Abstract
Purpose
To develop a new lipid-based particle formulation platform for respiratory drug delivery applications. To find processing conditions for high surface rugosity and manufacturability. To assess the applicability of the new formulation method to different lipids.
Methods
A new spray drying method with a simplified aqueous suspension feedstock preparation process was developed for the manufacture of rugose lipid particles of 1,2-distearoyl-sn-glycero-3-phosphocholine (DSPC). A study covering a wide range of feedstock temperatures and outlet temperatures was conducted to optimize the processing conditions. Aerosol performance was characterized in vitro and in silico to assess the feasibility of their use in respiratory drug delivery applications. The applicability of the new spray drying method to longer-chain phospholipids with adjusted spray drying temperatures was also evaluated.
Results
Highly rugose DSPC lipid particles were produced via spray drying with good manufacturability. A feedstock temperature close to, and an outlet temperature lower than, the main phase transition were identified as critical in producing particles with highly rugose surface features. High emitted dose and total lung dose showed promising aerosol performance of the produced particles for use as a drug loading platform for respiratory drug delivery. Two types of longer-chain lipid particles with higher main phase transition temperatures, 1,2-diarachidoyl-sn-glycero-3-phosphocholine (DAPC) and 1,2-dibehenoyl-sn-glycero-3-phosphocholine (22:0 PC), yielded similar rugose morphologies when spray dried at correspondingly higher processing temperatures.
Conclusions
Rugose lipid particles produced via spray drying from an aqueous suspension feedstock are promising as a formulation platform for respiratory drug delivery applications. The new technique can potentially produce rugose particles using various other lipids.








Similar content being viewed by others
References
Patton JS, Byron PR. Inhaling medicines: delivering drugs to the body through the lungs. Nat Rev Drug Discov. 2007;6(1):67–74. https://doi.org/10.1038/nrd2153.
Sanders M. Inhalation therapy: an historical review. Prim Care Respir J. 2007;16(2):71–81. https://doi.org/10.3132/pcrj.2007.00017.
Ibrahim M, Verma R, Garcia-Contreras L. Inhalation drug delivery devices: technology update. Med Devices (Auckl). 2015;8:131. https://doi.org/10.2147/MDER.S48888.
Le Brun P, De Boer A, Frijlink H, Heijerman H. A review of the technical aspects of drug nebulization. Pharm World Sci. 2000;22(3):75–81. https://doi.org/10.1023/A:1008786600530.
Myrdal PB, Sheth P, Stein SW. Advances in metered dose inhaler technology: formulation development. AAPS PharmSciTech. 2014;15(2):434–55. https://doi.org/10.1208/s12249-013-0063-x.
Stein SW, Sheth P, Hodson PD, Myrdal PB. Advances in metered dose inhaler technology: hardware development. AAPS PharmSciTech. 2014;15(2):326–38. https://doi.org/10.1208/s12249-013-0062-y.
Chougule MB, Padhi BK, Jinturkar KA, Misra A. Development of dry powder inhalers. Recent Pat Drug Deliv Formul. 2007;1(1):11–21. https://doi.org/10.2174/187221107779814159.
Frijlink H, De Boer A. Dry powder inhalers for pulmonary drug delivery. Expert Opin Drug Deliv. 2004;1(1):67–86. https://doi.org/10.1517/17425247.1.1.67.
de Boer AH, Hagedoorn P, Hoppentocht M, Buttini F, Grasmeijer F, Frijlink HW. Dry powder inhalation: past, present and future. Expert Opin Drug Deliv. 2017;14(4):499–512. https://doi.org/10.1080/17425247.2016.1224846.
Chan JGY, Wong J, Zhou QT, Leung SSY, Chan H-K. Advances in device and formulation technologies for pulmonary drug delivery. AAPS PharmSciTech. 2014;15(4):882–97. https://doi.org/10.1208/s12249-014-0114-y.
Telko MJ, Hickey AJ. Dry powder inhaler formulation. Respir Care. 2005;50(9):1209–27.
Weers JG, Miller DP. Formulation design of dry powders for inhalation. J Pharm Sci. 2015;104(10):3259–88. https://doi.org/10.1002/jps.24574.
