Abstract
Background Due to recent EU warnings and restrictions on the combined use of renin-angiotensin-aldosterone system (RAAS)-acting agents, and the seriousness of the associated harm, we analyzed the prescription of angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin receptor blockers (ARBs) as dual therapy or associated with spironolactone. Setting An administrative claims database of a regional hospital in Romania. Methods We retrospectively included all adult patients hospitalized during 18 months in 2013–2014, discharged with a prescription of a RAAS-acting agent. Main outcome measures Counts of ACEIs and ARBs co-prescription, of ACEIs or ARBs combined with spironolactone, co-morbidities, co-medication, creatinine, and electrolytes assessment and values. Results Out of 1697 patients with a prescription of a RAAS-acting agent, 24 (1.4 %) were co-prescribed ACEIs and ARBs, and 416 (24.5 %) ACEIs or ARBs with spironolactone. Patients prescribed dual ACEI/ARB therapy and the ones with ACEI or ARB-spironolactone combination had significantly higher prevalence of increased creatinine level before discharge, compared to the ACEI and ARB monotherapy groups (48 and 31 % compared to 17 and 27 %). Subjects with diabetes, heart failure, ischaemic heart disease, or urea ≥40 mg/dL had higher odds of having ACEI or ARB-spironolactone combination compared to monotherapy, while hypertension and renal disease subjects had lower odds. Similar findings were comparing dual ACEI/ARB therapy to monotherapy except heart failure (not statistically significant). Conclusion Overall, the prevalence of use of dual therapy was low. The combined use of RAAS-acting agents was higher in patients with known risk factors for further renal function deterioration, compared to the ones without.
Similar content being viewed by others
References
The SOLVD Investigators. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med. 1991;325(5):293–302.
Garg R, Yusuf S. Overview of randomized trials of angiotensin-converting enzyme inhibitors on mortality and morbidity in patients with heart failure. Collaborative Group on ACE Inhibitor Trials. JAMA. 1995;273(18):1450–6.
Pitt B, Poole-Wilson PA, Segal R, Martinez FA, Dickstein K, Camm AJ, et al. Effect of losartan compared with captopril on mortality in patients with symptomatic heart failure: randomised trial—the Losartan Heart Failure Survival Study ELITE II. Lancet. 2000;355:1582–7.
Pfeffer MA, Swedberg K, Granger CB, Held P, McMurray JJ, Michelson EL, et al. Effects of candesartan on mortality and morbidity in patients with chronic heart failure: the CHARM-Overall programme. Lancet. 2003;362:759–66.
Dickstein K, Cohen-Solal A, Filippatos G, McMurray JJ, Ponikowski P, Poole-Wilson PA, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur Heart J. 2008;29(19):2388–442.
American Diabetes Association. Standards of medical care in diabetes–2012. Diabetes Care. 2012;35(Suppl 1):S11–63.
Yusuf S, Teo KK, Pogue J, Dyal L, Copland I, Schumacher H, et al. (ONTARGET Investigators). Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med. 2008;358(15):1547–59.
Fried LF, Emanuele N, Zhang JH, Brophy M, Conner TA, Duckworth W, et al. (VA NEPHRON-D Investigators). Combined angiotensin inhibition for the treatment of diabetic nephropathy. N Engl J Med. 2013;369(20):1892–903.
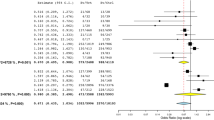
Makani H, Bangalore S, Desouza KA, Shah A, Messerli FH. Efficacy and safety of dual blockade of the renin-angiotensin system: meta-analysis of randomised trials. BMJ. 2013;346:f360. doi:10.1136/bmj.f360.
Restriction of combined use of medicines affecting the renin-angiotensin system (RAS). EMA/554928/2014. http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/referrals/Renin-angiotensin_system_(RAS)-acting_agents/human_referral_prac_000026.jsp&mid=WC0b01ac05805c516f.
Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized aldactone evaluation study investigators. N Engl J Med. 1999;341:709–17.
Wei L, Struthers AD, Fahey T, Watson AD, Macdonald TM. Spironolactone use and renal toxicity: population based longitudinal analysis. BMJ. 2010;340:c1768.
Svensson M, Gustafsson F, Galatius S, Hildebrandt PR, Atar D. How prevalent is hyperkalemia and renal dysfunction during treatment with spironolactone in patients with congestive heart failure? J Card Fail. 2004;10:297–303.
Bilotta C, Franchi C, Nobili A, Nicolini P, Djade CD, Tettamanti M, et al. New prescriptions of spironolactone associated with angiotensin-converting-enzyme inhibitors and/or angiotensin receptor blockers and their laboratory monitoring from 2001 to 2008: a population study on older people living in the community in Italy. Eur J Clin Pharmacol. 2013;69(4):909–17.
Shah KB, Rao K, Sawyer R, Gottlieb SS. The adequacy of laboratory monitoring in patients treated with spironolactone for congestive heart failure. J Am Coll Cardiol. 2005;46(5):845–9.
Wang PT, Huang YB, Lin MY, Chuang PF, Hwang SJ. Prescriptions for angiotensin-converting enzyme inhibitors/angiotensin receptor blockers and monitoring of serum creatinine and potassium in patients with chronic kidney disease. Kaohsiung J Med Sci. 2012;28(9):477–83.
R Core Team. R: A language and environment for statistical computing [Internet]. Vienna, Austria; 2015. http://www.r-project.org.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34(28):2159–219.
Trends in co-prescribing of renin-angiotensin system (RAS)—acting agents in France, Germany and the UK during 2001–2012. EMA drug utilisation study using IMS Health electronic health records. http://www.encepp.eu/encepp/viewResource.htm?id=4617 Accessed Apr 15 2015.
McAlister FA, Zhang J, Tonelli M, Klarenbach S, Manns BJ, Hemmelgarn BR, et al. The safety of combining angiotensin-converting-enzyme inhibitors with angiotensin-receptor blockers in elderly patients: a population-based longitudinal analysis. CMAJ. 2011;183(6):655–62.
Werner C, Pöss J, Böhm M. Optimal antagonism of the Renin-Angiotensin-aldosterone system: do we need dual or triple therapy? Drugs. 2010;70(10):1215–30.
Goland S, Naugolny V, Korbut Z, Rozen I, Caspi A, Malnick S. Appropriateness and complications of the use of spironolactone in patients treated in a heart failure clinic. Eur J Intern Med. 2011;22(4):424–7.
Kurnik D, Vesterman-Landes J, Bialik M, Katzir I, Lomnicky Y, Halkin H, et al. Hyperkalemia and renal function during monotherapy and dual renin-angiotensin blockade in the community setting. Clin Ther. 2011;33(4):456–64.
Bakris GL, Weir MR. Angiotensin-converting enzyme inhibitor-associated elevations in serum creatinine: is this a cause for concern? Arch Intern Med. 2000;160(5):685–93.
Spironolactone and renin-angiotensin system drugs in heart failure: risk of potentially fatal hyperkalaemia. Drug Safety Update volume 9 issue 6 February 2016: 2. https://www.gov.uk/drug-safety-update/spironolactone-and-renin-angiotensin-system-drugs-in-heart-failure-risk-of-potentially-fatal-hyperkalaemia Accessed Feb 18 2016.
Funding
This paper was published under the frame of European Social Fund, Human Resources Development Operational Programme 2007–2013, Project No. POSDRU/159/1.5/136893. The funding source had no involvement in the conduct of the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
All authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Farcas, A., Leucuta, D., Bucsa, C. et al. Combined use of renin-angiotensin-aldosterone system-acting agents: a cross-sectional study. Int J Clin Pharm 38, 1390–1397 (2016). https://doi.org/10.1007/s11096-016-0378-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-016-0378-2