Abstract
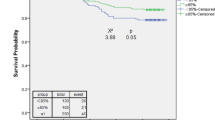
Background Nonconformity to chemotherapy schedules is common in clinical practice. Multiple clinical studies have established the negative prognostic impact of dose delay on survival outcome. Objective This study investigated the prevalence and reason for chemotherapy schedule modifications of breast cancer patients. This study also investigated the impact of schedule modifications on overall survival (OS). Setting This retrospective cohort study was done among breast cancer patient receiving chemotherapy from 2013 to 2017 and patients were followed until 31 Dec 2018. Methods Medical records of patients with cancer were reviewed. Female patients over eighteen years old were included, with primary carcinoma of the breast, who received anthracycline or taxane based chemotherapy regime and completed more than two cycles of chemotherapy. Patients were categorized into three groups of (1) no schedule modification, (2) with schedule modification and (3) incomplete schedule. The Kaplan–Meier was used to test for survival differences in the univariate setting and Cox regression model was used in the multivariate setting. Main outcome measure Prevalence, overall survival rates and hazard ratio of three schedule group Results Among 171 patient who were included in the final analysis, 28 (16.4%) had no schedule modification, 118 (69.0%) with schedule modification and 25 (14.6%) had incomplete schedule with OS of 75.0%, 59.3% and 52.0% respectively. 94% (189) of all cycle rescheduling happened because of constitutional symptoms (70), for non-medical reasons (61) and blood/bone marrow toxicity (58). When compared to patients with no schedule modification, patients with schedule modification had a 2.34-times higher risk of death (HR 2.34, 95% CI 1.03–5.32; p = 0.043). Conclusion Nonconformity to the chemotherapy schedule is common in clinical practice because of treatment complications, patients’ social schedule conflicts, and facility administrative reasons. Cumulative delays of ≥ 14 days are likely to have negative prognostic effect on patient survival. Thus, the duration of the delays between cycles should be reduced whenever possible to achieve the maximum chemotherapeutic benefit.


Similar content being viewed by others
References
Giordano SH, Lin Y-L, Kuo YF, Hortobagyi GN, Goodwin JS. Decline in the use of anthracyclines for breast cancer. J Clin Oncol. 2012;30(18):2232.
Group EBCTC. Comparisons between different polychemotherapy regimens for early breast cancer: meta-analyses of long-term outcome among 100 000 women in 123 randomised trials. The Lancet. 2012; 379(9814): 432–44.
Group EBCTC. Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. The Lancet. 2005; 365(9472): 1687–717.
Lyman GH, Dale DC, Crawford J. Incidence and predictors of low dose-intensity in adjuvant breast cancer chemotherapy: a nationwide study of community practices. J Clin Oncol. 2003;21(24):4524–31.
Wu Y, Aravind S, Ranganathan G, Martin A, Nalysnyk L. Anemia and thrombocytopenia in patients undergoing chemotherapy for solid tumors: a descriptive study of a large outpatient oncology practice database, 2000–2007. Clin Ther. 2009;31:2416–32.
Riccardi A, Pugliese P, Danova M, Brugnatelli S, Grasso D, Giordano M, et al. A phase II study of sequential 5-fluorouracil, epirubicin and cyclophosphamide (FEC) and paclitaxel in advanced breast cancer (Protocol PV BC 97/01). Br J Cancer. 2001;85(2):141–6.
Martin M, Villar A, Sole-Calvo A, Gonzalez R, Massuti B, Lizon J, et al. Doxorubicin in combination with fluorouracil and cyclophosphamide (i.v. FAC regimen, day 1, 21) versus methotrexate in combination with fluorouracil and cyclophosphamide (i.v. CMF regimen, day 1, 21) as adjuvant chemotherapy for operable breast cancer: a study by the GEICAM group. Ann Oncol. 2003;14(6):833–42.
Iwata H, Sato N, Masuda N, Nakamura S, Yamamoto N, Kuroi K, et al. Docetaxel followed by fluorouracil/epirubicin/cyclophosphamide as neoadjuvant chemotherapy for patients with primary breast cancer. Jpn J Clin Oncol. 2011;41(7):867–75.
Bonneterre J, Dieras V, Tubiana-Hulin M, Bougnoux P, Bonneterre ME, Delozier T, et al. Phase II multicentre randomised study of docetaxel plus epirubicin vs 5-fluorouracil plus epirubicin and cyclophosphamide in metastatic breast cancer. Br J Cancer. 2004;91(8):1466–71.
Italian Multicentre Breast Study with E, Ambrosini G, Balli M, Garusi G, Demicheli R, Jirillo A, et al. Phase III randomized study of fluorouracil, epirubicin, and cyclophosphamide v fluorouracil, doxorubicin, and cyclophosphamide in advanced breast cancer: an Italian multicentre trial. J Clin Oncology Off J Am Soc Clin Oncol. 1988; 6(6): 976–82.