Vehring R. Pharmaceutical particle engineering via spray drying. Pharm Res. 2008;25(5):999–1022. https://doi.org/10.1007/s11095-007-9475-1.
Pilcer G, Amighi K. Formulation strategy and use of excipients in pulmonary drug delivery. Int J Pharm. 2010;392(1–2):1–19. https://doi.org/10.1016/j.ijpharm.2010.03.017.
Hamishehkar H, Rahimpour Y, Javadzadeh Y. The role of carrier in dry powder inhaler. In: Sezer AD, editor. Recent advances in novel drug carrier systems. Rijeka: InTech; 2012. p. 39–66. https://doi.org/10.5772/51209.
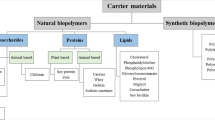
Zillen D, Beugeling M, Hinrichs WL, Frijlink HW, Grasmeijer F. Natural and bioinspired excipients for dry powder inhalation formulations. Curr Opin colloid. Interface Sci. 2021;101497. https://doi.org/10.1016/j.cocis.2021.101497.
Fröhlich E, Salar-Behzadi S. Oral inhalation for delivery of proteins and peptides to the lungs. Eur J Pharm Biopharm. 2021;163:198–211. https://doi.org/10.1016/j.ejpb.2021.04.003.
Pilcer G, Wauthoz N, Amighi K. Lactose characteristics and the generation of the aerosol. Adv Drug Del Rev. 2012;64(3):233–56. https://doi.org/10.1016/j.addr.2011.05.003.
Chang RYK, Chow MY, Khanal D, Chen D, Chan H-K. Dry powder pharmaceutical biologics for inhalation therapy. Adv Drug Del Rev. 2021. https://doi.org/10.1016/j.addr.2021.02.017.
Ngan CL, Asmawi AA. Lipid-based pulmonary delivery system: a review and future considerations of formulation strategies and limitations. Drug Deliv Transl Res. 2018;8(5):1527–44. https://doi.org/10.1007/s13346-018-0550-4.
Li J, Wang X, Zhang T, Wang C, Huang Z, Luo X, Deng Y. A review on phospholipids and their main applications in drug delivery systems. Asian J Pharm Sci. 2015;10(2):81–98. https://doi.org/10.1016/j.ajps.2014.09.004.
Cipolla D, Shekunov B, Blanchard J, Hickey A. Lipid-based carriers for pulmonary products: preclinical development and case studies in humans. Adv Drug Del Rev. 2014;75:53–80. https://doi.org/10.1016/j.addr.2014.05.001.
Scalia S, Young PM, Traini D. Solid lipid microparticles as an approach to drug delivery. Expert Opin Drug Deliv. 2015;12(4):583–99. https://doi.org/10.1517/17425247.2015.980812.
Jaspart S, Piel G, Delattre L, Evrard B. Solid lipid microparticles: formulation, preparation, characterisation, drug release and applications. Expert Opin Drug Deliv. 2005;2(1):75–87. https://doi.org/10.1517/17425247.2.1.75.
Vanbever R, Mintzes JD, Wang J, Nice J, Chen D, Batycky R, Langer R, Edwards DA. Formulation and physical characterization of large porous particles for inhalation. Pharm Res. 1999;16(11):1735–42. https://doi.org/10.1023/A:1018910200420.
Bosquillon C, Lombry C, Preat V, Vanbever R. Influence of formulation excipients and physical characteristics of inhalation dry powders on their aerosolization performance. J Control Release. 2001;70(3):329–39. https://doi.org/10.1016/S0168-3659(00)00362-X.
Minne A, Boireau H, Horta MJ, Vanbever R. Optimization of the aerosolization properties of an inhalation dry powder based on selection of excipients. Eur J Pharm Biopharm. 2008;70(3):839–44. https://doi.org/10.1016/j.ejpb.2008.06.013.
Pilcer G, Sebti T, Amighi K. Formulation and characterization of lipid-coated tobramycin particles for dry powder inhalation. Pharm Res. 2006;23(5):931–40. https://doi.org/10.1007/s11095-006-9789-4.
