Abstract
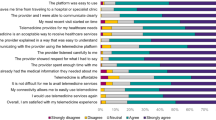
Background Assessing and satisfying patient expectation are essential in successful patient-centered communication. Recognizing the gap between patient expectation and perception during pharmacist–patient communication can help to identify communication problems and suggest ways to improve communication. Objective To evaluate the gap between patient expectation and perception of sharing information and communications skills during pharmacist–patient communication. Setting Community pharmacies in South Korea. Method A questionnaire was developed to collect expectation and perception of sharing information and communication skills. Items for sharing information included drug effect, dosage/route of administration, adverse drug reactions, storage, drug–drug interactions, drug–food interactions, managing a missed dose or overdose, co-medication, and past drug allergies. Communication skills included friendliness, expertise, easy language, emphasis on main content, confirmation of understanding, enough time, calm environment, and private space. A cross-sectional survey was conducted in 500 convenience sample using an online or written questionnaire in May 2018. Responses about patient expectation and perception were scored using 4-point Likert scales. Gap between patient expectation and perception was calculated as the differences among 4-point Likert scores. Factors associated with patient expectation and gap scores were evaluated using a multivariable regression method. Main outcome measure Patient expectation and perception of sharing information, as well as perception of communication skills during pharmacist–patient communication (questionnaire consisting 35 items). Results This study analyzed responses of 460 participants who answered all items on the questionnaire. Most respondents agreed or strongly agreed that they want to share information with pharmacists. All items had significant gap between patient expectation and perception (p < 0.01). Gap scores were highest for adverse drug reaction, drug–drug interaction, and past drug allergies (all, median 2). Gap scores were negatively associated with age 50–59 years, ≥ 60 years, and presence of ≥ 1 chronic illness. Patient perception of communication skills, especially regarding private space, were poor. Conclusions The information shared with pharmacists was significantly less than that expected by participants, and most pharmacist communication skills were evaluated as poor. Understanding the expectation of each patient and communicating accordingly with appropriate communication skills are necessary to improve patient-centered communication in community pharmacies.
Similar content being viewed by others
Change history
16 August 2020
In the original publication of the article the order of authors has been interchanged and now the same has been provided correctly in this correction.
References
Kerr A, Strawbridge J, Kelleher C, Mertens F, Pype P, Deveugele M, et al. How can pharmacists develop patient–pharmacist communication skills? A realist review protocol. Syst Rev. 2017;6(1):14.
Stewart M, Brown JB, Donner A, McWhinney IR, Oates J, Weston WW, et al. The impact of patient-centered care on outcomes. J Fam Pract. 2000;49(9):796–804.
Thamby SA, Subramani P. Seven-star pharmacist concept of WHO. J Young Pharm. 2014;6(2):1–3.
Murad MS, Chatterley T, Guirguis LM. A meta-narrative review of recorded patient–pharmacist interactions: exploring biomedical or patient-centered communication? Res Soc Adm Pharm RSAP. 2014;10(1):1–20.
Naughton CA. Patient-centered communication. Pharmacy (Basel). 2018;6(1):13.
Wolters M, van Hulten R, Blom L, Bouvy ML. Exploring the concept of patient centred communication for the pharmacy practice. Int J Clin Pharm. 2017;39(6):1145–56.
Perrault EK, Beal JL. The effect of pharmacy setting and pharmacist communication style on patient perceptions and selection of pharmacists. J Am Pharm Assoc. (2013). 2018;58(4):404–11.
Borgsteede SD, Karapinar-Carkit F, Hoffmann E, Zoer J, van den Bemt PM. Information needs about medication according to patients discharged from a general hospital. Patient Educ Couns. 2011;83(1):22–8.
Kazaryan I, Sevikyan A. Patients in need of medicine information. Int J Risk Saf Med. 2015;27(Suppl 1):S21–S2222.
Horne R, Hankins M, Jenkins R. The satisfaction with information about medicines scale (SIMS): a new measurement tool for audit and research. Qual Health Care. 2001;10(3):135–40.
