Abstract
Purpose
The differences between intestinal and systemic (hepatic and renal) P-glycoprotein (P-gp) and breast cancer resistance protein (BCRP) roles in drug disposition are difficult to define. Accordingly, we characterized Encequidar (ECD) as an intestinal P-gp and BCRP specific inhibitor to evaluate their role in drug disposition.
Methods
We assessed the in vitro and in vivo inhibition potential of ECD towards human and animal P-gp and BCRP.
Results
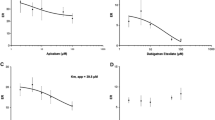
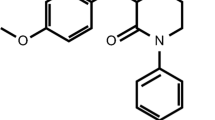
ECD is a potent inhibitor with a high degree of selectivity in inhibiting human P-gp (hP-gp) over human BCRP (hBCRP) (IC50s of 0.0058 ± 0.0006 vs. > 10 µM, respectively). In contrast, ECD is a potent inhibitor of rat and cynomolgus monkey BCRP (IC50 ranged from 0.059 to 0.18 µM). While the AUC of IV paclitaxel (PTX) was significantly increased by elacridar (ELD) (P < 0.05) but not ECD in rats (15 mg/kg; PO) (2.55- vs. 0.93-fold), that of PO PTX was significantly elevated to a similar extent between the inhibitors (39.5- vs. 33.5-fold). Similarly, the AUC of PO sulfasalazine (SFZ) was dramatically increased by ELD and ECD (16.6- vs. 3.04-fold) although that of IV SFZ was not significantly affected by ELD and ECD in rats (1.18- vs. 1.06-fold). Finally, a comparable ECD-induced increase of the AUC of PO talinolol in cynomolgus monkeys was observed compared with ELD (2.14- vs. 2.12-fold).
Conclusions
ECD may allow an in-depth appraisal of the role of intestinal efflux transporter(s) in drug disposition in animals and humans through local intestinal drug interactions.





Similar content being viewed by others
Data availability
Upon request, and subject to review, Bristol Myers Squibb Company will provide the data that support the findings of this study.
Abbreviations
- A-to-B:
-
Apical to basolateral direction
- AMP:
-
Adenosine 5’-monophosphate
- ATP:
-
Adenosine 5’-triphosphate
- AUC :
-
Area under the plasma concentration–time curve
- B-to-A:
-
Basolateral to apical direction
- BCRP:
-
Breast cancer resistance protein
- C max :
-
Total maximal concentration in plasma
- C max,u :
-
Unbound maximal concentration in plasma
- DDI:
-
Drug-drug interaction
- HBSS:
-
Hanks’ balanced salt solution
- ECD:
-
Encequidar
- ELD:
-
Elacridar
- ER:
-
Efflux ratio
- FDA:
-
The United States Food and Drug Administration
- IC 50 :
-
Half-maximal inhibitory concentration
- I gut :
-
Maximum expected concentration in the intestinal lumen estimated as dose/250 mL
- LC–MS/MS:
-
Liquid chromatography–tandem mass spectrometry
- MDCK:
-
Madin-Darby canine kidney cell
- MDR:
-
Multidrug resistance protein
- MRP:
-
Multidrug resistance-associated protein
- P-gp:
-
P-glycoprotein
- PTX:
-
Paclitaxel
- SFZ:
-
Sulfasalazine
- SRM:
-
Selective reaction monitoring
- TLN:
-
Talinolol
- T max :
-
Time when peak plasma concentration occurs
References
Juliano RL, Ling V. A surface glycoprotein modulating drug permeability in Chinese hamster ovary cell mutants. Biochem Biophys Acta. 1976;455(1):152–62.
Doyle LA, Yang W, Abruzzo LV, Krogmann T, Gao Y, Rishi AK, et al. A multidrug resistance transporter from human MCF-7 breast cancer cells. Proc Natl Acad Sci U S A. 1998;95(26):15665–70.
Thiebaut F, Tsuruo T, Hamada H, Gottesman MM, Pastan I, Willingham MC. Cellular localization of the multidrug-resistance gene product P-glycoprotein in normal human tissues. Proc Natl Acad Sci U S A. 1987;84(21):7735–8.
Maliepaard M, Scheffer GL, Faneyte IF, van Gastelen MA, Pijnenborg AC, Schinkel AH, et al. Subcellular localization and distribution of the breast cancer resistance protein transporter in normal human tissues. Cancer Res. 2001;61(8):3458–64.
Drozdzik M, Busch D, Lapczuk J, Muller J, Ostrowski M, Kurzawski M, et al. Protein Abundance of Clinically Relevant Drug Transporters in the Human Liver and Intestine: A Comparative Analysis in Paired Tissue Specimens. Clin Pharmacol Ther. 2019;105(5):1204–12.
Chatterjee S, Deshpande AA, Shen H. Recent advances in the in vitro and in vivo methods to assess impact of P-glycoprotein and breast cancer resistance protein transporters in central nervous system drug disposition. Biopharm & Drug Disp. 2023;44(1):7–25.
