Abstract
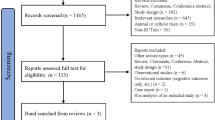
Background Valproate is a widely prescribed antiepileptic drug for generalized epilepsies, due to the extensive knowledge on its efficacy since it is on the market for many decades. However, a large number of new antiepileptic medicines was introduced into clinical practice and may be better options for treatment, considering that these medicines differ in terms of efficacy spectrum. Despite extensive research, questions regarding which medicine would constitute the first option for the monotherapy treatment of generalized epilepsy remain. Aim of the Review To compare the relative efficacy of all available antiepileptic drugs in the monotherapy treatment of generalized epileptic seizures; and also to compare all antiepoileptig drugs with valproate, which is the current first-line treatment for generalized epilepsy. Methods A systematic review for randomized controlled clinical trials was performed. Network meta-analyses used Bayesian random effects model. Sensitivity analyses determined the results´ robustness. The relative probability of two efficacy outcomes (“Seizure free” and “Therapeutic inefficacy”) to happen for each medcicine was calculated using the Surface Under the Cumulative Ranking Curve. Results Seven papers (1809 patients) studied the efficacy of valproate, lamotrigine, phenytoin, carbamazepine, topiramate, levetiracetam, and phenobarbital in the treatment of generalized tonicclonic, tonic, and clonic seizures. Phenytoin demonstrated to be inferior to valproate in leaving the patient free of these seizures types [OR: 0.50 (95% CrI 0.27, 0.87)]. Lamotrigine (61%) showed the highest probability of presenting the outcome “Seizure free”, followed by levetiracetam (47%), topiramate (44%), and valproate (38%) in the treatment of generalized tonic–clonic, tonic, and clonic seizures. Meanwhile, valproate exhibited greater chance of presenting the outcome “Therapeutic inefficacy” (62%). Regarding absence seizures itself, there was no difference in the efficacy of lamotrigine and ethosuximide when compared to valproate. However, the ranking indicates that ethosuximide (52%) and valproate (47%) are both more likely than lamotrigine to keep the patient free of seizures. Conclusions Lamotrigine, levetiracetam, and topiramate are as effective as valproate for treating generalized tonic–clonic, tonic, and clonic seizures. Meanwhile, valproate and ethosuximide are the best options for the treatment of absence seizures promoting better control of seizures, which is the primary goal of pharmacotherapy.





Similar content being viewed by others
References
Ngugi AK, Bottomley C, Kleinschmidt I, Sander JW, Newton CR. Estimation of the burden of active and life-time epilepsy: a meta-analytic approach. Epilepsia. 2010;51(5):883–90.
Shorvon SD. Epidemiology, classification, natural history, and genetics of epilepsy. Lancet. 1990;336:93–6.
Lhatoo SD, Johnson AL, Goodridge DM, MacDonald BK, Sander JW, Shorvon SD. Mortality in epilepsy in the first 11–14 years after diagnosis: multivariate analysis of a long-term, prospective, population-based cohort. Ann Neurol. 2001;49(3):336–44.
Rugg-Gunn FJ, Sander JW. Management of chronic epilepsy. BMJ. 2012;345:1–7.
Perucca E, Beghi E, Dulac O, Shorvon S, Tomson T. Assessing risk to benefit ratio in antiepileptic drug therapy. Epilepsy Res. 2000;41(2):107–39.
Kwan P, Brodie MJ. Early identification of refractory epilepsy. N Engl J Med. 2000;342(5):314–9.
Sirven JI, Noe K, Hoerth M, Drazkowski J. Antiepileptic drugs 2012: recent advances and trends. Mayo Clin Proc. 2012;87(9):879–89.
Shorvon SD, Perucca E, Enge J. Handbook of epilepsy treatment. 3a Edição. United Kingdom: Wiley-Blackwell; 2010. ISBN 978-1-4051-9818-9.
Mattson RH. Medical management of epilepsy in adults. Neurology. 1998;51(5):15–20.
Emilio P, Torbjörn T. The pharmacological treatment of epilepsy in adults. Lancet Neurol. 2011;10:446–56.
Savi MGM, Silva EL. Information flow in the clinical practice of resident physicians: an analysis from an evidence-based medicine perspective. Ciência Inf. 2009;38(3):177–91.
Higgins JPT, Thompson SG. Cochrane handbook for systematic reviews of interventions, Version 5.1.0. The Cochrane Collaboration, 2011. www.cochrane-handbook.org. Accessed 1 May 2015.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(6):e1000097.
Glauser T, Ben-Menachem E, Bourgeois B, Cnaan A, Chadwick D, Guerreiro C, et al. ILAE treatment guidelines: evidence-based analysis of antiepileptic drug efficacy and effectiveness as initial monotherapy for epileptic seizures and syndromes. Epilepsia. 2006;47(7):1094–120.
Harbord RM, Egger M, Sterne JC. A modified test for small-study effects in meta-analyses of controlled trials with binary endpoints. Stat Med. 2005;25(20):3443–57.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–74.
Cipriani A, Higgins JP, Geddes JR, Salanti G. Conceptual and technical challenges in network meta-analysis. Ann Intern Med. 2013;159(2):130–7.
Lu G, Ades AE. Combination of direct and indirect evidence in mixed treatment comparisons. Stat Med. 2004;23:3105–24.
Dias S, Welton NJ, Caldwell DM, Ades AE. Checking consistency in mixed treatment comparison meta-analysis. Stat Med. 2010;29(7–8):932–44.
Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. 2011;64(2):163–71.
Lau J, Ioannidis JPA, Schmid CH. Quantitative syntesis in systematic reviews. Ann Intern Med. 1997;127(9):820–6.
