Abstract
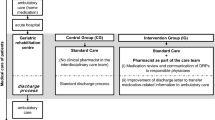
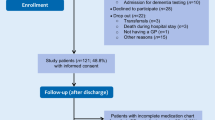
Background Drug-related problems after discharge are common among older adults with polypharmacy. Medication review during hospitalization has been proposed as one solution. Inpatient medication review is often based on clinical records only. An obstacle is the lack of insight into the outpatient history. Therefore, a geriatric stewardship was designed and involved an inpatient medication review by a hospital pharmacist and geriatrician based on (I) clinical records to draft initial recommendations, (II) consultations with primary care providers (general practitioner and community pharmacist) to discuss the hospital-based recommendations, (III) patient interviews to assess their needs, and (IV) a multidisciplinary evaluation of all previous steps to draft final recommendations. Objective To assess the effect of the geriatric stewardship on drug-related problems reported by patients after discharge. Setting General teaching hospital. Methods An implementation study (pre–post design) was performed. Orthopaedic and surgical patients (≥ 65 years) with polypharmacy and a frailty risk factor were included. The pre-group received usual care, the post-group received the geriatric stewardship intervention. Two weeks post-discharge, patient-reported drug-related problems were assessed using a validated questionnaire. Drug-related problems were classified into drug-related complaints, practical problems, and questions about medication. Outcomes The outcomes were the number and type of drug-related problems per patient (primary) and the number of initial recommendations that were altered due to primary care provider and patient input (secondary). Results In total, 127 patients were analysed (usual care n = 74, intervention n = 53). Intervention patients reported fewer drug-related problems compared to usual care: 2.8 versus 3.3 per patient (Adjusted relative risk 0.83, 95% confidence interval 0.66–1.05). This difference resulted from a halving in drug-related complaints (p < 0.05), for example pain, drowsiness, nausea or constipation. Nearly 30% of the initial recommendations based on the clinical records were discarded or modified after primary care provider consultations and patient interviews. Conclusion The geriatric stewardship did not significantly reduce drug-related problems, but it significantly halved drug-related complaints. One-in-three initial recommendations were altered due to primary care provider and patient input. Inpatient medication reviews should not be based on clinical records only; they require transmural collaboration and patient participation to ensure continuity of patient care.