Tanigawara Y. Role of P-glycoprotein in drug disposition. Ther Drug Monit. 2000;22(1):137–40.
Breedveld P, Beijnen JH, Schellens JH. Use of P-glycoprotein and BCRP inhibitors to improve oral bioavailability and CNS penetration of anticancer drugs. Trends Pharmacol Sci. 2006;27(1):17–24.
Lund M, Petersen TS, Dalhoff KP. Clinical Implications of P-Glycoprotein Modulation in Drug-Drug Interactions. Drugs. 2017;77(8):859–83.
Lee CA, O’Connor MA, Ritchie TK, Galetin A, Cook JA, Ragueneau-Majlessi I, et al. Breast cancer resistance protein (ABCG2) in clinical pharmacokinetics and drug interactions: practical recommendations for clinical victim and perpetrator drug-drug interaction study design. Drug Metab Dispos Biol Fate Chem. 2015;43(4):490–509.
Taskar KS, Yang X, Neuhoff S, Patel M, Yoshida K, Paine MF, et al. Clinical Relevance of Hepatic and Renal P-gp/BCRP Inhibition of Drugs: An International Transporter Consortium Perspective. Clin Pharmacol Ther. 2022;112(3):573–92.
Kwak JO, Lee SH, Lee GS, Kim MS, Ahn YG, Lee JH, et al. Selective inhibition of MDR1 (ABCB1) by HM30181 increases oral bioavailability and therapeutic efficacy of paclitaxel. Eur J Pharmacol. 2010;627(1–3):92–8.
Smolinski MP, Urgaonkar S, Pitzonka L, Cutler M, Lee G, Suh KH, et al. Discovery of Encequidar, First-in-Class Intestine Specific P-glycoprotein Inhibitor. J Med Chem. 2021;64(7):3677–93.
Jackson C, Hung T, Segelov E, Barlow P, Prenen H, McLaren B, et al. Oral paclitaxel with encequidar compared to intravenous paclitaxel in patients with advanced cancer: A randomised crossover pharmacokinetic study. Br J Clin Pharmacol. 2021;87(12):4670–80.
Rautio J, Humphreys JE, Webster LO, Balakrishnan A, Keogh JP, Kunta JR, et al. In vitro p-glycoprotein inhibition assays for assessment of clinical drug interaction potential of new drug candidates: a recommendation for probe substrates. Drug Metab Dispos Biol Fate Chem. 2006;34(5):786–92.
Kim TE, Lee H, Lim KS, Lee S, Yoon SH, Park KM, et al. Effects of HM30181, a P-glycoprotein inhibitor, on the pharmacokinetics and pharmacodynamics of loperamide in healthy volunteers. Br J Clin Pharmacol. 2014;78(3):556–64.
Schenck-Gustafsson K, Dahlqvist R. Pharmacokinetics of digoxin in patients subjected to the quinidine-digoxin interaction. Br J Clin Pharmacol. 1981;11(2):181–6.
Cha YJ, Lee H, Gu N, Kim TE, Lim KS, Yoon SH, et al. Sustained Increase in the Oral Bioavailability of Loperamide after a Single Oral Dose of HM30181, a P-glycoprotein Inhibitor, in Healthy Male Participants. Basic Clin Pharmacol Toxicol. 2013;113(6):419–24.
Rugo HS, Umanzor GA, Barrios FJ, Vasallo RH, Chivalan MA, Bejarano S, et al. Open-Label, Randomized, Multicenter, Phase III Study Comparing Oral Paclitaxel Plus Encequidar Versus Intravenous Paclitaxel in Patients With Metastatic Breast Cancer. J Clinic Oncol Offic J Am Soc Clin Oncol. 2023;41(1):65–74.
Ieiri I, Higuchi S, Sugiyama Y. Genetic polymorphisms of uptake (OATP1B1, 1B3) and efflux (MRP2, BCRP) transporters: implications for inter-individual differences in the pharmacokinetics and pharmacodynamics of statins and other clinically relevant drugs. Expert Opin Drug Metab Toxicol. 2009;5(7):703–29.
Zamek-Gliszczynski MJ, Bedwell DW, Bao JQ, Higgins JW. Characterization of SAGE Mdr1a (P-gp), Bcrp, and Mrp2 knockout rats using loperamide, paclitaxel, sulfasalazine, and carboxydichlorofluorescein pharmacokinetics. Drug Metab Dispos Biol Fate Chem. 2012;40(9):1825–33.
Mease K, Sane R, Podila L, Taub ME. Differential selectivity of efflux transporter inhibitors in Caco-2 and MDCK-MDR1 monolayers: a strategy to assess the interaction of a new chemical entity with P-gp, BCRP, and MRP2. J Pharm Sci. 2012;101(5):1888–97.
Wang Q, Strab R, Kardos P, Ferguson C, Li J, Owen A, et al. Application and limitation of inhibitors in drug-transporter interactions studies. Int J Pharm. 2008;356(1–2):12–8.
