Abstract
Purpose
The present study aimed to elucidate the transport properties of imipramine and paroxetine, which are the antidepressants, across the blood-brain barrier (BBB) in rats.
Methods
In vivo influx and efflux transport of imipramine and paroxetine across the BBB were tested using integration plot analysis and a combination of brain efflux index and brain slice uptake studies, respectively. Conditionally immortalized rat brain capillary endothelial cells, TR-BBB13 cells, were utilized to characterize imipramine and paroxetine transport at the BBB in vitro.
Results
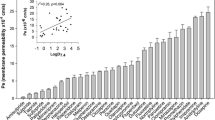
The in vivo influx clearance of [3H]imipramine and [3H]paroxetine in rats was determined to be 0.322 mL/(min·g brain) and 0.313 mL/(min·g brain), respectively. The efflux clearance of [3H]imipramine and [3H]paroxetine was 0.380 mL/(min·g brain) and 0.126 mL/(min·g brain), respectively. These results suggest that the net flux of paroxetine, but not imipramine, at the BBB in vivo was dominated by transport to the brain from the circulating blood. The uptake of imipramine and paroxetine by TR-BBB13 cells exhibited time- and temperature-dependence and one-saturable kinetics with a Km of 37.6 μM and 89.2 μM, respectively. In vitro uptake analyses of extracellular ion dependency and the effect of substrates/inhibitors for organic cation transporters and transport systems revealed minor contributions to known transporters and transport systems and the difference in transport properties in the BBB between imipramine and paroxetine.
Conclusions
Our study showed the comprehensive outcomes of imipramine and paroxetine transport at the BBB, implying that molecular mechanism(s) distinct from previously reported transporters and transport systems are involved in the transport.








Similar content being viewed by others
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- aCSF:
-
artificial cerebrospinal fluid
- AUC(t):
-
Area under the plasma concentration time curve from time 0 to t
- BBB:
-
Blood-brain barrier
- BEI:
-
Brain efflux index
- CEF:
-
Cerebral extracellular fluid
- CL eff,BBB :
-
Efflux clearance across the BBB
- CL inf,brain :
-
Apparent influx clearance of the drug into the brain
- Cp(t):
-
Plasma concentration at time t
- HEPES:
-
2-[4-(2-hydroxyethyl)-1-piperazinyl]ethansulfonic acid
- k eff,BBB :
-
Elimination rate constant from the brain across the BBB
- K m :
-
Michaelis-Menten constant
- K p,app,brain :
-
Apparent brain-to-plasma concentration ratio
- LTR:
-
LysoTracker® Red
- MATE1:
-
Multidrug and toxin extrusion protein 1
- MPP+ :
-
1-methyl-4-phenyl pyridinium
- N.E.:
-
Not examined
- OCT:
-
Organic cation transporter
- OCTN:
-
Organic cation/L-carnitine transporter
- PMAT:
-
Plasma membrane monoamine transporter
- SD:
-
Standard deviation
- SERT:
-
Serotonin transporter
- SLC:
-
Solute carrier
- TEA:
-
Tetraetylammonium
- V d,brain :
-
Cerebral distribution volume of the drug
- V i,brain :
-
Rapidly-equilibrated cerebral distribution volume
- V max :
-
Maximum uptake rate
References
Schildkraut JJ. The catecholamine hypothesis of affective disorders: a review of supporting evidence. Am J Psychiatry. 1965;122(5):509–22.
Arroll B, Elley CR, Fishman T, Goodyear-Smith FA, Kenealy T, Blashki G, Kerse N, Macgillivray S. Antidepressants versus placebo for depression in primary care. Cochrane Database Syst Rev. 2009;3:CD007954.
Baghai TC, Blier P, Baldwin DS, Bauer M, Goodwin GM, Fountoulakis KN, Kasper S, Leonard BE, Malt UF, Stein DJ, Versiani M, Moller HJ. Executive summary of the report by the WPA section on pharmacopsychiatry on general and comparative efficacy and effectiveness of antidepressants in the acute treatment of depressive disorders. Eur Arch Psychiatry Clin Neurosci. 2012;262(1):13–22.
Al-Harbi KS. Treatment-resistant depression: therapeutic trends, challenges, and future directions. Patient Prefer Adherence. 2012;6:369–88.