Similar content being viewed by others
References
Ahmad A, Mast MR, Nijpels G, Elders PJ, Dekker JM, Hugtenburg JG. Identification of drug-related problems of elderly patients discharged from hospital. Patient Prefer Adherence. 2014;8:155–65.
Parekh N, Ali K, Page A, Roper T, Rajkumar C. Incidence of Medication-related harm in older adults after hospital discharge: a systematic review. J Am Geriatr Soc. 2018;66(9):1812–22.
Griese-Mammen N, Hersberger KE, Messerli M, Leikola S, Horvat N, van Mil JWF, et al. PCNE definition of medication review: reaching agreement. Int J Clin Pharm. 2018;40(5):1199–2008.
Mangoni AA, Jackson SH. Age-related changes in pharmacokinetics and pharmacodynamics: basic principles and practical applications. Br J Clin Pharmacol. 2004;57(1):6–14.
El Morabet N, Uitvlugt EB, van den Bemt BJF, van den Bemt P, Janssen MJA, Karapinar-Carkit F. Prevalence and preventability of drug-related hospital readmissions: a systematic review. J Am Geriatr Soc. 2018;66(3):602–8.
Witherington EM, Pirzada OM, Avery AJ. Communication gaps and readmissions to hospital for patients aged 75 years and older: observational study. Qual Saf Health Care. 2008;17(1):71–5.
Chiatti C, Bustacchini S, Furneri G, Mantovani L, Cristiani M, Misuraca C, et al. The economic burden of inappropriate drug prescribing, lack of adherence and compliance, adverse drug events in older people: a systematic review. Drug Saf. 2012;35(Suppl 1):73–87.
NHG. Multidisciplinaire richtlijn polyfarmacie bij ouderen (Dutch Guideline: ‘Multidisciplinary Guideline Polypharmacy in the Elderly’). 2012. Available at https://richtlijnen.nhg.org/files/2020-05/polyfarmacie_bij_ouderen.pdf. Accessed 7 July 2020.
NVvG. Addendum Polyfarmacie bij ouderen in de tweede lijn (Addendum Dutch Guideline: ‘Multidisciplinary Guideline Polypharmacy in the Elderly in secondary care’). 2018. Available at https://richtlijnendatabase.nl/nieuws/addendum_polyfarmacie_bij_ouderen_in_de_tweede_l.html. Accessed 7 July 2020.
Hohl CM, Wickham ME, Sobolev B, Perry JJ, Sivilotti ML, Garrison S, et al. The effect of early in-hospital medication review on health outcomes: a systematic review. Br J Clin Pharmacol. 2015;80(1):51–61.
Christensen M, Lundh A. Medication review in hospitalised patients to reduce morbidity and mortality. Cochrane Database Syst Rev. 2016;20(2):CD008986.
Geurts MM, Talsma J, Brouwers JR, de Gier JJ. Medication review and reconciliation with cooperation between pharmacist and general practitioner and the benefit for the patient: a systematic review. Br J Clin Pharmacol. 2012;74(1):16–33.
Farris KB, Carter BL, Xu Y, Dawson JD, Shelsky C, Weetman DB, et al. Effect of a care transition intervention by pharmacists: an RCT. BMC Health Serv Res. 2014;14:406.
Gillespie U, Alassaad A, Henrohn D, Garmo H, Hammarlund-Udenaes M, Toss H, et al. A comprehensive pharmacist intervention to reduce morbidity in patients 80 years or older: a randomized controlled trial. Arch Intern Med. 2009;169(9):894–900.
Lisby M, Bonnerup DK, Brock B, Gregersen PA, Jensen J, Larsen ML, et al. Medication review and patient outcomes in an orthopedic department: a randomized controlled study. J Patient Saf. 2018;14(2):74–81.
Schnipper JL, Kirwin JL, Cotugno MC, Wahlstrom SA, Brown BA, Tarvin E, et al. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Arch Intern Med. 2006;166(5):565–71.
Bonnerup DK, Lisby M, Sædder EA, Sørensen CA, Brock B, Andersen L, et al. Risk of prescribing errors in acutely admitted patients: a pilot study. Int J Clin Pharm. 2016;38(5):1157–63.
Viktil KK, Blix HS, Moger TA, Reikvam A. Interview of patients by pharmacists contributes significantly to the identification of drug-related problems (DRPs). Pharmacoepidemiol Drug Saf. 2006;15(9):667–74.
Stämpfli D, Boeni F, Gerber A, Bättig VAD, Hersberger KE, Lampert ML. Contribution of patient interviews as part of a comprehensive approach to the identification of drug-related problems on geriatric wards. Drugs Aging. 2018;35(7):665–75.
Blenkinsopp A, Bond C, Raynor DK. Medication reviews. Br J Clin Pharmacol. 2012;74:573–80.
Bladh L, Ottosson E, Karlsson J, Klintberg L, Wallerstedt SM. Effects of a clinical pharmacist service on health-related quality of life and prescribing of drugs: a randomised controlled trial. BMJ Qual Saf. 2011;20(9):738–46.
Scullin C, Scott MG, Hogg A, McElnay JC. An innovative approach to integrated medicines management. J Eval Clin Pract. 2007;13(5):781–8.
Kripalani S, Theobald CN, Anctil B, Vasilevskis EE. Reducing hospital readmission rates: current strategies and future directions. Annu Rev Med. 2014;65:471–85.
Ravn-Nielsen LV, Duckert ML, Lund ML, Henriksen JP, Nielsen ML, Eriksen CS, et al. Effect of an in-hospital multifaceted clinical pharmacist intervention on the risk of readmission: a randomized clinical trial. JAMA Intern Med. 2018;178(3):375–82.