Buzdar AU, Suman VJ, Meric-Bernstam F, Leitch AM, Ellis MJ, Boughey JC, et al. Fluorouracil, epirubicin, and cyclophosphamide (FEC-75) followed by paclitaxel plus trastuzumab versus paclitaxel plus trastuzumab followed by FEC-75 plus trastuzumab as neoadjuvant treatment for patients with HER2-positive breast cancer (Z1041): a randomised, controlled, phase 3 trial. Lancet Oncol. 2013;14(13):1317–25.
Hryniuk W, Levine M. Analysis of dose intensity for adjuvant chemotherapy trials in stage II breast cancer. J Clin Oncol. 1986;4(8):1162–70.
Liutkauskiene S, Janciauskiene R, Jureniene K, Grizas S, Malonyte R, Juozaityte E. Retrospective analysis of the impact of platinum dose reduction and chemotherapy delays on the outcomes of stage III ovarian cancer patients. BMC Cancer. 2015;15(1):105.
Budman DR, Berry DA, Cirrincione CT, Henderson IC, Wood WC, Weiss RB, et al. Dose and dose intensity as determinants of outcome in the adjuvant treatment of breast cancer. JNCI J Natl Cancer Inst. 1998;90(16):1205–11.
Edge SB, Compton CC. The American joint committee on cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010;17(6):1471–4.
Krigel RL, Palackdharry CS, Padavic K, Haas N, Kilpatrick D, Langer C, et al. Ifosfamide, carboplatin, and etoposide plus granulocyte-macrophage colony-stimulating factor: a phase I study with apparent activity in non-small-cell lung cancer. J Clin Oncol. 1994;12(6):1251–8.
Elias A, Ryan L, Aisner J, Antman KH, editors. Mesna, doxorubicin, ifosfamide, dacarbazine (MAID) regimen for adults with advanced sarcoma. In: Seminars in oncology; 1990 (Vol. 17, pp. 41–49).
Veldhuis G, Willemse P, Beijnen J, Boonstra H, Piersma H, Van der Graaf W, et al. Paclitaxel, ifosfamide and cisplatin with granulocyte colony-stimulating factor or recombinant human interleukin 3 and granulocyte colony-stimulating factor in ovarian cancer: a feasibility study. Br J Cancer. 1997;75(5):703.
Schütte J, Mouridsen H, Stewart W, Santoro A, Van Oosterom A, Somers R, et al. Ifosfamide plus doxorubicin in previously untreated patients with advanced soft tissue sarcoma. Eur J Cancer Clin Oncol. 1990;26(5):558–61.
Fetting JH, Gray R, Fairclough DL, Smith TJ, Margolin KA, Citron ML, et al. Sixteen-week multidrug regimen versus cyclophosphamide, doxorubicin, and fluorouracil as adjuvant therapy for node-positive, receptor-negative breast cancer: an intergroup study. J Clin Oncol. 1998;16(7):2382–91.
Boni C, Cocconi G, Bisagni G, Ceci G, Peracchia G. Cisplatin and etoposide (VP-16) as a single regimen for small cell lung cancer a phase II trial. Cancer. 1989;63(4):638–42.
Keefe DM, Elting LS, Nguyen HT, Grunberg SM, Aprile G, Bonaventura A, et al. Risk and outcomes of chemotherapy-induced diarrhea (CID) among patients with colorectal cancer receiving multi-cycle chemotherapy. Cancer Chemother Pharmacol. 2014;74(4):675–80.
American Society of Clinical Oncology. Recommendations for the use of hematopoietic colony-stimulating factors: evidence-based, clinical practice guidelines. J Clin Oncol. 1994;12(11):2471–508.
Motzer RJ, Geller NL, Bosl GJ. The effect of a 7-day delay in chemotherapy cycles on complete response and event-free survival in good-risk disseminated germ cell tumor patients. Cancer. 1990;66(5):857–61.
Wu Y, Aravind S, Nalysnyk L, Ranganathan G. Dose delay amongst cancer patients undergoing chemotherapy. Am Soc Hematol. 2008.
Denduluri N, Lyman GH, Wang Y, Morrow PK, Barron R, Patt D, et al. Chemotherapy dose intensity and overall survival among patients with advanced breast or ovarian cancer. Clin Breast Cancer. 2018;18(5):380–6.
Stitzenberg KB, Sigurdson ER, Egleston BL, Starkey RB, Meropol NJ. Centralization of cancer surgery: implications for patient access to optimal care. J Clin Oncol. 2009;27(28):4671.
Schraa S, Frerichs K, Agterof M, Hunting J, Los M, de Jong P. Relative dose intensity as a proxy measure of quality and prognosis in adjuvant chemotherapy for breast cancer in daily clinical practice. Eur J Cancer. 2017;79:152–7.
Lyman GH. Impact of chemotherapy dose intensity on cancer patient outcomes. J Natl Compr Canc Netw. 2009;7(1):99–108.
Griffin DA, Penprase B, Klamerus JF, editors. Relative dose intensity–improving treatment and outcomes in early-stage breast cancer: a retrospective study. In: Oncology nursing forum; 2012.
Faustino C, Afonso N, Sousa B, Santo JE, Rodrigues H. Relative dose intensity reduction in breast cancer adjuvant chemotherapy. AACR; 2009.
