Abstract
Purpose
This study evaluated the in vitro aerosol performance of a dry powder antibiotic product that combined a highly dispersible tobramycin powder with a previously optimized pediatric air-jet dry powder inhaler (DPI) across a subject age range of 2–10 years.
Methods
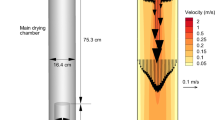
An excipient enhanced growth (EEG) formulation of the antibiotic tobramycin (Tobi) was prepared using a small particle spray drying technique that included mannitol as the hygroscopic excipient and trileucine as the dispersion enhancer. The Tobi-EEG formulation was aerosolized using a positive-pressure pediatric air-jet DPI that included a 3D rod array. Realistic in vitro experiments were conducted in representative airway models consistent with children in the age ranges of 2–3, 5–6 and 9–10 years using oral or nose-to-lung administration, non-humidified or humidified airway conditions, and constant or age-specific air volumes.
Results
Across all conditions tested, mouth-throat depositional loss was < 1% and nose-throat depositional loss was < 3% of loaded dose. Lung delivery efficiency was in the range of 77.3–85.1% of loaded dose with minor variations based on subject age (~ 8% absolute difference), oral or nasal administration (< 2%), and delivered air volume (< 2%). Humidified airway conditions had an insignificant impact on extrathoracic depositional loss and significantly increased aerosol size at the exit of a representative lung chamber.
Conclusions
In conclusion, the inhaled antibiotic product nearly eliminated extrathoracic depositional loss, demonstrated high efficiency nose-to-lung antibiotic aerosol delivery in pediatric airway models for the first time, and provided ~ 80% lung delivery efficiency with little variability across subject age and administered air volume.



Similar content being viewed by others
Abbreviations
- 3D:
-
Three-dimensional
- B#:
-
Bifurcation number
- CDC:
-
Centers for Disease Control and Prevention
- CFD:
-
Computational fluid dynamics
- DF:
-
Deposition fraction
- DPI:
-
Dry powder inhaler
- ED:
-
Emitted dose
- EEG:
-
Excipient enhanced growth
- FPF:
-
Fine particle fraction
- HP:
-
High performance
- HPLC:
-
High performance liquid chromatography
- LC–MS:
-
Liquid chromatography-mass spectrometry
- MMAD:
-
Mass median aerodynamic diameter
- MN:
-
Mannitol
- MP:
-
Mouthpiece
- MT:
-
Mouth-throat
- NGI:
-
Next Generation Impactor
- RH:
-
Relative humidity
- SD:
-
Standard deviation
- TB:
-
Tracheobronchial
- Tobi:
-
Tobramycin
- USP:
-
United States Pharmacopeia
References
Weers JG, Son Y-J, Glusker M, Haynes A, Huang D, Kadrichu N, Le J, Li X, Malcolmson R, Miller DP, Tarara TE, Ung K, Clark A. Idealhalers versus realhalers: Is it possible to bypass deposition in the upper respiratory tract? J Aerosol Med Pulm Drug Deliv. 2019;32:55–69.
De Boer A, Hagedoorn P, Hoppentocht M, Buttini F, Grasmeijer F, Frijlink H. Dry powder inhalation: past, present and future. Expert Opin Drug Deliv. 2017;14:499–512.
Islam N, Cleary MJ. Developing an efficient and reliable dry powder inhaler for pulmonary drug delivery - A review for multidisciplinary researchers. Med Eng Phys. 2012;34:409–27.
Lexmond AJ, Hagedoorn P, Frijlink HW, Rottier BL, de Boer AH. Prerequisites for a dry powder inhaler for children with cystic fibrosis. PLoS ONE. 2017;12: e0183130.
Lexmond AJ, Kruizinga TJ, Hagedoorn P, Rottier BL, Frijlink HW, De Boer AH. Effect of inhaler design variables on paediatric use of dry powder inhalers. PLoS ONE. 2014;9: e99304.
Everard ML. Inhaler devices in infants and children: Challenges and solutions. Journal of Aerosol Medicine-Deposition Clearance and Effects in the Lung. 2004;17:186–95.
Lindert S, Below A, Breitkreutz J. Performance of dry powder inhalers with single dosed capsules in preschool children and adults using improved upper airway models. Pharmaceutics. 2014;6:36–51.
Devadason S, Everard M, MacEarlan C, Roller C, Summers Q, Swift P, Borgstrom L, Le Souëf P. Lung deposition from the Turbuhaler in children with cystic fibrosis. Eur Respir J. 1997;10:2023–8.
Below A, Bickmann D, Breitkreutz J. Assessing the performance of two dry powder inhalers in preschool children using an idealized pediatric upper airway model. Int J Pharm. 2013;444:169–74.
Borgstrom L, Bengtsson T, Derom E, Pauwels R. Variability in lung deposition of inhlaed drug, within and between asthmatic patients, with a pMDI and a dry powder inhaler, Turbuhaler. International Journal of Pharmaceutics. 2000;193:227–30.