Rush AJ, Trivedi MH, Wisniewski SR, Nierenberg AA, Stewart JW, Warden D, Niederehe G, Thase ME, Lavori PW, Lebowitz BD, McGrath PJ, Rosenbaum JF, Sackeim HA, Kupfer DJ, Luther J, Fava M. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry. 2006;163(11):1905–17.
Hall H, Ogren SO. Effects of antidepressant drugs on histamine-H1 receptors in the brain. Life Sci. 1984;34(6):597–605.
Stanton T, Bolden-Watson C, Cusack B, Richelson E. Antagonism of the five cloned human muscarinic cholinergic receptors expressed in CHO-K1 cells by antidepressants and antihistaminics. Biochem Pharmacol. 1993;45(11):2352–4.
Sanchez C, Reines EH, Montgomery SA. A comparative review of escitalopram, paroxetine, and sertraline: are they all alike? Int Clin Psychopharmacol. 2014;29(4):185–96.
Richelson E. Pharmacology of antidepressants. Mayo Clin Proc. 2001;76(5):511–27.
Kaplan EM. Efficacy of venlafaxine in patients with major depressive disorder who have unsustained or no response to selective serotonin reuptake inhibitors: an open-label, uncontrolled study. Clin Ther. 2002;24(7):1194–200.
Ohtsuki S, Terasaki T. Contribution of carrier-mediated transport systems to the blood-brain barrier as a supporting and protecting interface for the brain; importance for CNS drug discovery and development. Pharm Res. 2007;24(9):1745–58.
Berner B, Wilson DR, Steffens RJ, Mazzenga GC, Hinz R, Guy RH, Maibach HI. The relationship between pKa and skin irritation for a series of basic penetrants in man. Fundam Appl Toxicol. 1990;15(4):760–6.
Bjørhovde A, Halvorsen TG, Rasmussen KE, Pedersen-Bjergaard S. Liquid-phase microextraction of drugs from human breast milk. Anal Chim Acta. 2003;491(2):155–61.
Tsuda M, Terada T, Asaka J, Ueba M, Katsura T, Inui K. Oppositely directed H+ gradient functions as a driving force of rat H+/organic cation antiporter MATE1. Am J Physiol Renal Physiol. 2007;292(2):F593–8.
Wang M, Sun Y, Hu B, He Z, Chen S, Qi D. An H, Wei Y. Curr Drug Deliv: Organic cation transporters are involved in fluoxetine transport across the blood-brain barrier in vivo and in vitro; 2021.
Okura T, Kato S, Deguchi Y. Functional expression of organic cation/carnitine transporter 2 (OCTN2/SLC22A5) in human brain capillary endothelial cell line hCMEC/D3, a human blood-brain barrier model. Drug Metab Pharmacokinet. 2014;29(1):69–74.
Okura T, Kato S, Takano Y, Sato T, Yamashita A, Morimoto R, Ohtsuki S, Terasaki T, Deguchi Y. Functional characterization of rat plasma membrane monoamine transporter in the blood-brain and blood-cerebrospinal fluid barriers. J Pharm Sci. 2011;100(9):3924–38.
Okura T, Hattori A, Takano Y, Sato T, Hammarlund-Udenaes M, Terasaki T, Deguchi Y. Involvement of the pyrilamine transporter, a putative organic cation transporter, in blood-brain barrier transport of oxycodone. Drug Metab Dispos. 2008;36(10):2005–13.
Tega Y, Akanuma S, Kubo Y, Terasaki T, Hosoya K. Blood-to-brain influx transport of nicotine at the rat blood-brain barrier: involvement of a pyrilamine-sensitive organic cation transport process. Neurochem Int. 2013;62(2):173–81.
Yamazaki M, Fukuoka H, Nagata O, Kato H, Ito Y, Terasaki T, Tsuji A. Transport mechanism of an H1-antagonist at the blood-brain barrier: transport mechanism of mepyramine using the carotid injection technique. Biol Pharm Bull. 1994;17(5):676–9.
Daniel WA, Wojcikowski J. Lysosomal trapping as an important mechanism involved in the cellular distribution of perazine and in pharmacokinetic interaction with antidepressants. Eur Neuropsychopharmacol. 1999;9(6):483–91.