Eleftheriadis GK, Akrivou M, Bouropoulos N, Tsibouklis J, Vizirianakis IS, Fatouros DG. Polymer–Lipid microparticles for pulmonary delivery. Langmuir. 2018;34(11):3438–48. https://doi.org/10.1021/acs.langmuir.7b03645.
Shetty N, Hou J, Yanez E, Shur J, Cheng J, Sun CC, Nagapudi K, Narang AS. Effect of lipidic excipients on the particle properties and aerosol performance of high drug load spray dried particles for inhalation. J Pharm Sci. 2021. https://doi.org/10.1016/j.xphs.2021.09.004.
Jaspart S, Bertholet P, Piel G, Dogné J-M, Delattre L, Evrard B. Solid lipid microparticles as a sustained release system for pulmonary drug delivery. Eur J Pharm Biopharm. 2007;65(1):47–56. https://doi.org/10.1016/j.ejpb.2006.07.006.
Scalia S, Salama R, Young P, Traini D. Preparation and in vitro evaluation of salbutamol-loaded lipid microparticles for sustained release pulmonary therapy. J Microencapsul. 2012;29(3):225–33. https://doi.org/10.3109/02652048.2011.646326.
Mezzena M, Scalia S, Young PM, Traini D. Solid lipid budesonide microparticles for controlled release inhalation therapy. AAPS J. 2009;11(4):771–8. https://doi.org/10.1208/s12248-009-9148-6.
Scalia S, Haghi M, Losi V, Trotta V, Young PM, Traini D. Quercetin solid lipid microparticles: a flavonoid for inhalation lung delivery. Eur J Pharm Sci. 2013;49(2):278–85. https://doi.org/10.1016/j.ejps.2013.03.009.
Maretti E, Rossi T, Bondi M, Croce MA, Hanuskova M, Leo E, Sacchetti F, Iannuccelli V. Inhaled solid lipid microparticles to target alveolar macrophages for tuberculosis. Int J Pharm. 2014;462(1–2):74–82. https://doi.org/10.1016/j.ijpharm.2013.12.034.
Weers J, Tarara T. The PulmoSphere™ platform for pulmonary drug delivery. Ther Deliv. 2014;5(3):277–95. https://doi.org/10.4155/tde.14.3.
Weers JG, Miller DP, Tarara TE. Spray-dried PulmoSphere™ formulations for inhalation comprising crystalline drug particles. AAPS PharmSciTech. 2019;20(3). https://doi.org/10.1208/s12249-018-1280-0.
Geller DE, Weers J, Heuerding S. Development of an inhaled dry-powder formulation of tobramycin using PulmoSphere™ technology. J Aerosol Med Pulm Drug Deliv. 2011;24(4):175–82. https://doi.org/10.1089/jamp.2010.0855.
Miller DP, Tan T, Tarara TE, Nakamura J, Malcolmson RJ, Weers JG. Physical characterization of tobramycin inhalation powder: I. rational design of a stable engineered-particle formulation for delivery to the lungs. Mol Pharm. 2015;12(8):2582–93. https://doi.org/10.1021/acs.molpharmaceut.5b00147.
Tarara TE, Hartman MS, Gill H, Kennedy AA, Weers JG. Characterization of suspension-based metered dose inhaler formulations composed of spray-dried budesonide microcrystals dispersed in HFA-134a. Pharm Res. 2004;21(9):1607–14. https://doi.org/10.1023/B:PHAM.0000041455.13980.f1.
Vehring R, Lechuga-Ballesteros D, Joshi V, Noga B, Dwivedi SK. Cosuspensions of microcrystals and engineered microparticles for uniform and efficient delivery of respiratory therapeutics from pressurized metered dose inhalers. Langmuir. 2012;28(42):15015–23. https://doi.org/10.1021/la302281n.
Fisher AB. Lung lipid composition and surfactant biology. In: Parent RA, editor. Comparative biology of the normal lung: Academic Press; 2015. p. 423–66. https://doi.org/10.1016/B978-0-12-404577-4.00022-9.
Praphawatvet T, Peters JI, Williams RO III. Inhaled nanoparticles - an updated review. Int J Pharm. 2020;119671. https://doi.org/10.1016/j.ijpharm.2020.119671.