Borgstrom L, Olsson B, Thorsson L. Degree of throat deposition can explain the variability in lung deposition of inhaled drugs. J Aerosol Med. 2006;19:473–83.
Tiddens HA, Geller DE, Challoner P, Speirs RJ, Kesser KC, Overbeek SE, Humble D, Shrewsbury SB, Standaert TA. Effect of dry powder inhaler resistance on the inspiratory flow rates and volumes of cystic fibrosis patients of six years and older. Journal Of Aerosol Medicine-Deposition Clearance And Effects In The Lung. 2006;19:456–65.
Everard ML. Aerosol delivery in infants and young children. Journal of Aerosol Medicine-Deposition Clearance and Effects in the Lung. 1996;9:71–7.
Ruzycki CA, Golshahi L, Vehring R, Finlay WH. Comparison of in vitro deposition of pharmaceutical aerosols in an idealized child throat with in vivo deposition in the upper respiratory tract of children. Pharm Res. 2014;31:1525–35.
Golshahi L, Finlay WH. An idealized child throat that mimics average pediatric oropharyngeal deposition. Aerosol Sci Technol. 2012;46:i–iv.
Haynes A, Geller D, Weers J, Ament B, Pavkov R, Malcolmson R, Debonnett L, Mastoridis P, Yadao A, Heuerding S. Inhalation of tobramycin using simulated cystic fibrosis patient profiles. Pediatr Pulmonol. 2016;51:1159–67.
Rubin BK. Pediatric aerosol therapy: New devices and new drugs. Respir Care. 2011;56:1411–21.
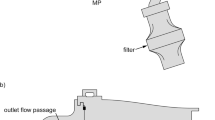
Farkas D, Hindle M, Bonasera S, Bass K, Longest W. Development of an inline dry powder inhaler for oral or trans-nasal aerosol administration to children. J Aerosol Med Pulm Drug Deliv. 2020;33:83–98.
Weers JG, Miller DP. Formulation design of dry powders for inhalation. J Pharm Sci. 2015;104:3259–88.
Son Y-J, Longest PW, Hindle M. Aerosolization characteristics of dry powder inhaler formulations for the excipient enhanced growth (EEG) application: Effect of spray drying process conditions on aerosol performance. Int J Pharm. 2013;443:137–45.
Feng A, Boraey M, Gwin M, Finlay P, Kuehl P, Vehring R. Mechanistic models facilitate efficient development of leucine containing microparticles for pulmonary drug delivery. Int J Pharm. 2011;409:156–63.
Vehring R. Pharmaceutical particle engineering via spray drying. Pharm Res. 2008;25:999–1022.
Vehring R, Foss WR, Lechuga-Ballesteros D. Particle formation in spray drying. J Aerosol Sci. 2007;38:728–46.
Hindle M, Longest PW. Condensational growth of combination drug-excipient submicrometer particles for targeted high efficiency pulmonary delivery: Evaluation of formulation and delivery device. J Pharm Pharmacol. 2012;64:1254–63.
Son Y-J, Longest PW, Tian G, Hindle M. Evaluation and modification of commercial dry powder inhalers for the aerosolization of submicrometer excipient enhanced growth (EEG) formulation. Eur J Pharm Sci. 2013;49:390–9.
Longest PW, Son Y-J, Holbrook LT, Hindle M. Aerodynamic factors responsible for the deaggregation of carrier-free drug powders to form micrometer and submicrometer aerosols. Pharm Res. 2013;30:1608–27.
Longest P, Farkas D, Hassan A, Hindle M. Computational fluid dynamics (CFD) simulations of spray drying: linking drying parameters with experimental aerosolization performance. Pharm Res. 2020;37:101–101.
Hassan A, Farkas D, Longest W, Hindle M. Characterization of excipient enhanced growth (EEG) tobramycin dry powder aerosol formulations. Int J Pharm. 2020;591: 120027.
Bonasera S. Formulation, characterization and pharmacokinetic modeliing of excipient enhanced growth spray-dried inhalation powders. Dissertation, Virginia Commonwealth University, Richmond, VA. 2021;
Farkas D, Bonasera S, Bass K, Hindle M, Longest PW. Advancement of a positive-pressure dry powder inhaler for children: use of a vertical aerosolization chamber and three-dimensional rod array interface. Pharm Res. 2020;37:177.
Farkas D, Hindle M, Longest PW. Development of an inline dry powder inhaler that requires low air volume. J Aerosol Med Pulm Drug Deliv. 2018;31:255–65.
Farkas D, Hindle M, Longest PW. Application of an inline dry powder inhaler to deliver high dose pharmaceutical aerosols during low flow nasal cannula therapy. Int J Pharm. 2018;546:1–9.
Farkas D, Hindle M, Longest PW. Efficient nose-to-lung aerosol delivery with an inline DPI requiring low actuation air volume. Pharm Res. 2018;35:194.
Bass K, Farkas D, Hassan A, Bonasera S, Hindle M, Longest W. High-efficiency dry powder aerosol delivery to children: Review and application of new technologies. J Aerosol Sci. 2021;153: 105692.