Schmitt MV, Lienau P, Fricker G, Reichel A. Quantitation of lysosomal trapping of basic lipophilic compounds using in vitro assays and in silico predictions based on the determination of the full pH profile of the endo−/lysosomal system in rat hepatocytes. Drug Metab Dispos. 2019;47(1):49–57.
Kakee A, Terasaki T, Sugiyama Y. Brain efflux index as a novel method of analyzing efflux transport at the blood-brain barrier. J Pharmacol Exp Ther. 1996;277(3):1550–9.
Hosoya KI, Takashima T, Tetsuka K, Nagura T, Ohtsuki S, Takanaga H, Ueda M, Yanai N, Obinata M, Terasaki T. mRna expression and transport characterization of conditionally immortalized rat brain capillary endothelial cell lines; a new in vitro BBB model for drug targeting. J Drug Target. 2000;8(6):357–70.
Flecknell P. Replacement, reduction and refinement. ALTEX. 2002;19(2):73–8.
Tega Y, Tabata H, Kurosawa T, Kitamura A, Itagaki F, Oshitari T, Deguchi Y. Structural requirements for uptake of diphenhydramine analogs into hCMEC/D3 cells via the proton-coupled organic cation antiporter. J Pharm Sci. 2021;110(1):397–403.
Yamaoka K, Tanigawara Y, Nakagawa T, Uno T. A pharmacokinetic analysis program (multi) for microcomputer. Aust J Pharm. 1981;4(11):879–85.
Kawase A, Chuma T, Irie K, Kazaoka A, Kakuno A, Matsuda N, Shimada H, Iwaki M. Increased penetration of diphenhydramine in brain via proton-coupled organic cation antiporter in rats with lipopolysaccharide-induced inflammation. Brain Behav Immun Health. 2021;10:100188.
Wu KC, Lu YH, Peng YH, Hsu LC, Lin CJ. Effects of lipopolysaccharide on the expression of plasma membrane monoamine transporter (PMAT) at the blood-brain barrier and its implications to the transport of neurotoxins. J Neurochem. 2015;135(6):1178–88.
Kekuda R, Prasad PD, Wu X, Wang H, Fei YJ, Leibach FH, Ganapathy V. Cloning and functional characterization of a potential-sensitive, polyspecific organic cation transporter (OCT3) most abundantly expressed in placenta. J Biol Chem. 1998;273(26):15971–9.
Terada T, Masuda S, Asaka J, Tsuda M, Katsura T, Inui K. Molecular cloning, functional characterization and tissue distribution of rat H+/organic cation antiporter MATE1. Pharm Res. 2006;23(8):1696–701.
Urakami Y, Okuda M, Masuda S, Saito H, Inui KI. Functional characteristics and membrane localization of rat multispecific organic cation transporters, OCT1 and OCT2, mediating tubular secretion of cationic drugs. J Pharmacol Exp Ther. 1998;287(2):800–5.
Wu X, George RL, Huang W, Wang H, Conway SJ, Leibach FH, Ganapathy V. Structural and functional characteristics and tissue distribution pattern of rat OCTN1, an organic cation transporter, cloned from placenta. Biochim Biophys Acta. 2000;1466(1–2):315–27.
Wu X, Huang W, Prasad PD, Seth P, Rajan DP, Leibach FH, Chen J, Conway SJ, Ganapathy V. Functional characteristics and tissue distribution pattern of organic cation transporter 2 (OCTN2), an organic cation/carnitine transporter. J Pharmacol Exp Ther. 1999;290(3):1482–92.
VanWert AL, Gionfriddo MR, Sweet DH. Organic anion transporters: discovery, pharmacology, regulation and roles in pathophysiology. Biopharm Drug Dispos. 2010;31(1):1–71.
Wakayama K, Ohtsuki S, Takanaga H, Hosoya K, Terasaki T. Localization of norepinephrine and serotonin transporter in mouse brain capillary endothelial cells. Neurosci Res. 2002;44(2):173–80.
Tachikawa M, Takeda Y, Tomi M, Hosoya K. Involvement of OCTN2 in the transport of acetyl-L-carnitine across the inner blood-retinal barrier. Invest Ophthalmol Vis Sci. 2010;51(1):430–6.