D’Sa D, Williams L, Speck J, Dwivedi S, Lechuga D. Thermodynamic and structural effects of CaCl2 on the phase transitions and structures of Distearoyl-phosphatidylcholine (DSPC) by differential scanning calorimetry and X-ray diffraction. In.AAPS Annual Meeting and Exposition. Washington, DC, US; 2011.
Corzo C, Fuchsbichler A, Savencu I, Urich JA, Zimmer A, Lochmann D, Reyer S, Salar-Behzadi S. Lipid-microparticles for pulmonary delivery of active pharmaceutical ingredients: impact of lipid crystallization on spray-drying processability. Int J Pharm. 2021;121259. https://doi.org/10.1016/j.ijpharm.2021.121259.
Koynova R, Caffrey M. Phases and phase transitions of the phosphatidylcholines. Biochimica et Biophysica Acta (BBA)-reviews on. Biomembranes. 1998;1376(1):91–145. https://doi.org/10.1016/S0304-4157(98)00006-9.
Marsh D. Handbook of lipid bilayers, 2nd Edition: CRC press; 2013. https://doi.org/10.1201/b11712.
Janiak MJ, Small DM, Shipley GG. Temperature and compositional dependence of the structure of hydrated dimyristoyl lecithin. J Biol Chem. 1979;254(13):6068–78. https://doi.org/10.1016/S0021-9258(18)50520-2.
Marsh D. General features of phospholipid phase transitions. Chem Phys Lipids. 1991;57(2):109–20. https://doi.org/10.1016/0009-3084(91)90071-I.
Szoka F Jr, Papahadjopoulos D. Comparative properties and methods of preparation of lipid vesicles (liposomes). Annu Rev Biophys Bioeng. 1980;9(1):467–508. https://doi.org/10.1146/annurev.bb.09.060180.002343.
Ivey J. Particle formation from evaporating microdroplets for inhaled drug delivery. In. Mechanical engineering. Edmonton, Alberta: University of Alberta; 2018. https://doi.org/10.7939/R3RB6WJ3S.
Hoe S, Ivey JW, Boraey MA, Shamsaddini-Shahrbabak A, Javaheri E, Matinkhoo S, Finlay WH, Vehring R. Use of a fundamental approach to spray-drying formulation design to facilitate the development of multi-component dry powder aerosols for respiratory drug delivery. Pharm Res. 2014;31(2):449–65. https://doi.org/10.1007/s11095-013-1174-5.
Carrigy NB, Liang L, Wang H, Kariuki S, Nagel TE, Connerton IF, Vehring R. Trileucine and pullulan improve anti-Campylobacter bacteriophage stability in engineered spray-dried microparticles. Ann Biomed Eng. 2019. https://doi.org/10.1007/s10439-019-02435-6.
Wang H, Bhambri P, Ivey J, Vehring R. Design and pharmaceutical applications of a low-flow-rate single-nozzle impactor. Int J Pharm. 2017;533(1):14–25. https://doi.org/10.1016/j.ijpharm.2017.09.047.
Rouquerol F, Rouquerol J, Sing KS, Llewellyn P, Maurin G. Adsorption by powders and porous solids: principles, Methodology and applications: Academic press; 2014. https://doi.org/10.1016/B978-0-08-097035-6.00007-3.
Carrigy NB, Ordoubadi M, Liu Y, Melhem O, Barona D, Wang H, Milburn L, Ruzycki CA, Finlay WH, Vehring R. Amorphous pullulan trehalose microparticle platform for respiratory delivery. Int J Pharm. 2019;563:156–68. https://doi.org/10.1016/j.ijpharm.2019.04.004.
Pharmacopeia US. <601> Aerosols, nasal sprays, metered dose inhalers, and dry powder inhalers. Rockville: In.US Pharmacopeial Convention; 2012.
Javaheri E, Shemirani FM, Pichelin M, Katz IM, Caillibotte G, Vehring R, Finlay WH. Deposition modeling of hygroscopic saline aerosols in the human respiratory tract: comparison between air and helium–oxygen as carrier gases. J Aerosol Sci. 2013;64:81–93. https://doi.org/10.1016/j.jaerosci.2013.04.010.
Ruzycki CA, Murphy B, Nathoo H, Finlay WH, Martin AR. Combined in vitro-in silico approach to predict deposition and pharmacokinetics of budesonide dry powder inhalers. Pharm Res. 2020;37(10):1–19. https://doi.org/10.1007/s11095-020-02924-7.