Kayyali R, Gomes AM, Mason T, Naik M. patients perceptions of medication counselling from community pharmacies. Pharm Pharmacol Int J. 2016;4(2):00071.
Gültekin O, Abdi AM, Al-Baghdadi H, Akansoy M, Rasmussen F, Başgut B. Counseling of inhalation medicine perceived by patients and their healthcare providers: insights from North Cyprus. Int J Clin Pharm. 2019;41(5):1272–81.
Ministry of Health and Welfare, Pharmaceutical Affairs Act (2016). https://elaw.klri.re.kr/kor_service/lawView.do?hseq=40196&lang=ENG;2017. Accessed 15 Sep 2019.
Lee JH, Sohn HS, Shin HT. Quality evaluation of medication counseling in Korean community pharmacies. Korean J Clin Pharm. 2009;19(2):131–45.
Gregorio J, Cavaco AM, Lapao LV. How to best manage time interaction with patients? Community pharmacist workload and service provision analysis. Res Soc Adm Pharm RSAP. 2017;13(1):133–47.
Park J, Jung M. A note on determination of sample size for a Likert scale. Commun Korean Stat Soc. 2009;16(4):669–73.
Parasuraman A, Ziethaml V, Berry LL. SERVQUAL: a multiple-item scale for measuring consumer perceptions of service quality. J Retail. 1985;62(1):12–40.
Mohammadi A, Shoghli A. Survey on quality of primary health cares in Zanjan district health centers. J Zanjan Univ Med Sci. 2009;16(65):89–100.
Abolghasem Gorji H, Tabatabaei SM, Akbari A, Sarkhosh S, Khorasan S. Using the service quality gap's model (SERVQUAL) in Imam Khomeini teaching hospital. J Health Adm. 2013;16(51):7–18.
Mohebifar R, Hasani H, Barikani A, Rafiei S. Evaluating service quality from patients' perceptions: application of importance-performance analysis method. Osong Public Health Res Perspect. 2016;7(4):233–8.
Fryar CD, Ostchega Y, Hales CM, Zhang G, Kruszon-Moran D. Hypertension prevalence and control among adults: United States, 2015–2016. NCHS Data Brief. 2017;289. https://www.cdc.gov/nchs/data/databriefs/db289.pdf. Accessed 11 Jan 2020.
National Center for Chronic Disease Prevention and Health Promotion. National diabetes statistics report. 2017. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf. Accessed 11 Jan 2020.
Takaki H, Abe T, Hagihara A. Perceptions of pharmacists and patients on information provision and their influence on patient satisfaction in Japanese community pharmacies. J Eval Clin Pract. 2015;21(6):1135–41.
Hattingh HL, Emmerton L, Ng Cheong Tin P, Green C. Utilization of community pharmacy space to enhance privacy: a qualitative study. Health Expect. 2016;19(5):1098–110.
Rapport F, Doel MA, Jerzembek GS. "Convenient space" or "a tight squeeze": insider views on the community pharmacy. Health Place. 2009;15(1):315–22.
Thompson L, Bidwell S. Space, time, and emotion in the community pharmacy. Health Place. 2015;34:251–6.
Statistics Korea. Population by age and sex 2016. https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1IN1603;2017. Accessed 14 Sep 2019.
Statistics Korea. Population by region and population density 2019. https://www.index.go.kr/potal/main/EachDtlPageDetail.do?idx_cd=1007. Accessed 11 Jan 2020.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Myeong Gyu Kim analyzed data and wrote the manuscript. Na Eun Lee developed a questionnaire and carried out the survey. Hyun Soon Sohn developed a questionnaire, conceived and planned the experiments.
Corresponding author
Ethics declarations
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kim, M.G., Lee, N.E. & Sohn, H.S. Gap between patient expectation and perception during pharmacist–patient communication at community pharmacy. Int J Clin Pharm 42, 677–684 (2020). https://doi.org/10.1007/s11096-020-01014-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-020-01014-3