Brodie MJ, Richens A, Yuen AW. Double-blind comparison of lamotrigine and carbamazepine in newly diagnosed epilepsy. Lancet. 1995;345(8948):476–9.
Callaghan N, O’Hare J, O’Driscoll D, O’Neill B, Daly M. Comparative study of ethosuximide and sodium valproate in the treatment of typical absence seizures (petit mal). Dev Med Child Neurol. 1982;24(6):830–6.
Callaghan N, Kenny RA, O’Neill B, Crowley M, Goggin T. A prospective study between carbamazepine, phenytoin and sodium valproate as monotherapy in previously untreated and recently diagnosed patients with epilepsy. J Neurol Neurosurg Psychiatry. 1985;48(7):639–44.
Coppola G, Auricchio G, Federico R, Carotenuto M, Pascotto A. Lamotrigine versus valproic acid as first-line monotherapy in newly diagnosed typical absence seizures: an open-label, randomized, parallel-group study. Epilepsia. 2004;45(9):1049–53.
Frank LM, Enlow T, Holmes GL, Manasco P, Concannon S, Chen C, et al. Lamictal (lamotrigine) monotherapy for typical absence seizures in children. Epilepsia. 1999;40(7):973–9.
Glauser TA, Cnaan A, Shinnar S, Hirtz DG, Dlugos D, Masur D, et al. Ethosuximide, valproic acid, and lamotrigine in childhood absence epilepsy: initial monotherapy outcomes at 12 months. Epilepsia. 2013;54(1):141–55.
Marson AG, Al-Kharusi AM, Alwaidh M, Appleton R, Baker GA, Chadwick DW, et al. The SANAD study of effectiveness of valproate, lamotrigine, or topiramate for generalised and unclassifiable epilepsy: an unblinded randomised controlled trial. Lancet. 2007;369(9566):1016–26.
Ramsay RE, Wilder BJ, Murphy JV, Holmes GL, Uthman B, Slateret J, et al. Efficacy and safety of valproic acid versus phenytoin as sole therapy for newly diagnosed primary generalized tonic-clonic seizures. J Epilepsy. 1992;5(1):55–60.
Rastogi P, Mehrotra TN, Agarwala RK, Singh VS. Comparison of sodium valproate and phenytoin as single drug treatment in generalised and partial epilepsy. J Assoc Physicians India. 1991;39(8):606–8.
Richens A, Davidson DL, Cartlidge NE, Easter DJ. A multicentre comparative trial of sodium valproate and carbamazepine in adult onset epilepsy. Adult EPITEG Collaborative Group. J Neurol Neurosurg Psychiatry. 1994;57(6):682–7.
Steiner TJ, Dellaportas CI, Findley LJ, Gross M, Gibberd FB, Perkin GD, et al. Lamotrigine monotherapy in newly diagnosed untreated epilepsy: a double-blind comparison with phenytoin. Epilepsia. 1999;40(5):601–7.
Steinhoff BJ, Ueberall MA, Siemes H, Kurlemann G, Schmitz B, Bergmann L. The LAM-SAFE Study: lamotrigine versus carbamazepine or valproic acid in newly diagnosed focal and generalised epilepsies in adolescents and adults. Seizure. 2005;14(8):597–605.
Thilothammal N, Banu K, Ratnam RS. Comparison of phenobarbitone, phenytoin with sodium valproate: randomized, double-blind study. Indian Pediatr. 1996;33(7):549–55.
Trinka E, Marson AG, Van Paesschen W, Kälviäinen R, Marovac J, Duncan B, et al. KOMET: an unblinded, randomised, two parallel-group, stratified trial comparing the effectiveness of levetiracetam with controlled-release carbamazepine and extended-release sodium valproate as monotherapy in patients with newly diagnosed epilepsy. J Neurol Neurosurg Psychiatry. 2013;84(10):1138–47.
Turnbull DM, Howel D, Rawlins MD, Chadwick DW. Which drug for the adult epileptic patient: phenytoin or valproate? Br Med J (Clin Res Ed). 1985;290(6471):815–9.
Wilder BJ, Ramsay RE, Murphy JV, Karas BJ, Marquardt K, Hammond EJ. Comparison of valproic acid and phenytoin in newly diagnosed tonic-clonic seizures. Neurology. 1983;33(11):1474–6.
Bandstra NF, Camfield CS, Camfield PR. Stigma of epilepsy. Can J Neurol Sci. 2008;35(4):436–40.
Campos MSA, Ayres LR, Morelo MR, Marques FA, Pereira LR. Efficacy and tolerability of antiepileptic drugs in patients with focal epilepsy: systematic review and network meta-analyses. Pharmacotherapy. 2016;36(12):1255–71.
Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. 2011;64(2):163–71.
Sato S, White BG, Penry JK, Dreifuss FE, Sackellares JC, Kupferberg HJ. Valproate versus ethosuximide in the treatment of absence seizures. Neurology. 1982;32:157–63.
Glauser T, Ben-Menachem E, Bourgeois B, Cnaan A, Guerreiro C, Kälviäinen R, et al. Updated ILAE evidence review of antiepileptic drug efficacy and effectiveness as initial monotherapy for epileptic seizures and syndromes. Epilepsia. 2013;54(3):551–63.
Funding
No funding was received in support of this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Campos, M.S.d.A., Ayres, L.R., Morelo, M.R.S. et al. Comparative efficacy of antiepileptic drugs for patients with generalized epileptic seizures: systematic review and network meta-analyses. Int J Clin Pharm 40, 589–598 (2018). https://doi.org/10.1007/s11096-018-0641-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-018-0641-9