Journal of Economic and Social Measurement, 40(1–4), 197–219. https://doi.org/10.3233/JEM-150419
Margerison, C. E., MacCallum, C. L., Chen, J., Zamani-Hank, Y., & Kaestner, R. (2020). Impacts of medicaid expansion on health among women of reproductive age. American Journal of Preventive Medicine, 58(1), 1–11. https://doi.org/10.1016/j.amepre.2019.08.019
Mazurenko, O., Balio, C. P., Agarwal, R., Carroll, A. E., & Menachemi, N. (2018). The effects of medicaid expansion under the ACA: A systematic review. Health Affairs, 37(6), 944–950. https://doi.org/10.1377/hlthaff.2017.1491
Michelmore, K. (2018). The earned income tax credit and union formation: The impact of expected spouse earnings. Review of Economics of the Household, 16(2), 377–406. https://doi.org/10.1007/s11150-016-9348-7
Miller, S., Hu, L., Kaestner, R., Mazumder, B., & Wong, A. (2020). The ACA medicaid expansion in michigan and financial health. NBER Working Paper, 25053, 46. http://www.nber.org/papers/w25053. Accessed 7 Sept 2021
Miller, S., Johnson, N., & Wherry, L. R. (2021). Medicaid and mortality: New evidence from linked survey and administrative data*. The Quarterly Journal of Economics, 136(3), 1783–1829. https://doi.org/10.1093/qje/qjab004
Moffitt, R. A., Reville, R., & Winkler, A. E. (1998). Beyond single mothers: Cohabitation and marriage in the AFDC program. Demography (Pre-2011), 35(3), 259–278. http://www.proquest.com/docview/222951068/abstract/758B6B24A4A547ABPQ/1. Accessed 7 Sept 2021
Montez, J. K., Angel, J. L., & Angel, R. J. (2009). Employment, marriage, and inequality in health insurance for Mexican-origin women. Journal of Health and Social Behavior, 50(2), 132–148. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2700956/. Accessed 7 Sept 2021
Musick, K., & Bumpass, L. (2012). Re-examining the case for marriage: Union formation and changes in well-being. Journal of Marriage and the Family, 74(1), 1–18. https://doi.org/10.1111/j.1741-3737.2011.00873.x
Palmer, M. (2020). Does publicly subsidized health insurance affect the birth rate? Southern Economic Journal, 87(1), 70–121. https://doi.org/10.1002/soej.12436
Potoms, T., & Rosenberg, S. (2022). Public insurance and marital outcomes: Evidence from the affordable care act’s medicaid expansion. https://sarah-rosenberg.com/wp-content/uploads/Rosenberg_JMP.pdf. Accessed 5 June 2022
Raley, R. K., Crissey, S., & Muller, C. (2007). Of sex and romance: Late adolescent relationships and young adult union formation. Journal of Marriage and the Family, 69(5), 1210–1226. https://doi.org/10.1111/j.1741-3737.2007.00442.x
Sassler, S., & Miller, A. (2017). Cohabitation nation: Gender, class, and the remaking of relationships. University of California Press. https://doi.org/10.1525/9780520962101
Slusky, D. J. G., & Ginther, D. K. (2021). Did Medicaid expansion reduce medical divorce? Review of Economics of the Household, 19(4), 1139–1174. https://doi.org/10.1007/s11150-021-09566-7
Smock, P. J., Casper, L. M., & Wyse, J. (2008). Nonmarital cohabitation: current knowledge and future directions for research. Population Studies Center Research Report 08-648. Population Studies Center, University of Michigan. https://psc.isr.umich.edu/publications/. Accessed 7 Sept 2021
Smock, P. J., Manning, W. D., & Porter, M. (2005). “Everything’s there except money”: How money shapes decisions to marry among cohabitors. Journal of Marriage and Family, 67(3), 680–696. https://doi.org/10.1111/j.1741-3737.2005.00162.x
Sommers, B. D., Gunja, M. Z., Finegold, K., & Musco, T. (2015). Changes in self-reported insurance coverage, access to care, and health under the affordable care act. JAMA, 314(4), 366–374. https://doi.org/10.1001/jama.2015.8421
Thornton, A., Axinn, W. G., & Teachman, J. D. (1995). The influence of school enrollment and accumulation on cohabitation and marriage in early adulthood. American Sociological Review, 60(5), 762–774. https://doi.org/10.2307/2096321
Tipirneni, R., Ayanian, J. Z., Patel, M. R., Kieffer, E. C., Kirch, M. A., Bryant, C., Kullgren, J. T., Clark, S. J., Lee, S., Solway, E., Chang, T., Haggins, A. N., Luster, J., Beathard, E., & Goold, S. D. (2020). Association of medicaid expansion with enrollee employment and student status in Michigan. JAMA Network Open, 3(1), e1920 316. https://doi.org/10.1001/jamanetworkopen.2019.20316
Tipirneni, R., Kullgren, J. T., Ayanian, J. Z., Kieffer, E. C., Rosland, A.-M., Chang, T., Haggins, A. N., Clark, S. J., Lee, S., Solway, E., Kirch, M. A., Mrukowicz, C., Beathard, E., Sears, E., & Goold, S. D. (2019). Changes in health and ability to work among medicaid expansion enrollees: A mixed methods study. Journal of General Internal Medicine, 34(2), 272–280. https://doi.org/10.1007/s11606-018-4736-8
Wagner, B. (2019). Health status and transitions in cohabiting relationships of American young adults. Journal of Marriage and the Family, 81(4), 847–862. https://doi.org/10.1111/jomf.12572
Yelowitz, A. S. (1998). Will extending medicaid to two-parent families encourage marriage? The Journal of Human Resources, 33(4), 833–865. https://doi.org/10.2307/146400
Yu, H., Dick, A. W., & Szilagyi, P. G. (2008). Does public insurance provide better financial protection against rising health care costs for families of children with special health care needs? Medical Care, 46(10), 1064–1070. https://doi.org/10.1097/MLR.0b013e318185cdf2
Zewde, N., & Wimer, C. (2019). Antipoverty impact of medicaid growing with state expansions over time. Health Affairs, 38(1), 132–21. https://doi.org/10.1377/hlthaff.2018.05155
Acknowledgements
Thank you to Rachel Worrell and Andrew Colwell who contributed as research assistants for this work. Thank you to Adam M. Lippert for comments on a previous version of this manuscript.
Funding
Open access funding provided by SCELC, Statewide California Electronic Library Consortium. Research reported in this publication was partially supported by La Verne Academy small grants from University of La Verne.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that they have no conflict of interest/competing interest.
Ethical Approval
This study is considered “not human subjects research” by the Institutional Review Board at the University of La Verne.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gough Courtney, M. Did the Affordable Care Act’s Medicaid Expansion Change Cohabitation Trends?. Popul Res Policy Rev 42, 46 (2023). https://doi.org/10.1007/s11113-023-09789-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11113-023-09789-9