Hammarlund-Udenaes M, Friden M, Syvanen S, Gupta A. On the rate and extent of drug delivery to the brain. Pharm Res. 2008;25(8):1737–50.
Nagy A, Johansson R. The demethylation of imipramine and clomipramine as apparent from their plasma kinetics. Psychopharmacology. 1977;54(2):125–31.
Sallee FR, Pollock BG. Clinical pharmacokinetics of imipramine and desipramine. Clin Pharmacokinet. 1990;18(5):346–64.
Ohtsuki S, Sato S, Yamaguchi H, Kamoi M, Asashima T, Terasaki T. Exogenous expression of claudin-5 induces barrier properties in cultured rat brain capillary endothelial cells. J Cell Physiol. 2007;210(1):81–6.
Takanaga H, Tokuda N, Ohtsuki S, Hosoya K, Terasaki T. ATA2 is predominantly expressed as system a at the blood-brain barrier and acts as brain-to-blood efflux transport for L-proline. Mol Pharmacol. 2002;61(6):1289–96.
Kocsis JH, Hanin I, Bowden C, Brunswick D. Imipramine and amitriptyline plasma concentrations and clinical response in major depression. Br J Psychiatry. 1986;148:52–7.
DeVane CL. Differential pharmacology of newer antidepressants. J Clin Psychiatry. 1998;59(Suppl 20):85–93.
Shinozaki Y, Akanuma SI, Mori Y, Kubo Y, Hosoya KI. Comprehensive evidence of carrier-mediated distribution of amantadine to the retina across the blood-retinal barrier in rats. Pharmaceutics. 2021;13(9).
Grundemann D, Liebich G, Kiefer N, Koster S, Schomig E. Selective substrates for non-neuronal monoamine transporters. Mol Pharmacol. 1999;56(1):1–10.
Andre P, Debray M, Scherrmann JM, Cisternino S. Clonidine transport at the mouse blood-brain barrier by a new H+ antiporter that interacts with addictive drugs. J Cereb Blood Flow Metab. 2009;29(7):1293–304.
Kubo Y, Shimizu Y, Kusagawa Y, Akanuma S, Hosoya K. Propranolol transport across the inner blood-retinal barrier: potential involvement of a novel organic cation transporter. J Pharm Sci. 2013;102(9):3332–42.
Kubo Y, Yamada M, Konakawa S, Akanuma SI, Hosoya KI. Uptake study in lysosome-enriched fraction: critical involvement of lysosomal trapping in quinacrine uptake but not fluorescence-labeled verapamil transport at blood-retinal barrier. Pharmaceutics. 2020;12(8):747.
Kubo Y, Seko N, Usui T, Akanuma S, Hosoya K. Lysosomal trapping is present in retinal capillary endothelial cells: insight into its influence on cationic drug transport at the inner blood-retinal barrier. Biol Pharm Bull. 2016;39(8):1319–24.
Anderson IM. Selective serotonin reuptake inhibitors versus tricyclic antidepressants: a meta-analysis of efficacy and tolerability. J Affect Disord. 2000;58(1):19–36.
ACKNOWLEDGMENTS AND DISCLOSURES
The authors thank Mr. Ryuta Jomura (University of Toyama, Toyama, Japan) for supporting the in vivo studies. The authors declare that they have no conflicts of interest.
Funding
This research was supported by the Japan Society for the Promotion of Science (JSPS) KAKENHI [Grant Numbers: 19K07160 to Shin-ichi Akanuma and 20H03403 to Ken-ichi Hosoya] and the Research Grant from the Smoking Research Foundation.
Author information
Authors and Affiliations
Contributions
S.A., M.H., and Y.M. performed the experiments and analyzed the data; S.A., Y.K., and H.K. designed the experiments; S.A. and K.H. wrote the manuscript. All the authors have read the final version of the manuscript.
Corresponding authors
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Akanuma, Si., Han, M., Murayama, Y. et al. Differences in Cerebral Distribution between Imipramine and Paroxetine via Membrane Transporters at the Rat Blood-Brain Barrier. Pharm Res 39, 223–237 (2022). https://doi.org/10.1007/s11095-022-03179-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-022-03179-0