Kempen TGH, Bertilsson M, Lindner KJ, Sulku J, Nielsen EI, Högberg A, et al. Medication Reviews Bridging Healthcare (MedBridge): study protocol for a pragmatic cluster-randomised crossover trial. Contemp Clin Trials. 2017;61:126–32.
Ensing HT, Stuijt CC, van den Bemt BJ, van Dooren AA, Karapinar-Çarkit F, Koster ES, et al. Identifying the optimal role for pharmacists in care transitions: a systematic review. J Manag Care Spec Pharm. 2015;21(8):614–36.
Knight DA, Thompson D, Mathie E, Dickinson A. ‘Seamless care? Just a list would have helped!’ Older people and their carer’s experiences of support with medication on discharge home from hospital. Health Expect. 2013;16(3):277–91.
Mistiaen P, Duijnhouwer E, Wijkel D, de Bont M, Veeger A. The problems of elderly people at home one week after discharge from an acute care setting. J Adv Nurs. 1997;25(6):1233–40.
Mohammed MA, Moles RJ, Chen TF. Medication-related burden and patients’ lived experience with medicine: a systematic review and metasynthesis of qualitative studies. BMJ Open. 2016;6(2):e010035.
Blok C. de, Koster E, Schilp J, Wagner C. Implementation of the Dutch National Patient Safety Programme (VMS Veiligheidsprogramma): evaluation research in Dutch hospitals. Summary. Utrecht/Amsterdam: NIVEL, EMGO + Instituut, 2013. Available at: https://www.nivel.nl/nl/publicatie/implementation-dutch-national-patient-safety-programme-vms-veiligheidsprogramma. Accessed 7 July 2020.
O’Mahony D, O’Sullivan D, Byrne S, O’Connor MN, Ryan C, Gallagher P. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015;44(2):213–8.
Willeboordse F, Grundeken LH, van den Eijkel LP, Schellevis FG, Elders PJ, Hugtenburg JG. Information on actual medication use and drug-related problems in older patients: questionnaire or interview? Int J Clin Pharm. 2016;38(2):380–7.
Cua YM, Kripalani S. Medication use in the transition from hospital to home. Ann Acad Med Singap. 2008;37(2):136–46.
Daliri S, Hugtenburg JG, Ter Riet G, van den Bemt BJF, Buurman BM, Scholte OP, Reimer WJM, et al. The effect of a pharmacy-led transitional care program on medication-related problems post-discharge: a before-after prospective study. PLoS ONE. 2019;14(3):e0213593.
Eibergen L, Janssen MJA, Blom L, Karapinar-Çarkit F. Informational needs and recall of in-hospital medication changes of recently discharged patients. Res Social Adm Pharm. 2018;14(2):146–52.
Schoenmakers TW, Teichert M, Wensing M, de Smet PA. Evaluation of potentially drug-related patient-reported common symptoms assessed during clinical medication reviews: a cross-sectional observational study. Drug Saf. 2017;40(5):419–30.
Verdoorn S, Kwint HF, Blom J, Gussekloo J, Bouvy ML. DREAMeR: drug use reconsidered in the elderly using goal attainment scales during medication review; study protocol of a randomised controlled trial. BMC Geriatr. 2018;18(1):190.
Zhu J, Stuver SO, Epstein AM, Schneider EC, Weissman JS, Weingart SN. Can we rely on patients’ reports of adverse events? Med Care. 2011;49(10):948–55.
Weingart SN, Gandhi TK, Seger AC, Seger DL, Borus J, Burdick E, et al. Patient-reported medication symptoms in primary care. Arch Intern Med. 2005;165(2):234–40.
Parekh N, Ali K, Davies JG, Stevenson JM, Banya W, Nyangoma S, et al. Medication-related harm in older adults following hospital discharge: development and validation of a prediction tool. BMJ Qual Saf. 2020;29(2):142–53.
Acknowledgements
We would like to acknowledge the patients involved in this study as well as the GPs and community pharmacists who participated. We also thank N. Khorsand, S.U. Kisoensingh, O.J. de Vries, T.H. Geersing, E.B. Uitvlugt, B. Nikolik, B.J.D. Gerritsen, M. Yilmaz, R. de Heij, and A.R.E. Wapstra for their assistance with the data collection, and W.H. Heideman and T. van der Ploeg for their help with the analysis.
Funding
No funding was received for performing this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix 1: Questionnaire: structured telephone interview two weeks post-discharge
Appendix 1: Questionnaire: structured telephone interview two weeks post-discharge
A: Any symptoms
“I would like to discuss with you many common physical complaints. Not everyone suffers from these complaints, but it is possible. For each complaint I mention, can you indicate whether you are bothered by it?”

B: Practical problems
“Using medicines can sometimes cause practical problems. I will now mention a number of statements. For the statements, could you indicate whether you agree or disagree?”

C: Questions about medication

D: Satisfaction

.
Rights and permissions
About this article
Cite this article
Ponjee, G.H.M., van de Meerendonk, H.W.P.C., Janssen, M.J.A. et al. The effect of an inpatient geriatric stewardship on drug-related problems reported by patients after discharge. Int J Clin Pharm 43, 191–202 (2021). https://doi.org/10.1007/s11096-020-01133-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-020-01133-x