Egwuonwu O, Anyanwu S, Nwofor A. Default from neoadjuvant chemotherapy in premenopausal female breast cancer patients: what is to blame? Nigerian J Clin Pract. 2012;15(3):265–9.
Steward W, Vantongelen K, Verweij J, Thomas D, Van Oosterom A. Chemotherapy administration and data collection in an EORTC collaborative group—can we trust the results? Eur J Cancer. 1993;29(7):943–7.
Chang J. Chemotherapy dose reduction and delay in clinical practice: evaluating the risk to patient outcome in adjuvant chemotherapy for breast cancer. Eur J Cancer. 2000;36:11–4.
Scoggins JF, Fedorenko CR, Donahue SM, Buchwald D, Blough DK, Ramsey SD. Is distance to provider a barrier to care for medicaid patients with breast, colorectal, or lung cancer? J Rural Health. 2012;28(1):54–62.
Guidry JJ, Aday LA, Zhang D, Winn RJ. Transportation as a barrier to cancer treatment. Cancer Pract. 1997;5(6):361–6.
Salloum RG, Smith TJ, Jensen GA, Lafata JE. Factors associated with adherence to chemotherapy guidelines in patients with non-small cell lung cancer. Lung Cancer. 2012;75(2):255–60.
Liutkauskiene S, Grizas S, Jureniene K, Suipyte J, Statnickaite A, Juozaityte E. Retrospective analysis of the impact of anthracycline dose reduction and chemotherapy delays on the outcomes of early breast cancer molecular subtypes. BMC Cancer. 2018;18(1):453.
Wood WC, Budman DR, Korzun AH, Cooper MR, Younger J, Hart RD, et al. Dose and dose intensity of adjuvant chemotherapy for stage II, node-positive breast carcinoma. N Engl J Med. 1994;330(18):1253–9.
Savarese D, Hsieh CC, Stewart FM. Clinical impact of chemotherapy dose escalation in patients with hematologic malignancies and solid tumors. J Clin Oncol. 1997;15(8):2981–95.
Bonadonna G, Valagussa P, Moliterni A, Zambetti M, Brambilla C. Adjuvant cyclophosphamide, methotrexate, and fluorouracil in node-positive breast cancer—the results of 20 years of follow-up. N Engl J Med. 1995;332(14):901–6.
Hryniuk W, Bush H. The importance of dose intensity in chemotherapy of metastatic breast cancer. J Clin Oncol. 1984;2(11):1281–8.
Lepage E, Gisselbrecht C, Haioun C, Sebban C, Tilly H, Bosly A, et al. Prognostic significance of received relative dose intensity in non-Hodgkin’s lymphoma patients: application to LNH-87 protocol. Ann Oncol. 1993;4(8):651–6.
Henderson I, Hayes DF, Gelman R. Dose-response in the treatment of breast cancer: a critical review. J Clin Oncol. 1988;6(9):1501–15.
Seebacher V, Reinthaller A, Koelbl H, Concin N, Nehoda R, Polterauer S. The Impact of the Duration of Adjuvant Chemotherapy on Survival in Patients with Epithelial Ovarian Cancer - A Retrospective Study. PLoS One. 2017;12(1):e0169272-e.
Chirivella I, Bermejo B, Insa A, Pérez-Fidalgo A, Magro A, Rosello S, et al. Optimal delivery of anthracycline-based chemotherapy in the adjuvant setting improves outcome of breast cancer patients. Breast Cancer Res Treat. 2009;114(3):479–84.
Arriagada R, Le Chevalier T, Pignon J-P, Riviere A, Monnet I, Chomy P, et al. Initial chemotherapeutic doses and survival in patients with limited small-cell lung cancer. N Engl J Med. 1993;329(25):1848–52.
Kaye S, Paul J, Cassidy J, Lewis C, Duncan I, Gordon H, et al. Mature results of a randomized trial of two doses of cisplatin for the treatment of ovarian cancer. Scottish Gynecology Cancer Trials Group. Journal of clinical oncology. 1996;14(7):2113-9.
Cox JD, Pajak TF, Asbell S, Russell AH, Pederson J, Byhardt RW, et al. Interruptions of high-dose radiation therapy decrease longterm survival of favorable patients with unresectable nonsmall cell carcinoma of the lung: analysis of 1244 cases from 3 radiation therapy oncology group (RTOG) trials. Int J Radiat Oncol Biol Phys. 1993;27(3):493-8.
Acknowledgements
Our study group would like to thank Director General, Ministry of Health Malaysia for approval to publish this research, Clinical Research Centre (Biostatistics & Data Repository Sector), the National Institute of Health, Setia Alam for the data linkage service, and the National Registration Department (JPN) for their willingness to share their mortality records for research purposes.
Funding
This study and manuscript were not funded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gunasekaran, G.H., Hassali, M.A.B.A., Sabri, W.M.A.B.W. et al. Impact of chemotherapy schedule modification on breast cancer patients: a single-centre retrospective study. Int J Clin Pharm 42, 642–651 (2020). https://doi.org/10.1007/s11096-020-01011-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-020-01011-6