Kosa RE, Lazzaro S, Bi YA, Tierney B, Gates D, Modi S, et al. Simultaneous Assessment of Transporter-Mediated Drug-Drug Interactions Using a Probe Drug Cocktail in Cynomolgus Monkey. Drug Metab Dispos Biol Fate Chem. 2018;46(8):1179–89.
Karibe T, Imaoka T, Abe K, Ando O. Curcumin as an In Vivo Selective Intestinal Breast Cancer Resistance Protein Inhibitor in Cynomolgus Monkeys. Drug Metab Dispos Biol Fate Chem. 2018;46(5):667–79.
Imai S, Arai T, Yamada T, Niwa M. Improved In Vitro-In Vivo Correlation by Using the Unbound-Fraction-Adjusted IC(50) for Breast Cancer Resistance Protein Inhibition. Pharm Res. 2020;37(12):230.
Kawahara I, Nishikawa S, Yamamoto A, Kono Y, Fujita T. The Impact of Breast Cancer Resistance Protein (BCRP/ABCG2) on Drug Transport Across Caco-2 Cell Monolayers. Drug Metab Dispos Biol Fate Chem. 2020;48(6):491–8.
Nozaki Y, Kusuhara H, Kondo T, Iwaki M, Shiroyanagi Y, Nakayama H, et al. Species difference in the inhibitory effect of nonsteroidal anti-inflammatory drugs on the uptake of methotrexate by human kidney slices. J Pharmacol Exp Ther. 2007;322(3):1162–70.
Chu X, Bleasby K, Evers R. Species differences in drug transporters and implications for translating preclinical findings to humans. Expert Opin Drug Metab Toxicol. 2013;9(3):237–52.
Gonzalez-Lobato L, Real R, Prieto JG, Alvarez AI, Merino G. Differential inhibition of murine Bcrp1/Abcg2 and human BCRP/ABCG2 by the mycotoxin fumitremorgin C. Eur J Pharmacol. 2010;644(1–3):41–8.
Ma WW, Li JJ, Azad NS, Lam ET, Diamond JR, Dy GK, et al. A phase Ib study of Oraxol (oral paclitaxel and encequidar) in patients with advanced malignancies. Cancer Chemother Pharmacol. 2022;90(1):7–17.
Zolnerciks JK, Booth-Genthe CL, Gupta A, Harris J, Unadkat JD. Substrate- and species-dependent inhibition of P-glycoprotein-mediated transport: implications for predicting in vivo drug interactions. J Pharm Sci. 2011;100(8):3055–61.
Suzuyama N, Katoh M, Takeuchi T, Yoshitomi S, Higuchi T, Asashi S, et al. Species differences of inhibitory effects on P-glycoprotein-mediated drug transport. J Pharm Sci. 2007;96(6):1609–18.
Urakami Y, Okuda M, Saito H, Inui K. Hormonal regulation of organic cation transporter OCT2 expression in rat kidney. FEBS Lett. 2000;473(2):173–6.
Urakami Y, Nakamura N, Takahashi K, Okuda M, Saito H, Hashimoto Y, et al. Gender differences in expression of organic cation transporter OCT2 in rat kidney. FEBS Lett. 1999;461(3):339–42.
Madla CM, Qin Y, Gavins FKH, Liu J, Dou L, Orlu M, et al. Sex Differences in Intestinal P-Glycoprotein Expression in Wistar versus Sprague Dawley Rats. Pharmaceutics. 2022;14(5):1030.
Matsson P, Pedersen JM, Norinder U, Bergstrom CA, Artursson P. Identification of novel specific and general inhibitors of the three major human ATP-binding cassette transporters P-gp, BCRP and MRP2 among registered drugs. Pharm Res. 2009;26(8):1816–31.
Zamek-Gliszczynski MJ, Sangha V, Shen H, Feng B, Wittwer MB, Varma MVS, et al. Transporters in Drug Development: International Transporter Consortium Update on Emerging Transporters of Clinical Importance. Clin Pharmacol Ther. 2022;112(3):485–500.
Acknowledgements
The authors thank Yueping Zhang (Bristol Myers Squibb Company) for help conducting some MDCK-hMDR1 and MDCK-hBCRP experiments.
Funding
This study was sponsored by Bristol Myers Squibb Company.
Author information
Authors and Affiliations
Contributions
Design of work: Chu, Panfen, Fancher, Shah, Xue, Sinz, and Shen.
Conduction of experiments: Chu, Panfen, Wang, Marino, Chen, Landage, Patil, and Desai.
Analysis and interpretation of data: Chu, Panfen, Marino, Sinz, and Shen.
Drafting and revising work: Chu, Panfen, Landage, Sinz, and Shen.
Corresponding author
Ethics declarations
Conflict of Interest
All authors are employees of either Bristol Myers Squibb Company or Biocon Bristol Myers Squibb R&D Centre, Syngene International Ltd.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chu, J., Panfen, E., Wang, L. et al. Evaluation of Encequidar as An Intestinal P-gp and BCRP Specific Inhibitor to Assess the Role of Intestinal P-gp and BCRP in Drug-Drug Interactions. Pharm Res 40, 2567–2584 (2023). https://doi.org/10.1007/s11095-023-03563-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-023-03563-4