Tavernini S, Farina DJ, Martin AR, Finlay WH. Using filters to estimate regional lung deposition with dry powder inhalers. Pharm Res. 2021;38(9):1601–13. https://doi.org/10.1007/s11095-021-03082-0.
Vierros S, Sammalkorpi M. Phosphatidylcholine reverse micelles on the wrong track in molecular dynamics simulations of phospholipids in an organic solvent. J Chem Phys. 2015;142(9):094902. https://doi.org/10.1063/1.4914022.
Pichot R, Watson RL, Norton IT. Phospholipids at the interface: current trends and challenges. Int J Mol Sci. 2013;14(6):11767–94. https://doi.org/10.3390/ijms140611767.
Wang H, Nobes DS, Vehring R. Particle surface roughness improves colloidal stability of pressurized pharmaceutical suspensions. Pharm Res. 2019;36(3):43. https://doi.org/10.1007/s11095-019-2572-0.
Baldelli A, Vehring R. Analysis of cohesion forces between monodisperse microparticles with rough surfaces. Colloids Surf Physicochem Eng Aspects. 2016;506:179–89. https://doi.org/10.1016/j.colsurfa.2016.06.009.
Vehring R, Foss WR, Lechuga-Ballesteros D. Particle formation in spray drying. J Aerosol Sci. 2007;38(7):728–46. https://doi.org/10.1016/j.jaerosci.2007.04.005.
Wang H, Tan P, Barona D, Li G, Hoe S, Lechuga-Ballesteros D, Nobes DS, Vehring R. Characterization of the suspension stability of pharmaceuticals using a shadowgraphic imaging method. Int J Pharm. 2018;548(1):128–38. https://doi.org/10.1016/j.ijpharm.2018.06.053.
Dellamary LA, Tarara TE, Smith DJ, Woelk CH, Adractas A, Costello ML, Gill H, Weers JG. Hollow porous particles in metered dose inhalers. Pharm Res. 2000;17(2):168–74. https://doi.org/10.1023/A:1007513213292.
Lechuga-Ballesteros D, Vehring R, Dwivedi S. A new co-suspension MDI platform: scientific foundations of mono, dual and triple combination products. In Respiratory Drug Delivery Europe. 2011:101–12.
Adi S, Adi H, Chan H-K, Tong Z, Yang R, Yu A. Effects of mechanical impaction on aerosol performance of particles with different surface roughness. Powder Technol. 2013;236:164–70. https://doi.org/10.1016/j.powtec.2012.02.051.
Newman S, Busse W. Evolution of dry powder inhaler design, formulation, and performance. Respir Med. 2002;96(5):293–304. https://doi.org/10.1053/rmed.2001.1276.
Borgström L, Olsson B, Thorsson L. Degree of throat deposition can explain the variability in lung deposition of inhaled drugs. J Aerosol Med. 2006;19(4):473–83. https://doi.org/10.1089/jam.2006.19.473.
Clark AR, Weers JG, Dhand R. The confusing world of dry powder inhalers: it is all about inspiratory pressures, not inspiratory flow rates. J Aerosol Med Pulm Drug Deliv. 2020;33(1):1–11. https://doi.org/10.1089/jamp.2019.1556.
Ung KT, Chan H-K. Effects of ramp-up of inspired airflow on in vitro aerosol dose delivery performance for certain dry powder inhalers. Eur J Pharm Sci. 2016;84:46–54. https://doi.org/10.1016/j.ejps.2016.01.005.
Acknowledgments and Disclosures
The authors acknowledge the language editing provided by Luba Slabyj. PC, KL, NC, DLB are employees of AstraZeneca and may own stock or stock options. The authors declare no conflict of interest.
Funding
This work was supported by the Natural Sciences and Engineering Research Council of Canada through its Collaborative Research & Development program (Grant CRDPJ 543336–19).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, H., Ordoubadi, M., Connaughton, P. et al. Spray Dried Rugose Lipid Particle Platform for Respiratory Drug Delivery. Pharm Res 39, 805–823 (2022). https://doi.org/10.1007/s11095-022-03242-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-022-03242-w