Geller DE, Weers J, Heuerding S. Development of an inhaled dry-powder formulation of Tobramycin using PulmoSphereTM technology. J Aerosol Med Pulm Drug Deliv. 2011;24:175–82.
Weers J. Inhaled antimicrobial therapy - Barriers to effective treatment. Adv Drug Deliv Rev. 2015;85:24–43.
Robertson JM, Friedman EM, Rubin BK. Nasal and sinus disease in cystic fibrosis. Paediatr Respir Rev. 2008;9:213–9.
Bonestroo HJ, de Winter-de Groot KM, van der Ent CK, Arets HG. Upper and lower airway cultures in children with cystic fibrosis: do not neglect the upper airways. J Cyst Fibros. 2010;9:130–4.
Sawicki GS, Sellers DE, Robinson WM. High treatment burden in adults with cyctic fibrosis: challenges to disease self-management. J Cyst Fibros. 2009;8:91–6.
Geller DE, Konstan MW, Smith J, Noonberg SB, Conrad C. Novel tobramycin inhalation powder in cystic fibrosis subjects: Pharmacokinetics and safety. Pediatr Pulmonol. 2007;42:307–13.
Bass K, Longest PW. Development of DPI patient interfaces for improved aerosol delivery to children. AAPS PharmSciTech. 2020;21:157.
Phalen RF, Oldham MJ, Beaucage CB, Crocker TT, Mortensen JD. Postnatal enlargement of human tracheobronchial airways and implications for particle deposition. Anat Rec. 1985;212:368–80.
Kuczmarski RJ. CDC growth charts: United States, US Department of Health and Human Services, Centers for Disease Control and …, 2000.
Wachtel H, Bickmann D, Breitkreutz J, Langguth P. Can pediatric throat models and air flow profiles improve our dose finding strategy. Respiratory Drug Delivery. 2010;2010:195–204.
Golshahi L, Noga ML, Finlay WH. Deposition of inhaled micrometer-sized particles in oropharyngeal airway replicas of children at constant flow rates. J Aerosol Sci. 2012;49:21–31.
DeHaan WH, Finlay WH. In vitro monodisperse aerosol deposition in a mouth and throat with six different inhalation devices. J Aerosol Med. 2001;14:361–7.
DeHaan WH, Finlay WH. Predicting extrathoracic deposition from dry powder inhalers. J Aerosol Sci. 2004;35:309–31.
Bickmann D, Wachtel H, Kroger R, Langguth P. Examining inhaler perforance using a child’s throat model. Respiratory Drug Delivery. 2008;2008:565–9.
Cheng YS. Aerosol deposition in the extrathoracic region. Aerosol Sci Technol. 2003;37:659–71.
Xi J, Longest PW. Transport and deposition of micro-aerosols in realistic and simplified models of the oral airway. Ann Biomed Eng. 2007;35:560–81.
Bass K, Farkas D, Longest W. Optimizing Aerosolization Using Computational Fluid Dynamics in a Pediatric Air-Jet Dry Powder Inhaler. AAPS PharmSciTech. 2019;20:329.
Rosenow T, Oudraad MCJ, Murray CP, Turkovic L, Kuo W, de Bruijne M, Ranganathan SC, Tiddens HAWM, and Stick SM. PRAGMA-CF. A quantitative structural lung disease computed tomography outcome in young children with cystic fibrosis. American Journal of Respiratory and Critical Care Medicine. 2015;191:1158–1165.
ICRP. Human respiratory tract model for radiological protection, Elsevier Science Ltd., New York, 1994.
Longest W, Hassan A, Farkas D, and Hindle M. Computational fluid dynamics (CFD) guided spray drying recommendations for improved aerosol performance of a small-particle antibiotic formulation. Pharm Res. 2022;https://doi.org/10.1007/s11095-022-03180-7
Chua H, Collis G, Newbury A, Chan K, Bower G, Sly P, Le Souef P. The influence of age on aerosol deposition in children with cystic fibrosis. Eur Respir J. 1994;7:2185–91.
Everard M, Hardy J, Milner A. Comparison of nebulised aerosol deposition in the lungs of healthy adults following oral and nasal inhalation. Thorax. 1993;48:1045–6.
Geller DE. Aerosol antibiotics in cystic fibrosis. Respir Care. 2004;54:658–70.
ACKNOWLEDGMENTS AND DISCLOSURES
Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number R01HD087339 and by the National Heart, Lung and Blood Institute of the National Institutes of Health under Award Number R01HL139673. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Author Disclosure Statement
Virginia Commonwealth University is currently pursuing patent protection of devices and methods described in this study, which if licensed and commercialized, may provide a future financial interest to the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Farkas, D., Thomas, M.L., Hassan, A. et al. Near Elimination of In Vitro Predicted Extrathoracic Aerosol Deposition in Children Using a Spray-Dried Antibiotic Formulation and Pediatric Air-Jet DPI. Pharm Res 40, 1193–1207 (2023). https://doi.org/10.1007/s11095-022-03316-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-022-03316-9